![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
127 Cards in this Set
- Front
- Back
|
What is the definition of coagulation?
|
A cascade process by which soluble fibrinogen is converted to insoluble fibrin in the end.
|
|
|
What part of the blood hold the ability to coagulate?
|
The plasma, not the hematocrit
|
|
|
How is blood kept in liquid form in circulation?
|
Endothelial cells produce products that prevent platelets from sticking to the endothelial cells. They also provide a physical barrier to the collagen in the BM.
|
|
|
What antiplatelet factors do healthy endothelial cells produce?
|
NO, PGI2, and ADP phosphatases
|
|
|
How do these antiplatelet factors work? (NO/PGI2/ADP Phosphatase)
|
They inhibit the binding sites on the platelets.
|
|
|
What is the cell structure of a platelet?
|
It is a membrane bound cell with no nucleus
|
|
|
How long is the lifespan of a platelet?
|
8-10 days
|
|
|
How big is a platelet?
|
2-3 um
|
|
|
How big is a RBC?
|
8-10um
|
|
|
How can you remember this?
|
You can fit about 2-3 platelets in a RBC?
|
|
|
What is the daily role of platelets?
|
to plug up all the micro punctures in our vascular system.
|
|
|
WHat is thrombocytopenia?
|
Low platelet count
|
|
|
What is the clinical manifestation for an uninjured person with thrombocytopenia?
|
micro hemorrhages and pupura all over the body
|
|
|
What antiplatelet/coagulation proteins are present on every healthy endothelial cell?
|
heparin sulfate, thrombomodulin, and t. PA
|
|
|
What does heparin sulfate that is secreted by the endothelial cells do?
|
binds to and activates Antithrombin III
|
|
|
What does antithrombin III do?
|
It cuts down THROMBIN and also the activated factors 9-12 (intrinsic pathway) which will make thrombin.
|
|
|
Why is this advantagerous to healthy cells near a site on injury?
|
It prevents coagulation from happening in non injured sites.
|
|
|
What is the naughty molecule that is also expressed on healthy endothelial cells.
|
Thrombomodulin
|
|
|
What does thrombbomodulin do?
|
It binds thrombin and prevents it from coagulating., which activates protein C.
|
|
|
What does protein C do?
|
It eats up factors 5a and 8a
|
|
|
Draw thrombomodulin process.
|

|
|
|
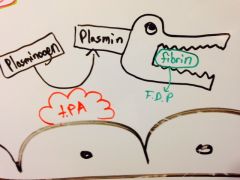
What is the substance produced by healthy endothelial cells that deal with plasminogen?
|
t. PA (tissue plasminogen activator), which is an enzyme that sits on the endothelial cells.
|
|
|
What does t. PA do?
|
It converts plasminogen in the blood to plasmin.
|
|
|
What does plasmin do?
|
It will take fibrin and break it down into fibrin degradation product.
|
|
|
Draw the function of tPA in a normal cell.
|
|
|
|
Name all the normal defense mechanisms to keep blood liquid in the body by HEALTHY endothelial cells.
|
1. Antiplatelet stickiness factors like NO, PGI2, and ADP phosphatase
2. Heparin sulfate 3. Thrombomodulin 4. t.PA |
|
|
What is the goal of your body when the endothelial cells are damaged?
|
To stop the bleeding
|
|
|
What is the order of the three steps to stop bleeding?
|
1. vasoconstriction
2. platelet plug 3. coagulation |
|
|
how does the vasoconsriction occur?
|
1. reflexive neurogenic constriction
2. reflexive myogenic constriction 3. endothelial cells produce endothelin and stop being able to produce anticoagulation stuff. |
|
|
What does endothelin do and when is it released?
|
it is released by damaged endothelial cells and constricts blood vessels.
|
|
|
What anticoagulation things are lost in injured endothelial cells?
|
All of the ones mentioned before are no longer present.
|
|
|
What do damaged endothelial cell secrete?
|
They cry because they are sad and secrete von Willebrand factor.
|
|
|
What does vWF do?
|
It attaches onto the exposed collagen and attracts and binds platelets.
|
|
|
What is on the membrane of platelets that allow them to stick onto vWF?
|
Gp1b (glycoprotein 1b)
|
|
|
What is platelet adhesion?
|
The process by which platelets stick to a surface that has no platelets.
|
|
|
What happens after platelet adhesion?
|
The vWF initiates an intracellular cascade which causes the platelet to start secreting TXA2.
|
|
|
What are the two functions of TXA2?
|
A vasoconstrictor and platelet aggregator.
|
|
|
What does aspirin do to the platelets?
|
It irreverssible acetylates the COX in their membrane so they can't produce TXA2.
|
|
|
What happens to activated platelets?
|
They undergo a release reaction that releases granules.
|
|
|
What are the two types of granules that are released?
|
alpha granules and dense/delta granules
|
|
|
What do the dense/delta granules look like and how can you use this to remember what they secrete?
|
They look like big SACS!
Serotonin ADP Calcium |
|
|
What does serotonin do?
|
Produces vasocontriction
|
|
|
What does ADP do?
|
It increases ADP concentration at the area of injury and that ACTIVATES platelets that are passing by, making their receptors active.
|
|
|
What are some drugs that inhibit ADP activation of platelets?
|
Ticlopidine and Plavix
|
|
|
How can you remember Plavix?
|
PLAtelets = PLAvix
|
|
|
Where are the coagulation factors located?
|
they are located in the blood
|
|
|
What does calcium do?
|
It binds to the negatively charged coagulation factors and fixes them onto the platelet membrane surface.
|
|
|
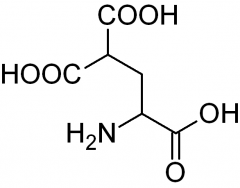
Where does calcium stick onto the coagualtion factors?
|
On carboxyglutamic acid residues. It sticks the coagulation factors together in this way by their COO- which have high calcium affinity.
|
|
|
What does carboxyglutamic acid look like?
|
|
|
|
What makes the post translational modification that leads to gamma carboxylation of glutamic acid?
|
vitamin K in the liver!
|
|
|
Which coagulation factors down vitamin K carboxylate?
|
2, 7, 9, and 10. And protein Z.
|
|
|
What do alpha granules of platelets release? (3)
|
1. coagulation factors (especially 5 and 8)
2. fibrinogen 3. platelet derived growth factor |
|
|
Draw the alpha and delta granules with their products.
|

|
|
|
What are the two main platelet products that attract more platelets to the scene?
|
TXA2 and ADP
|
|
|
What does it mean for platelets to be activated?
|
They secrerte granule products
|
|
|
What is platelet aggregation?
|
When platelets start sticking to one another (not vWF or BM.. that is platelet adherence)
|
|
|
What is the initial platelet plug produced by adherence/degranulation/and aggregation of paltelets called?
|
The primary platelet plug.
|
|
|
Is the primary platelet plug loose or tight?
|
loose
|
|
|
How do you make it tight?
|
Attract a bunch of fibrin fibers to cement it down.
|
|
|
What is the primary platelet plug with fibrin overlying it called?
|
The secondary platelet plug
|
|
|
Is the coagulation of blood in a clean glass tube by the intrinsic or extrinsic pathway?
|
The intrinsic pathway
|
|
|
Why is it called the intrinsic pathway?
|
Because scientists knew the tube was very clean so deducted that it must be due to something intrinsic in the blood that isn't added.
|
|
|
Why is the extrinsic pathway called what it is?
|
it forms when you add "tissue juice" to the blood.
|
|
|
How was the extrinsic pathway discovered?
|
Some sadistic scientist took citrated blood (which removed the intrinsic pathway) and added the "tissue juice" from the brain of a mouse he killed and found coagulation.
|
|
|
What was in the "tissue juice" that turned on coagulation?
|
Thromboplastin. (tissue factor)
|
|
|
What charge is citrate?
|
negatively charge (-ate = COO-)
|
|
|
Why does citrate prevent coagulation?
|
it binds calcium
|
|
|
What is thromboplastin made from and how is it creatied?
|
It is just lipids and lipoproteins from macerated tissued.
|
|
|
How is intrinsic pathway started?
|
When Hageman factor/factor 12 comes into contact with collagen from the BM or damaged endothelial cells or activated platelets.
|
|
|
Draw the intrinsic cascade of coagulation factors.
|

|
|
|
What are the cofactor coagulation factors and what do they always need to work? Why?
|
Factors 8 and 5, which work by binding other coagulation factors to the cell membrane by their carboxyglutamates so they need phospholipids from the cell membrane and calcium
|
|
|
What is the order of factors activated in the intrinsic pathway?
|
12 (hageman) --> 11 --> 9 (presence of PL, Ca, and 8) --> 10 --> Thrombin --> 13 (TSF) and fibrin
|
|
|
Which coagulation factors are involved in intrinsic pathway?
|
Factors 8-13
|
|
|
How does the extrinsic pathway work?
|
Tissue factor (thromboplastin) activates factor 7, which goes to activate the common pathway 10 and also the intrinsic pathway at factor 9.
|
|
|
What is the trigger for the intrinsic vs extrinsic pathway?
|
Intrinsic- factor 12 comes into contact with collagen
Extrinsic- tissue factor (thromboplastin) comes into contact with factor 7 |
|
|
What gets stuck in the platelet plug besides fibrin and platelets?
|
RBC's and WBC's
|
|
|
What is the whole secondary plug with the platelets, RBC's, WBC's, and fibrin called?
|
A Thrombus!
|
|
|
Why don't you get lower body edema with vasoconstriction?
|
Because edema is due to blood being too volumous for even the veins to handle. The arteries add little to capacitance.
|
|
|
What two cytokines are constantly being balanced in the body for coagulation/anticoagulation signals? (hint: COX)
|
Procoaglation- TXA2
Anticoagulation- PGI2 |
|
|
What does COX-1 inhibit?
|
production of both thromboxanes and prostaglandins
|
|
|
What does COX-2 inhibit?
|
it inhibits more prostaglandins than thromboxanes
|
|
|
What are the benefits of selective COX-2 inhibitors?
|
You don't get the bad side effects of typicals NSAIDs because COX-2 is only in inflammed tissue.
|
|
|
What are the downsides to COX-2 inhibitors?
|
You have an unbalance of TXA2 vs PGI2, which predisposes you to blood clots.
|
|
|
What binds factor 9 and 10 together besides calcium?
|
Factor 8 links them together.
|
|
|
What factor is prothrombin/thrombin?
|
Factor 2
|
|
|
What is heparan sulfate?
|
A glycosamino glycan attached to collagen responsible for the negative charge on basement membranes.
|
|
|
What is heparin sulfate?
|
A membrane bound protein on epithelial cells that binds antithrombin III, which cleave thrombin, factor 9a, and factor 10a.
|
|
|
What does PDGF do?
|
a growth factor for cells and angiogenesis.
|
|
|
What does it mean to have a coagulation?
|
Just to have fibrinogen converted to fibrin.
|
|
|
What does it mean to have a thrombus>
|
To have the platelet plug and the fibrin within the circulatory system
|
|
|
What does it mean to have a clot?
|
To have the platelet plug and the fibrin that can be either inside or outside the circulatory system.
|
|
|
What are the fates of a clot/occluded vessel? (4)
|
1. Break off and become an embolus
2. Dissolve 3. Undergo organization 4. Recanalization |
|
|
How does the clots dissolve?
|
when plasmin created by healthy endothelial cells with t.PA cuts the fibrin down.
|
|
|
How do clots get organized?
|
When fibroblasts are mobilized and lay new collagen over the thrombus
|
|
|
What do the surrounding endothelial cells do when a thrombus has completely occluded the vessel?
|
They proliferate and grow over the thrombus under the influence of platelet derived growth factor, grow in to meet each other, and dissolve the center in order to make a new canal for blood to flow. RECANALIZATION.
|
|
|
What are all the functions of platelet derived growth factor (PDGF)?
|
1. Induce smooth muscle growth
2. Induce fibroblasts to cover thrombus 3. Induce new endothelial growth (angiogenesis) |
|
|
Which COX enzyme created TXA2 in platelets? How can you remember this?
|
COX-1. This is what low doses of aspirin inhibits and COX-2 inhibitos tend to decrease PGI2 more and are being pulled because this causes clots.
|
|
|
So what process does coumadin treatment target?
|
The coagulation cascade (by inhibiting synthesis of factors 2,7, 9, and 10)
|
|
|
So what process does t. PA treatment target?
|
It actually busts the clots because it cuts down fibrin to fibrin degradation product
|
|
|
So what process does aspirin treatment target?
|
It inhibits platelet adhesion and aggregation by inhibiting synthesis of TXA2, which signals platelets to express gp1b to attache to von Willebrand factor.
|
|
|
So is aspirin a clot buster?
|
No. It just prevents the progression of clots.
|
|
|
BEGIN PATHOMA
|
Go
|
|
|
What is the very first action after endothelial damage? How can you remember this?
|
vasoconstriction. Remember this because you tend to immediately clutch an injured site to reduce blood flow so it's important!
|
|
|
What mediates this immediate vasoconstriction?
|
nervous system and endothelin from endothelial cells
|
|
|
Where does vWF come from?
|
Mostly the endothelial cells in the weibel palade bodies and also the alpha granules of the platelets.
|
|
|
What are all the steps in the primary plug formation?
|
1. vasoconstriction
2. binding of platelets to vWF 3. platelet degranulation |
|
|
What does ADP do?
|
It induces platelets to express Gp2b/3a
|
|
|
What does Gp2b3a do?
|
It allows platelets to aggregate to one another when they are linked together with fibrinogen..
|
|
|
What does vWF bind to?
|
subendothelial collagen which includes tissue collagen and BM collagen
|
|
|
What does activating of coagulation require? (3)
|
1. Calcium
2. Phospholipid (from membrane) 2. Activation factors |
|
|
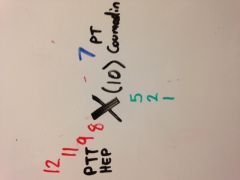
What does PT measure?
|
Measures the extrinsic and common pathways
|
|
|
What does PTT measure?
|
Measures the in trinsic and common pathways
|
|
|
how do you remember which pathway PTT vs PT measure?
|
PTT has more letters and so measures the intrinsic pathway which has more coagulation factors. They both measure the common pathway.
|
|
|
Draw Pathoma's method of memorizing the cascade.
|
|
|
|
What activates factor 12 to start the initial intrinsic cascade?
|
Sub Endothelial Collagen (SEC)
|
|
|
What activates factor 7 to start the initial extrinsic cascade?
|
Tissue Thromboplastin (TT)
|
|
|
how do you remember which pathway has which activator?
|
The activator acronym has the same number of letters as the test. (SEC and PTT, TT and PT)
|
|
|
How do you remember which test measures coumadin and which measures heparin according to pathoma?
|
Heparin is often abbreviated Hep, which also has 3 letters. Also PTT converts to 911, which is used more in emergencies.
|
|
|
What is thrombosis?
|
WHen a thrombus forms that is pathological, not physiological.
|
|
|
What is virchow's triad?
|
The three biggest risk factors for thrombosis.
1. hypercoagulable state 2. disturbed blood flow or blood stasis (activates coagulation factors) 3. endothelial damage |
|
|
What is the biggest cause of venous vs arterial thrombosis?
|
venous- blood stasis
arterial- atherosclerosis |
|
|
How can you tell if a thrombus was formed while the person was still alive?
|
If they have lines of Zahn (alternating layers of fibrin/platelets and RBC's indicating high blood flow dring thrombus formation) and are attached to the vessel wall.
|
|
|
Why would people form clots after they die?
|
the circulatory system is in stasis.
|
|
|
What are the three biggest risk factors for coagulation as a results of blood flow disturbance/stasis?
|
1. Long term immobilization (bedridden or long car ride)
2. Aneurysm 3. Cardiac wall dysfunction (a fib or MI) |
|
|
What happens to GFR in pregnancy?
|
increasez
|
|
|
What happens to GFR in old people?
|
it decreases
|
|
|
Why does iron increase acidosis?
|
too much will detroy you mitochondira, which will force you to use more aneorobic respiration and build up ethanol.
|

