![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
Describe the life cycle of plasmodium and name labeled parts
|
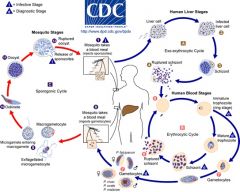
The malaria parasite life cycle involves two hosts. During a blood meal, a malaria-infected female Anopheles mosquito inoculates sporozoites into the human host . Sporozoites infect liver cells and mature into schizonts , which rupture and release merozoites . (Of note, in P. vivax and P. ovale a dormant stage [hypnozoites] can persist in the liver and cause relapses by invading the bloodstream weeks, or even years later.) After this initial replication in the liver (exo-erythrocytic schizogony ), the parasites undergo asexual multiplication in the erythrocytes (erythrocytic schizogony ). Merozoites infect red blood cells . The ring stage trophozoites mature into schizonts, which rupture releasing merozoites . Some parasites differentiate into sexual erythrocytic stages (gametocytes) . Blood stage parasites are responsible for the clinical manifestations of the disease.
The gametocytes, male (microgametocytes) and female (macrogametocytes), are ingested by an Anopheles mosquito during a blood meal . The parasites’ multiplication in the mosquito is known as the sporogonic cycle . While in the mosquito's stomach, the microgametes penetrate the macrogametes generating zygotes . The zygotes in turn become motile and elongated (ookinetes) which invade the midgut wall of the mosquito where they develop into oocysts . The oocysts grow, rupture, and release sporozoites , which make their way to the mosquito's salivary glands. Inoculation of the sporozoites into a new human host perpetuates the malaria life cycle. |
|
|
what is shizogony?
|
Following invasion of a liver cell
the parasite first undergoes a round of asexual replication called merogony, or schizogony, followed by multiple rounds of merogony in the erythrocytes |
|
|
What is another name for schizogony?
|
merogony
|
|
|
What is gametogony and where does it occur?
|
the formation of sexual forms, begins
within the erythrocytes of the vertebrate host and is completed within the mosquito |
|
|
What is sporogony and where does it occur?
|
within the mosquito another round of asexual replication called sporogony takes place
|
|
|
Compare the nomenclature of generalized apicomplexan life cycles to plasmodium
|
- merogony in Plasmodium species is almost always referred to as schizogony
gametogony in Plasmodium is usually separated into two phases called gametocytogenesis and gametogenesis. |
|
|
where do you find sporozoites?
|
Sporozoites are injected with the saliva during mosquito feeding and are
carried to the liver via the circulatory system. Within 30–60 minutes the sporozoites find the liver and invade a liver cell. The sporozoites gain access to the hepatocytes by first invading and traversing a macrophage within the liver called a Kupffer cell. |
|
|
what is an exoerythrocytic schizont
|
(or pre-erythrocytic)
After exiting the Kupffer cell, the sporozoite can traverse several hepatocytes before developing into an exoerythrocytic (or pre-erythrocytic) schizont |
|
|
What is schizogony?
|
Schizogony refers
to an asexual replicative process in which the parasite undergoes multiple rounds of nuclear division without cytoplasmic division followed by a budding, or segmentation |
|
|
When schizogony ends, what does it form? where do you find them?
|
merozoites. The merozoites
are released into the circulatory system following rupture of the host hepatocytes. |
|
|
what is the hypnozoite stage?
What zoite is involved in the hypnozoite stage? |
sporozoites do not immediately
undergo asexual replication, but enter a dormant phase known as the hypnozoite stage. The hypnozoite can reactivate and undergo schizogony at a later time resulting in a relapse. |
|
|
what species can enter the hypnozoite stage?
|
In P. vivax and P. ovale some of the sporozoites do not immediately
undergo asexual replication, but enter a dormant phase known as the hypnozoite stage. |
|
|
describe relapse
|
Relapse has a specific meaning in regard to malaria and refers to the reactivation of the infection via hypnozoites.
|
|
|
describe recrudescence
|
Recrudescence is used to describe the situation in which parasitemia in
the blood falls below detectable levels and then later increases to a patent parasitemia. |
|
|
what zoite invades erythrocytes?
|
Merozoites released from the infected liver cells invade erythrocytes
|
|
|
what is the invasion mechanism?
|
During the invasion process the invasive forms (e.g., merozoites and sporozoites) of most apicomplexan species orientate themselves
so that the apical end is juxtaposed to the host cell. The contents of the rhoptries, micronemes, and dense granules are expelled as the parasite invades. Experiments in Toxoplasma gondii indicate that the micronemes are expelled first and the expulsion occurs with initial contact between the parasite and host. The rhoptries are discharged immediately after the micronemes and dense granule contents are released last. Many dense granules are extruded after the parasite has completed its entry, and thus probably play a role in modifying the host cell. |
|
Describe the invasion mechanism
|
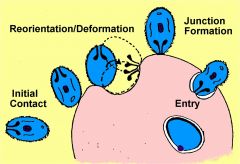
During the invasion process the invasive forms (e.g.,
merozoites and sporozoites) of most apicomplexan species orientate themselves so that the apical end is juxtaposed to the host cell. The contents of the rhoptries, micronemes, and dense granules are expelled as the parasite invades. Experiments in Toxoplasma gondii indicate that the micronemes are expelled first and the expulsion occurs with initial contact between the parasite and host. The rhoptries are discharged immediately after the micronemes and dense granule contents are released last. Many dense granules are extruded after the parasite has completed its entry, and thus probably play a role in modifying the host cell. |
|
|
What is the trophic period
|
intracellular parasite undergoes trophic phase
young trophozoite called ‘ring form’ ingests host hemoglobin - cytostome - food vacuole - hemozoin (malarial pigment) After entering the erythrocyte the parasite undergoes a trophic period followed by an asexual replication. The young trophozoite is often called a ring form due to its morphology in Giemsa-stained blood smears (Figure 15.2). As the parasite increases in size this ring morphology disappears and it is called a trophozoite. During the trophic period the parasite ingests the host cell cytoplasm and breaks down the hemoglobin into amino acids. |
|
|
What is hemozoin?
|
A by-product of the hemoglobin digestion is the malaria pigment, or hemozoin.
golden-brown to black granules |
|
What are th blood stages of a malaria parasite?
|
(A) Ring stage of P. falciparum.
(B) Trophozoite of P. vivax. Note the stippling known as Schüffner’s granules within the infected erythrocyte. (C) Multinucleated schizont stage of P. malariae. |
|
|
What marks the end of the trophozoite stage?
What stage is it now? |
Nuclear division marks the end of the trophozoite stage and the beginning
of the schizont stage. |
|
|
What is erythrocytic schizogony?
|
nuclear division = begin schizont stage
6-40 nuclei budding merozoites = segmenter erythrocyte rupture releases merozoites Erythrocytic schizogony consists of three to five rounds (depending on species) of nuclear replication followed by a budding process. Budding involves the migration of the nuclei and other organelles to the plasma membrane where they are incorporated into the forming merozoite. Late stage schizonts in which the individual merozoites become discernable are called segmenters. The host erythrocyte ruptures and releases the merozoites. |
|
|
What causes the intermittent fever paroxysms?
|
The blood-stage parasites within a host usually undergo a synchronous schizogony resulting in a simultaneous
rupture of the infected erythrocytes and release of merozoites. The concomitant release of antigens and waste products with the rupture of the infected erythrocyte accounts for the intermittent fever paroxysms associated with malaria. |
|
|
what is gametocytogenesis?
|
As an alternative to schizogony some of the parasites will undergo a
sexual cycle and differentiate into either micro- or macrogametocytes. Gametocytes circulate in the peripheral blood stream and are capable of forming gametes if ingested by a mosquito. They do not cause pathology in the human host and will disappear from the circulation if not taken up by a mosquito. The factors involved in the induction of gametocytogenesis are not known. Host immunity and drug treatment may result in a higher proportion of gametocytes as compared with asexual forms. |
|
|
What is gametogenesis?
|
The next step in sexual development is gametogenesis, or the formation
of micro- and macrogametes. After ingestion by the mosquito, the gametocytes escape from the erythrocyte and undergo gametogenesis within the mosquito gut. |
|
|
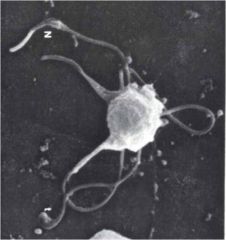
what are microgametes?
|
The microgametocyte
undergoes three rounds of nuclear replication. Then these eight nuclei become associated with flagella that emerge from the body of the microgametocyte to form the microgametes. This process is readily observable by light microscopy due to the thrashing flagella and is called exflagellation. |
|
|
What are macrogametes?
|
the macrogametocytes mature into macrogametes. However, at
the morphological level this is much less dramatic than the exflagellation exhibited by the microgametocytes |
|
|
What is exflagellation?
|
Flagella that emerge from the body of the microgametocyte to form the microgametes. This process is readily observable by light microscopy due to the thrashing flagella and is called exflagellation.
Exflagellation occurs spontaneously when infected blood is exposed to air. |
|
|
What are the critical factors involved in the induction of gametogenesis?
|
Critical factors involved in the induction of this gametogenesis are
1) a decrease in temperature 2) decrease in the dissolved carbon dioxide 3) the subsequent increase in pH to above 8.0 1-3 all occur spontaneously after expoure to air. 4) decrease in pH: a mosquito-derived exflagellation factor also promotes the formation of gametes at a lower pH. |
|
|
What does xanthurenic acid do?
|
mosquito-derived exflagellation factor has been identified as xanthurenic acid, a metabolite from insects.
Xanthurenic acid lowers the permissive pH for exflagellation and is probably a biological cue for the parasite to undergo gametogenesis. |
|
|
Summarize gametogenesis
|
occurs in mosquito gut
‘exflagellation’ most obvious - 3X nuclear replication - 8 microgametes formed one macrogamete exposure to air induces - decreased temperature (2-3oC) - increased pH (8-8.3) - result of decreased pCO2 gametocyte activating factor in mosquito - xanthurenic acid |
|
What am I?
|
Exflagellation
|
|
|
Summarize gametocytogenesis
|
alternative to asexual replication
induction factors not known - drug treatment increase #'s - immune response increases #'s ring --> gametocyte - Pf : ~10 days - others: ~same as schizogony sexual dimorphism - microgametocytes (♂) - macrogametocytes (♀) no pathology no replication infective stage for mosquito |
|
|
Summarize ookinete formation
|
fusion of micro- and macrogametes
zygote --> ookinete (~24 hr) ookinete transverses gut epithelium ('trans-invasion') |
|
|
summarize sporogony
|
summarize sporogony
ookinete --> oocyst between epithelium and basal lamina asexual replication --> sporozoites sporozoites released sporozoites migrate through hemocoel sporozoites 'invade' salivary glands 9-21 days (gametes --> sporozoites) |
|
|
What is an ookinete?
|
gamete fusion (i.e., fertilization), the resulting
zygote develops into an ookinete. The ookinete is a motile and invasive stage which can traverse both the peritrophic membrane and the midgut epithelium of the mosquito. Traversing the peritrophic membrane probably involves secretion of chitinases. Penetration of the midgut epithelium involves invading and exiting several epithelial cells before emerging on the basal side of the epithelium. |
|
|
What is sporogony?
|
After the ookinete reaches the extracellular space between the epithelial cells and the basal lamina, the ookinete develops into an oocyst.
Oocysts undergo an asexual replication, called sporogony, which culminates in the production of several thousand sporozoites. After finding the salivary glands, the sporozoites invade and traverse the salivary gland epithelial cells and come to lie within its lumen. These sporozoites are expelled into the vertebrate host as the mosquito takes a blood meal. |
|
|
What are the three distinct invasive malaria life cycle stages?
|
three distinct invasive stages: sporozoites,
merozoites, and ookinetes. Sporozoites traverse the salivary glands and invade hepatocytes; merozoites invade erythrocytes; ookinetes traverse the mosquito gut epithelium. All invasive stages are characterized by apical organelles and can invade or pass through host cells. |
|
|
What are the two distinct merogony types obsevrved in malaria life cycle?
|
The first, called exoerythrocytic schizogony, occurs in the liver and is initiated by the sporozoite.
Second, the resulting merozoites then invade erythrocytes and undergo repeated rounds of merogony called erythrocytic schizogony. Some of the merozoites produced from the erythrocytic schizogony will undergo gametogony. |
|
|
Describe the two plasmodium gametogony phases
|
1) gametocytogenesis occurring in the bloodstream
of the vertebrate host, 2) gametogenesis taking place in the mosquito gut. The gametes fuse to become a zygote which first develops into an ookinete and then becomes an oocyst where sporogony takes place. |
|
|
Summarize the invasive stages
|
Invasive Stages
Merozoite --> erythrocytes Sporozoite --> salivary glands and hepatocytes Ookinete --> epithelium |
|
|
Malaria epi info
|
causative agent = Plasmodium species
40% of world’s population lives in endemic areas 3-500 million clinical cases per year 1.5-2.7 million deaths (90% Africa) |
|
|
Who identified malaria
|
Laveran 1880
|
|
|
Who demonstrated malaria's mosqutito transmission
|
Ross 1898
|
|
|
Who described malaria's liver stage?
|
Garnham 1940s
|
|
|
What stage are most of the pathology and clinical manifestations associated with malaria found?
|
the asexual erythrocytic stage parasites. Tissue
schizonts and gametocytes cause little, if any, pathology |
|
|
The severity of malaria attacks are dependent onw what factors?
|
manifestations and severity depend on parasite species and host status: immunity, general health, nutritional state, genetics
|
|
|
How long do recrudenseces or relapses occur?
|
recrudescences or relapses can occur over months or years
|
|
|
What are the three ways you can get malaria?
|
natural (sporozoites/Anopheles)
blood transfusions congenital : relatively rare although placenta is heavily infected |
|
|
What is different about malaria that was transmitted via blood transfusions?
|
shorter incubation period
fatality risk (P. falciparum) no relapses possible (vivax/ovale) Mechanical transmission of infected blood via blood transfusions or sharing syringes will result in a shorter incubation period because there is no liver stage. There is also an increased risk of fatality with mechanically transmitted P. falciparum. The lack of the liver stage infection as a result of mechanical transmission also precludes relapses in P. vivax or P. ovale infections. Table |
|
|
what are the prepatent periods for Pf, Pv, Po, Pm?
|
Prepatent period (days)
Pf, Pv, Po, Pm 6–9, 8–12, 10–14, and 15–18, respectively |
|
|
What are the incubation periods for Pf, Pv, Po, and Pm?
|
Incubation period (days)
Pf, Pv, Po, and Pm? 7–14, 12–17, 16–18, 18–40, respectively |
|
|
What are the merozoite maturation (days) for Pf, Pv, Po, and Pm?
|
Merozoite maturation (days)
Pf, Pv, Po, and Pm 5–7, 6–8, 9, 12–16, respectively |
|
|
How many merozoits are produced for Pf, Pv, Po, and Pm?
|
Merozoites produced
Pf, Pv, Po, and Pm 40,000; 10,000; 15,000; 2000, respectively |
|
|
What are the prodromal symptoms and when do they occur?
|
All four species can exhibit nonspecific prodromal symptoms a few days
before the first febrile attack. These prodromal symptoms are generally described as flu-like and include: headache, slight fever, muscle pain, anorexia, nausea, and lassitude. The symptoms tend to correlate with increasing numbers of parasites in the blood. |
|
|
What are malaria paroxysms?
|
Febrile Attack (Malaria Paroxysm)
prodromal symptoms will be followed by febrile attacks also known as malarial paroxysms. These paroxysms exhibit periodicities of 48 hours for P. vivax, P. ovale, and P. falciparum, and a 72-hour periodicity for P. malariae. periodic febrile episodes every 48 or 72 hours alternating with symptom-free periods initially fever may be irregular before developing periodicity may be accompanied by splenomegaly, hepato-megaly (slight jaundice), hemolytic anemia |
|
|
What is the malaria paroxysm cold stage?
|
The malarial paroxysm usually lasts 4–8 hours and begins
with a sudden onset of chills in which the patient experiences an intense feeling of cold despite having an elevated temperature. Cold stage: Feeling of intense cold Vigorous shivering Lasts 15–60 minutes |
|
|
What is the malaria paroxysm hot stage?
|
Immediately following this cold stage is the hot stage. The patient feels an intense heat accompanied by severe headache.
Fatigue, dizziness, anorexia, myalgia, and nausea will often be associated with the hot stage. Hot stage: Intense heat Dry burning skin Throbbing headache Lasts 2–6 hours |
|
|
What is the malaria paroxysm sweating stage?
|
Next a period of profuse sweating will ensue and the fever will start to decline. The
patient is exhausted and weak and will usually fall asleep. Upon awakening the patient generally feels well, other than being tired, and does not exhibit symptoms until the onset of the next paroxysm. Sweating stage: Profuse sweating Declining temperature Exhausted and weak --> sleep Lasts 2–4 hours |
|
|
What are the malaria paraxysms associated with?
|
paroxysms associated with synchrony of merozoite release
between paroxysms temperature is normal and patient feels well falciparum may not exhi-bit classic paroxysms continuous fever 24 hr periodicity |
|
|
What species are tertian verses quartan malaria?
|
Pf, Pv, Po - tertian
Pm - quartan |
|
name the species fever pattern
|
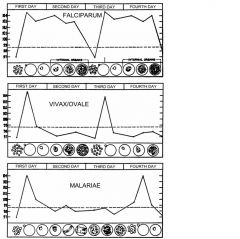
Pf, Pv/Po, Pm
|
|
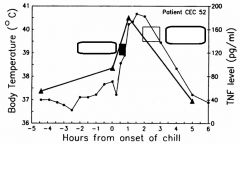
What is the relationship between fever and TNF-alpha levels?
|
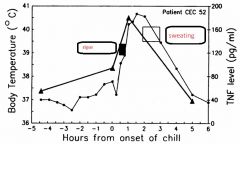
Body temperature (circles) and serum TNF-a levels (triangles) were measured during the malarial paroxysm. The hatched box denotes the period of intense shivering, the black box the hot stage and the gray box denotes profuse sweating.
Presumably antigens or toxins are released into the bloodstream and tissues when the infected erythrocyte ruptures. These released parasite products then stimulate macrophages and other immune effector cells to produce TNF-a and other cytokines leading to the febrile attacks. It has been suggested that a major component of this presumptive toxin might be glycosylphosphatidylinositol derived from various parasite proteins. |
|
|
Describe the severity of initial paroxysms for Pv, Po, Pm, and Pf
|
Pv: Moderate to severe
Po: Mild Pm:Mild to moderate Pf: Severe |
|
|
What is the average parasiemia (mm3) for Pv, Po, Pm, and Pf?
|
Pv: 20,000
Po: 9,000 Pm: 6,000 Pf: 50,000–500,000 |
|
|
What is the maximum parasiemia (mm3) for Pv, Po, Pm, and Pf?
|
Pv: 50,000
Po: 30,000 Pm: 20,000 Pf: 2,500,000(half of all RBCs are infected) |
|
|
What is the symptom duration (untreated) for Pv, Po, Pm, and Pf
|
Pv: 3–8+ weeks
Po: 2–3 weeks Pm: 3–24 weeks Pf: 2–3 weeks |
|
|
What is the maximum infection duration (untreated) for Pv, Po, Pm, and Pf
|
the maximum infection duration (untreated)
Pv: 5–8 years* Po: 12–20 months* Pm: 20–50+ years Pf: 6–17 months * Includes relapses from the hypnozoite stage. Relapses due to the activation of P. vivax hypnozoites can occur for several years. P. ovale is the most benign in that the paroxysms tend to be mild and of short duration and relapses seldom occur more than one year after the initial infection. |
|
|
What is the level of anemia for Pv, Po, Pm, and Pf
|
Pv: ++
Po: + Pm: ++ Pf: ++++ |
|
|
Which species has renal complications?
|
Pm
P. malariae is the most chronic, though, and recrudescences have been documented several decades after the initial infection. This chronicity is sometimes associated with renal complications, which are probably due to the deposition of antigen–antibody complexes in the glomeruli of the kidney. |
|
|
Which species has cerebral complications
|
Pf
P. falciparum can produce serious disease with mortal consequences. This increased morbidity and mortality is due in large part to the high parasitemias associated with P. falciparum infections. These potentially high parasitemias are partly the result of the large number of merozoites produced and the ability of P. falciparum to invade all erythrocytes. |
|
|
What RBCs do the different species prefer?
|
P. falciparum to
invade all erythrocytes. P. vivax and P. ovale prefer reticulocytes (i.e., immature erythrocytes) P. malariae prefers senescent erythrocytes. |
|
|
What is associated with higher parasitemias in Pf?
|
Higher parasitemias are also associated with the cytoadherence and sequestration of P. falciparum.
This sequestration in the tissues minimizes removal of infected erythrocytes by the spleen and can be viewed as an avoidance of the immune system. In addition, the cytoadherence to the endothelial cells of the capillaries allows for a more efficient erythrocyte invasion because the blood flow is much slower. The low oxygen tension found in the deep tissues is also metabolically favorable for parasite growth. |
|
|
Describe anti-malarial immunity
|
P. falciparum can be lethal in non-immune (eg., children, expatriates)
paroxysms become less severe and irregular as infection progresses semi-immune may exhibit little (1-2 days fever) or no symptoms Immunity against malaria is slow to develop and requires multiple exposures. - slow to develop - short lived - - - ‘premunition’ - non-sterilizing - - - lower parasitemia - - - less symptoms |
|
|
What is anti-parasite immunity?
|
immune response prevents merozoite invasion, eliminates infected erythrocytes, etc.
the “antiparasite” immunity which lowers the parasitemia |
|
|
What is anti-disease immunity?
|
eg., neutralization of exo-antigens or toxic effects
The observation that asymptomatic individuals can exhibit high levels of parasitemia has led to the concept of “antidisease” immunity. antigens or toxins released by the infected erythrocyte might stimulate the production of proinflammatory cytokines. Antibodies against these exoantigens could neutralize their toxic effects and thus lead to an antidisease immunity. People from endemic areas develop antibodies specific for the parasite glycosylphosphatidylinositol, a proposed parasite toxin, and some studies show a correlation between these antibodies and improved clinical outcomes. |

