![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
315 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
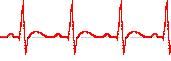
What does the following ECG Waves/Intervals represent?
P wave |
the sequential activation (depolarization) of the right and left atria
duration =conduction time through atria |
|
|
|
What does the following ECG Waves/Intervals represent?
QRS complex |
right and left ventricular depolarization (normally the ventricles are activated simultaneously)
|
|
|
|
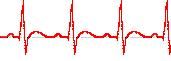
What does the following ECG Waves/Intervals represent?
ST-T wave: |
ventricular repolarization
|
|
|
|
What does the following ECG Waves/Intervals represent? U wave:
|
origin for this wave is not clear - but probably represents "afterdepolarizations" in the ventricles
|
|
|
|
What does the following ECG Waves/Intervals represent?
PR interval: |
time interval from onset of atrial depolarization (P wave) to onset of ventricular depolarization (QRS complex)
↑ conduction velocity through AV node → ↓ PR interval ↓ conduction velocity through AV node → ↑ PR interval |
|
|
|
What does the following ECG Waves/Intervals represent?
QRS duration: |
duration of ventricular muscle depolarization
|
|
|
|
What does the following ECG Waves/Intervals represent?
QT interval: |
duration of ventricular depolarization and repolarization
|
|
|
|
What does the following ECG Waves/Intervals represent?
RR interval: |
duration of ventricular cardiac cycle (an indicator of ventricular rate)
|
|
|
|
What does the following ECG Waves/Intervals represent?
PP interval: |
duration of atrial cycle (an indicator of atrial rate)
|
|
|
|
What are the bipolar limb leads and what plane are they in?
|
Frontal Plane
Lead I Lead II Lead III |
|
|
|
Where is Lead I and what are the charges?
|
RA (-) to LA (+) (Right Left, or lateral)
|
|
|
|
Where is Lead II and what are the charges?
|
RA (-) to LF (+) (Superior Inferior)
|
|
|
|
Where is Lead III and what are the charges?
|
LA (-) to LF (+) (Superior Inferior)
|
|
|
|
Which are the Augmented unipolar limb leads? What plane?
|
Frontal plane
aVR aVL aVF |
|
|
|
Where is lead aVR placement, charge and direction?
|
Lead aVR: RA (+) to [LA & LF] (-) (Rightward)
|
|
|
|
Where is lead aVL placement, charge and direction?
|
Lead aVL: LA (+) to [RA & LF] (-) (Leftward)
|
|
|
|
Where is lead aVF placement, charge and direction?
|
Lead aVF: LF (+) to [RA & LA] (-) (Inferior)
|
|
|
|
What are the Unipolar (+) chest leads and in what plane? What direction?
|
(Transverse plane):
Leads V1, V2, V3: (Posterior Anterior) Leads V4, V5, V6:(Right Left, or lateral) |
|
|
|
The 6 major sections in the "method" of reading an ECG (per extra info, not slides).
|
1. Measurements
2. Rhythm Analysis 3. Conduction Analysis 4. Waveform Description 5. Ecg Interpretation 6. Comparison with Previous ECG (if any) |
|
|
|
What is the resultant cardiac vector?
|
The vector sum of all cardiac electrical activity (at any time).
|
|
|
|
Depolarization moving towards a Positive electrode produces what type of deflection?
|
Upward
|
|
|
|
Depolarization moving towards a negative electrode produces what type of deflection?
|
downward
|
|
|
|
What is Einthoven’s law?
|
States that the net QRS magnitude in
leads I & III = Lead II |
|
|
|
How are the Augmented Limb Leads
different than the bipolar limb leads? |
They are 50% larger
|
|
|
|
what does the aVR lead show?
|
Sees the cavities of the ventricles. Atrial & ventricular depolarization and ventricular repolarization move away from the electrode: P-wave, QRS, T-wave are all negative.
|
|
|
|
what does the aVL and aVF lead show?
|
looks at the ventricles. Deflections are predominantly positive.
|
|
|
|
Leads V1 & V2 are mainly where?
What is their QRS wave typically? |
the Right side of the heart
mainly NEGATIVE QRS wave... |
|
|
|
Lead V3 is mainly where?
What is their QRS wave typically? |
Over interventricular septum
measuring the right bundle branch QRS is "net" Neutral |
|
|
|
Lead V4 is mainly where?
What is their QRS wave typically? |
Over interventricular septum
measuring the left bundle branch {QRS is "net" Neutral-more positive] |
|
|
|
Lead V5 & V6 are mainly where?
What is their QRS wave typically? |
the Left side of the heart
mainly POSITIVE QRS wave... |
|
|
|
How will hypertrophy affect the EKG?
|
Hypertrophy: ↑ depolarization activity and displaces mean QRS vector towards hypertrophied side for a right or left axis deviation
|
|
|

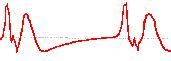
What is the arrhythmia?
|

First Degree Heart block:
Long PR interval |
|
|

|

Asystole
|
|
|

|

Digitalis Effect
Scooping ST segment |
|
|

|

Bradycardia
Normal P, QRS, T, rate < 60 |
|
|
|
Hypercalcemia
Short/absent ST segment |
|
|

|

Tent-shaped Twave
hyperkalemia |
|
|
|

Idioventricular Rhythm (IVR)
No Pwave, bizarre QRS, rate 20-40 |
|
|

|

Normal
|
|
|

|

Premature Atrial Contraction (PAC)
Premature Pwave, irregular P-P interval |
|
|

|

Premature Ventricular Contraction (PVC)
Wide QRS, unrelated to Pwave |
|
|

|

Normal P, QRS, T, rate > 100
Tachycardia, Sinus Rhythm |
|
|

|

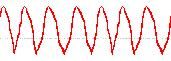
Ventricular Fibrillation (VFIB)
Chaotic waves |
|
|
|
Bizarre, wide QRS, no Pwav, rate > 100
Ventricular Tachycardia (VTAC) |
|
|
|
Elevation of the ST segment my be caused by:
|
Angina w/o exertion
Pericarditis |
|
|
|
Depression of the ST segment my be caused by:
|
digitalis
|
|
|
|
What is the sequence of electrical events in the heart? (Pathway)
|
Cardiac Depolarization at the SA node ->AV node ->Bundle of His->
Bundle branches (L & R) -> Purkinje fibers |
|
|
|
Where is the the fastest conduction in the heart?
|
Purkinje fibers @ 4.0 m/s
|
|
|
|
What are the 4 main pathways of the atrial conduction system?
|
Anterior, Middle and Posterior Internodal Track and Bachmans bundle to left atrium
|
|
|
|
The rate of the SA node varies with what factor?
|
Inspiration causea and Increase
while expiration causes a decrease |
|
|
|
Name the three automaticity foci
|
Atrial automaticity foci
Juntional automaticity foci Ventricular automaticity foci |
|
|
|
Where is the Juntional automaticity
foci located? |
middle & distal regions of AV node
|
|
|
|
Where is the Ventricular
automaticity foci located? |
His bundle & Bundle branches
|
|
|
|
What is the highest rate of automaticity for the SA node?
|
72/min
|
|
|
|
What is the rate of automaticity for the atrial foci?
|
60-80 per minute
|
|
|
|
What is the rate of automaticity for the AV junction foci?
|
40-60 per minute
|
|
|
|
What is the rate of automaticity for the ventricle foci?
|
20-40 per minute
|
|
|
|
What is the term for the faster more superior foci taking control/lead?
|
Overdrive supression
|
|
|
|
The ventricles are completely depolarized during
which isoelectric part of the EKG recording? |
ST Segment
|
|
|
|
How long is a typical P wave and what does the time/length represent?
|
0.1 sec
conduction time through atria |
|
|
|
How long is a normal PR interval?
What does it represent? |
0.12-0.20
Time from initial atrial depolarization to time of initial depolarization of ventricles. It is the filling time for the ventricles. |
|
|
|
↑ conduction velocity through AV node shows how in an EKG?
|
↓ PR interval
|
|
|
|
↓ conduction velocity through AV node shows how on an EK?
|
↑ PR interval
|
|
|
|
How long should the T wave be and what does it represent? What plase of the cardiac cycle?
|
0.16 sec
Later repolarization of ventricles ( Reduced ejection phase) |
|
|
|
What direction does Repolarization occur?
|
epicardial surfaces to endocardium. OUTSIDE→IN
|
|
|
|
What direction does depolarization occur?
|
endocardium.surfaces to epicardial INSIDE→OUT
|
|
|
|
The QT interval Represents?
What does it include? |
First ventricular depolarization to last ventricular ventricular
repolarization or Duration of Ventricular systole • Includes: – QRS complex – ST segment – T wave. |
|
|
|
How long should a QT interval be?
|
QT interval is normal if it is ½ the R-R interval.
|
|
|
|
What is the relationship between heart rate, QT interval and RR Interval?
|
If HR increases, RR & QT decrease and visa versa
|
|
|
|
What does the U wave reperesent?
|
repolarization of papillary muscle.
(Not always visible) |
|
|
|
Changes in Duration & Amplitude of EKG waves & intervals waves & intervals indicate what?
|
depict changes in Muscle mass
(hypertrophy)or conduction issues |
|
|
|
↑ HR & ↓ cycle length have what affect on duration of AP, refractory periods and excitability?
|
They decrease
|
|
|
|
How do you calculate heart rate?
|
HR = 1/cycle length (or r-r time)
|
|
|
|
What are the time measurements of the x-axis on dark (large) and light gridmarks on EKG paper?
|
dark lines on grid are 0 2 sec apart; light lines are 0 04 sec apart.
|
|
|
|
What does the y axis of the ekg paper reperesent?
|
Voltage gain = 1 mV/cm
|
|
|
|
What is the pattern for counting big squares (from Dubin)?
|
300,150, 100, 75,60,50
|
|
|
|
What steps per physiology to analyze EKG?
|
1. Calculate –ventricular and atrial rate:
2. Calculate – P-R interval 3. Calculate – QRS duration: |
|
|
|
how do you Calculate the mean axis of ventricular depolarization?
|
take the net from Leads I,II, & III and plot on triangle. Intersection is correlating quadrant. (each space 2 ticks)
|
|
|
|
What does the The amplitude (voltage) of and EKG tell us?
|
The size of the chamber or The mass (number) of active cells
|
|
|
|
How do Arrhythmias generally present on an EKG?
|
P-P interval will lengthen or decrease
P, QRS, T waves = normal ↑ or ↓ HR: Cardiac cycle duration changes |
|
|
|
What would cause a short P-P interval?
|
SNS/ flight/fight
>100 bpm is sinus tachycardia |
|
|
|
Under what influence/stimulation would cause a longer P-P interval?
What is a long p-p generally named/diagnosed? |
PNS (athletes)
< 60 cycles/min sinus bradycardia |
|
|
|
What are the characteristics of a 1° Atrioventricular conduction blocks?
|
Electrical transmission through the AV node is impeded. Delay is located ABOVE the His bundle
PR interval is lengthened > 0.2s Rate = variable P wave = normal Rhythm = regular Look for the start of a Pwave to the tip of an R wave to be bigger than 1 large box (.2sec) |
|
|
|
What could cause a a 1° Atrioventricular conduction block?
|
Digitalis toxicity
|
|
|
|
What are the characteristics of a Mobitz type I - Wenckebach conduction block?
|
Second Degree AV block occurs IN the AV node
P-R interval is progressively longer until one P wave is blocked; the cycle begins again following the blocked P wave. Not all P waves are followed by QRS complexes. Rate = variable Failure of impulses to reach ventricles. P wave = normal with constant P-P interval Rhythm = irregular |
|
|
|
What could cause a a 2° Type I conduction block?
|
Mobitz type I - Wenckebach
Digoxin toxicity, calcium channel blockers |
|
|
|
Whats the Wenckebach ratio?
|
Wenckebach series has a
consistent P:QRS ratio; 3:2, 4:3, 5:4 (1 less QRS than P) |
|
|
|
What's the tx for Type 1 Mobitz 2* AV block?
|
Tx : not indicated since rhythm produces no symptoms
|
|
|
|
What are the characteristics of a Second Degree AV Type II block?
|
Second Degree AV block occurs below the Bundle of His.
Dropped beats that are NOT preceded in a change in PR interval. Rate = variable P wave = normal with constant P-P interval QRS = often widened Rhythm = regular |
|
|
|
Whats the Mobitz Type II ratio?
|
Each repeating Mobitz series has a
consistent P:QRS ratio; 3:1, 4:1, 5:1 |
|
|
|
What are the potential causes of a Second Degree AV Mobitz Type II block?
|
After acute anterior MI – due to damage in bundle branches.
|
|
|
|
What is the treatment of a a Second Degree AV Mobitz Type II block?
|
artificial pacing
|
|
|
|
What would a Mobitz 2:1 block look like? 3:1?
|
2 P-waves to 1 QRS; 3 P-waves to 1 QRS
|
|
|
|
What are the characteristics of a 3° Atrioventricular conduction block?
|
Atrial & ventricular activities are unrelated due to complete block of atrial impulses to ventricles. Complete block at AV junction, common bundle or bundle branches.
Rate = atrial rate is normal, ventricular rate < 70bpm. P wave = normal with constant P-P interval (not “married” to QRS complexes) Another automaticity focus will pick up ventricle pacing QRS = widened or normal Rhythm = irregular |
|
|
|
What are the potential causes of a 3° Atrioventricular conduction block?
|
Older pt with degeneration of conductive tissue
|
|
|
|
What are the tx of a 3° Atrioventricular conduction block?
|
external pacing
|
|
|
|
In First degree A-V block the PR interval is?
|
Greater than 0.2s.
|
|
|
|
Describe the relationship between velocity of blood flow, pressure and the cross-sectional area of the vascular bed.
|
Velocity and pressure are inversely related to area.
High velocity, higher pressure, smaller area |
|
|
|
Describe the relationship between blood flow, pressure and resistance in a typical vascular bed.
|
Blood flow rate is constant
Velocity of flow is decreased as blood is ejected smaller vessels. Velocity of flow inversely proportional to the total X- sectional area Velocity of flow is slowest in the capillaries, which have the largest X-sectional area Cardiac output is in parallel series to organs with different % of blood to different organs) |
|
|
|
What does the pressure at the beginning of systemic circulation equal?
|
mean arterial pressure? (Average 93 mmHg)
|
|
|
|
What is the pressure at the end of systemic circulation?
|
0 mmHg
|
|
|
|
increasing pressure does what to flow?
|
increases it
|
|
|
|
if absolute pressure stays the same, what will happen to flow?
|
It will remain the same
|
|
|
|
What is Vascular resistance?
|
is a measure of hindrance to blood flow caused by friction between moving blood and the vessel wall
|
|
|
|
What is the most important factor in Poiseuille’s Equation?
|
Most important factor is radius.
Decreasing the radius by ½ does not increase the resistance 2-fold. It increases it 16-fold. |
|
|
|
flow rate depends on what 2 main factors?
|
Pressure gradients (delta-P between two points along the vascular system) & Vascular resistance
|
|
|
|
What is laminar flow?
|
Energy efficient flow where the velocity touching the wall of the vessel is 0 and the blood that is most center is the fastest (parabola in between)
|
|
|
|
How might flow become turbulent?
|
with clot, thrombi, aneurysm, anemia, atherosclerosis, valvular defects
|
|
|
|
What are the criteria of laminar and turbulent flow?
|
N R less than 2000, flow is laminar
N R greater than 3000, flow is turbulent N R between 2000 and 3000: -flow is transitional between laminar and turbulent |
|
|
|
Which vessles are most compliant?
|
Veins/Venous structures
|
|
|
|
What is an unstressed volume?
|
Large Volume, low Pressure (veins)
|
|
|
|
What is an stressed volume?
|
Low Volume, high Pressure (arteries)
|
|
|
|
When do arteries become arterioles?
|
In the organ: can adjust flow within
|
|
|
|
Arteries contain more of what type of fibers?
|
smooth muscle and elastic fibers to serve as PRESSURE reservoir
|
|
|
|
Veins contain more of what type of fibers?
|
more collagen fibers to serve as a BLOOD reservoir
|
|
|
|
What is cardiac inootropy?
|
the same thing as Contractility
|
|
|
|
What is Trepp?
|
It is the increasing HR that causes Ca 2+ accumulation which increases
contractility |
|
|
|
When afterload increases what happends to the ESV and stroke volume?
|
there is an increase in end-systolic volume and a decrease in stroke volume.
(Preload changes secondarily to changes in afterload) |
|
|
|
Afterload is increased when...
|
aortic pressure and systemic vascular resistance are increased, by aortic valve stenosis, and by ventricular dilation.
|
|
|
|
What is Contractility?
|
the intrinsic ability of the heart to contract independent of preload and afterload at any given fiber length
|
|
|
|
what factors affect contractility?
|
– ANS activity
– circulating hormones (i.e.,epinephrine) – Ca 2+ influx and availability |
|
|
|
What is preload?
|
Preload can be defined as the initial stretching of the cardiac myocytes prior to contraction. It is "measured" by the end-diastolic volume (EDV) which will indicate how stretched the sarcomeres are.
|
|
|
|
What factors affect preload? (5)
|
- filling time
- compliance - filling pressure - atrial systole - pericardial constraint |
|
|
|
What is afterload?
|
Afterload can be thought of as the "load" or pressure that the heart must eject blood against.
|
|
|
|
What factors affect afterload?
|
- arterial pressure
peripheral resistance arterial compliance - viscosity of blood - valve function |
|
|
|
What is the effect of Norepinepherine on contractility?
|
– increases the velocity of shortening
– increases ejection velocity – increases stroke volume – decreases ESV |
|
|
|
What happens to the rate of relaxation under SNS stimulation?
|
it is also enhanced to allow for the increased heart rate (needs filling time still)
|
|
|
|
A decrease in contractility causes what changes in ESV and SV?
|
increase in ESV and a decrease in stroke volume
|
|
|
|
What is the ratio of SV to EDV?
What is abnormal? |
– normal 50-75%
– abnormal < 40 |
|
|
|
What is the The Effect of Heart Rate on Cardiac Output in the following senario:
stroke volumes declines as heart rate encroaches on the rapid filling phase |
There is a peak output and then a
decrease. At too high of a SV, the cardiac output would be too drastically affected due to the decrease in filling time |
|
|
|
What is the The Effect of Heart Rate on Cardiac Output in the following senario:
stroke volume increases due to compensatory mechanisms, such as increased contractility |
then cardiac output will reach a higher peak before diastolic filling time becomes limiting
|
|
|
|
What does Ventricular minute work measure?
|
Contractile work per minute rather than per beat.
|
|
|
|
What is the “Resting” metabolic rate of the heart?
|
4.8 - 6 ml / gm / h.
|
|
|
|
How is the RMR of the heart divided?
|
25% to basal metabolism, the rest for contraction
|
|
|
|
How does left ventricle work compare to right ventricle work?
|
left ventricle does 6 to 7X the work of the right ventricle
|
|
|
|
What are the Metabolic substrates of the heart and their percentages?
|
35 to 40% of energy requirement from carbohydrate oxidation under basal conditions
Balance from Fatty Acid Oxidation |
|
|
|
What is Cardiac Efficiency?
|
Ratio of the work performed to the energy consumed
|
|
|
|
What is the Efficiency of myocardium usually? How does it change during exercise?
|
Efficiency of myocardium is usually from 5 to 15 %
Efficiency improves during exercise |
|
|
|
A . ↑↑HR (>150) will have what effect?
|
SV decreases, can't fill
CO decreases |
|
|
|
Where is the atrial kick represented on the EKG
|
P wave
|
|
|
|
What are the exogenous sources of fuel for the heart?
|
BLOOD
» glucose, lactate » fatty acids, ketone bodies |
|
|
|
What are the endogenous sources of fuel for the heart?
|
(intracellular stores):
» glycogen, triglycerides |
|
|
|
Uptake of fuels by the heart is
dependent on what factors? |
Workload
fed/fasted metabolic state changes in concentrations of fuel in the circulation |
|
|
|
4 Sources of ATP from carbohydrate metabolism
|
– glycolysis
– glucose oxidation – lactate oxidation – glycogen stores |
|
|
|
3 Sources of ATP from fatty acid metabolism
|
– triglyceride lipolysis and oxidation of the fatty acid
– lipoprotein and chylomicron oxidation – ketone body oxidation |
|
|
|
What is the Randle Cycle?
|
The Randle cycle is a metabolic process involving the competition of glucose and fatty acids for substrates in the fed (favoring CHO) or fasted state (favoring FFA.
High levels of lipids are oxidized in preference to glucose |
|
|
|
Whats generally going on during a fasted state?
|
Low levels of insulin; causes
– adipose tissue lipolysis is stimulated – blood FFA are high – FFA uptake by the heart – As FFA are oxidized, glucose use is inhibited |
|
|
|
What are the effects of low insulin?
|
– adipose tissue lipolysis is stimulated
– blood FFA are high – FFA uptake by the heart – As FFA are oxidized, glucose use is inhibited |
|
|
|
What happens when insulin levels are high?
|
– inhibits adipose tissue lipolysis
– increases glucose uptake in heart – increases glucose use by the heart Increase in glucose use overcomes the effects of FFA. |
|
|
|
What is the relationship between fat oxidation and glucose oxidation
|
inverse
|
|
|
|
Increased mitochondrial b-oxidation results in what enzymatic changes?
|
Cirtate and Acetly-CoA increase
– Citrate inhibits phosphofructokinase activity – Acetyl CoA inhibits pyruvate dehydrogenase This increases G-6-P, inhibiting hexokinase and resulting in a decrease in glucose uptake. |
|
|
|
when fat metabolism is decreased what two enzymes are no longer inhibited?
|
Inhibition on PDH and PFK is removed
|
|
|
|
As the level of fatty acid increases, oxidation of what increases?
|
palmitate oxidation
|
|
|
|
What is the effect of inhibiting glucose oxidation on the heart?
|
Inhibiting glucose
oxidation contributes to LV failure |
|
|
|
What conditions are associated
with excessively high rates of fatty acid oxidation? |
angina, infarct, diabetes, and post cardiac surgery
|
|
|
|
Why are high rates of fatty
acid metabolism detrimental? |
Induce cardiac arrhythmias
Increase oxygen consumption Promotes oxygen wasting yg g Reduces cardiac performance Leads to heart failure |
|
|
|
FAs inhibit key enzyme functions in what systems/mechanisms? (5)
|
»Na + -K + -ATPase, Ca 2+ ATPase
»ETS and Krebs cycle »Adenine nucleotide translocase »Pyruvate dehydrogenase Pyruvate dehydrogenase »Suppress glucose oxidation |
|
|
|
What is the metabolic breakdown of a heart with uncontrolled DM?
|
The heart relies exclusively on fatty acid metabolism
|
|
|
|
Infarct and cardiac surgery release what hormone with what effect on the heart?
|
epinephrine which increases plasma FFA (free fatty acids)
|
|
|
|
What enzyme is pharomocologically targeted to inhibit B-Oxidation?
|
ketoacyl CoA thiolase
|
|
|
|
What (2) drugs can block ketoacyl CoA thiolase?
|
Ranolazine, trimetazidine
|
|
|
|
How is FA uptake into the mitochondira inhibited pharmocologically?
|
by inhibiting carnitine palmitoyl transferase
|
|
|
|
What two drugs can inhibit carnitine palmitoyl transferase?
|
etomoxir, oxfenicine
|
|
|
|
Stimulation of pyruvate dehydrogenase will do what? What drug assists with this?
|
» dichloroacetate
pyruvate dehydrogenase is an enzyme for glucose metabolism, it will stimulate those cycles |
|
|
|
How can mitochondrial acetyl CoA levels be modulated with L-carnitine?
|
Use it to make acetylcarnitine reducing its ACoA's levles in the mitochondria which will Removes inhibition on pyruvate dehydrogenase
an enzyme in glucose metabolism pathways |
|
|
|
carnitine palmitoyltransferase I can be inhibited by what 2 drugs?
|
Oxfenicine
Etomoxir decreases FA oxidation |
|
|
|
What two drugs angian drugs can inhibit the oxidation of Fatty Acids?
|
Trimetazidine
Ranolazine |
|
|
|
What drug can inhibit inhibit the enzyme pyruvate dehydrogenase kinase?
|
Dichloroacetate
|
|
|
|
What pathways does lactate belong to?
|
Glucose oxidation pathway
|
|
|
|
What are the cnductile cells and why are they special
|
Bundle of His, Purkinje fibers, Sinoatrial (SA) node and
Atrioventricular (AV) node. they can generate spontaneous action potentials. |
|
|
|
What are the contractile cells of the heart called?
|
cardiac myocytes
|
|
|
|
Generally describe the Spread of Excitation in the heart
|
1. SA node: initiates action potential
2. Spread to the atria and to AV node 3. AV node: slow conduction 4. Bundle of His and Purkinje system: fast conduction |
|
|
|
What is conduction velocity?
|
speed of AP propagation through heart
fasest in the purkinjies slowest in the AV nodes |
|
|
|
What affects Conduction velocity?
|
1) rate of change in membrane potential as a function of time (i.e.
upstroke phase of action potential). 2) resistance |
|
|
|
What is a syncytium.?
What acts like this? |
A multinucleated mass of cytoplasm that is not separated into individual cells'
Cardiac cells |
|
|
|
Within intercalated discs, what two kinds of membrane junctions?
|
– Desmosomes: Mechanical junctions
– Gap junctions: Electrical junctions |
|
|
|
How does the legnth of cardiac AP compare to skeletal AP?
|
Long duration comparatively
|
|
|
|
Fast action potentials occur in what cell types?
|
contractile cells
|
|
|
|
Slow action potentials occur in what cell types?
|
pacemaker cells
|
|
|
|
What is Phase 0 of the Fast AP?
What Ionic influence? |
upstroke, rapid depolarization
– due to fast inward Na + current. |
|
|
|
What is Phase 1 of the Fast AP?
What Ionic influence? |
Phase 1: early repolarization
– electrochemical gradient favors K + movement out of the cell – inactivation gates on Na + channels close |
|
|
|
What is Phase 2 of the Fast AP?
What Ionic influence? |
Phase 2: plateau phase
–cause by balance between Ca 2+ (L-type channel; inward) current and K + (outward) currents |
|
|
|
What is Phase 3 of the Fast AP?
What Ionic influence? |
repolarization
Caused by turn-off of Ca 2+ current and further increase in K + currents. |
|
|
|
What is Phase 4 of the Fast AP?
What Ionic influence? |
resting potential
– Caused by large background K + outward current. (different channels than in Phase 3) – balanced by inward Na + and Ca 2+ current |
|
|
|
How can Phase 2 be inhibited?
|
can be inhibited by Ca 2+ channel blockers
|
|
|
|
Which phase of the fast AP is responsible for the very long AP?
|
Phase 2
|
|
|
|
What are the kinetics of Na+, Ca+, and K+?
|
Fast In
Slow In Fast Out |
|
|
|
What makes summation and tetanus of cardiac muscle is unlikely?
|
The fact that the long refractory period occurs in conjunction with
prolonged plateau phase, |
|
|
|
What are the key differences b/w fast and slow Aps?
|
1. automaticity
2. unstable resting membrane potential 3. no sustained plateau 4. No phases 1 & 2 |
|
|
|
What is happening in Phase 0 of the Slow Action Potentials?
What Ionic Influences? |
upstroke
– Slow due to inward long-lasting Ca 2+ current (L-type) |
|
|
|
What is happening in Phase 1 of the Slow Action Potentials?
What Ionic Influences? |
There isn't a phase 1
|
|
|
|
What is happening in Phase 2 of the Slow Action Potentials?
What Ionic Influences? |
There isn't a phase 2
|
|
|
|
What is happening in Phase 3 of the Slow Action Potentials?
What Ionic Influences? |
repolarization
– Caused by turn-off of Ca 2+ current and further increase in K + current. |
|
|
|
What is happening in Phase 4 of the Slow Action Potentials?
What Ionic Influences? |
pacemaker potential
(spontaneous depolarization) 1) repolarization from preceding AP turns on If (funny) current causing inward Na + 2)if threshold is reached a transient Ca 2+ current (T-type channel; inward) is turned on 3)AP peaks and K+ moves out of the cell |
|
|
|
Maximum diastolic potential in slow AP?
|
-65mV
|
|
|
|
What are the three criteria for "Normal" sinus rhythm?
|
AP must originate from the SA node
SA impulses must be regular and 60-100 per minute normal conduction |
|
|
|
When do Latent pacemakers appear?
|
If conduction is blocked or superior pacemaker isn't working
|
|
|
|
What is the Source of initiating calcium for cardiac muscle?
|
Extracellular
|
|
|
|
Whats the role of tropomyosin?
|
inhibits binding of myosin to actin
|
|
|
|
What is the role of troponin?
|
Ca 2+ -sensitive molecular switch, changes conformation so binding site for myosin can be exposed
|
|
|
|
What are the three parts of troponin?
|
TnC: “calcium sensor”, calcium binding produces a conformational change in TnI
TnT: links Tn complex to Tm, appears to control the position of Tm on the thin filament TnI: binds to actin and inhibits myosin ATPase |
|
|
|
how are myofilaments arranged?
|
into sarcomeres like skeletal muscle
|
|
|
|
Whats the legnth of a sarcomere?
|
z to z band
|
|
|
|
What's the A band?
|
the legnth of the myofilaments
|
|
|
|
Which bands shorten in a cross bridge cycling? Which stays the same?
|
I-bands and the H-zone shorten, Z bands come closer together,
A-bands do not change their length |
|
|
|
What are the steps of Excitation-Contraction Coupling in Cardiac
Contractile Cells? |
1. Excitation - AP causes the
depolarization of the membrane. 2. Ca 2+ channels open (during plateau of AP). 3. Ca 2+ enters cell (“trigger” Ca 2+ ) • Ca 2+ -induced Ca 2+ release from SR via ryanodine receptor. 4. Ca 2+ binds to troponin. 5. Crossbridge cycling. |
|
|
|
When are Ca++ channels opening in a long AP?
|
During phase 2 plateau phase
|
|
|
|
What is SERCA?
What does it do? |
Sarco(Endo)plasmic Reticulum Ca++-ATPase
It is a Ca2+ ATPase that transfers Ca2+ from the cytosol of the cell to the lumen of the SR at the expense of ATP hydrolysis during muscle relaxation. |
|
|
|
What effect does inhibiting the Na + /K + ATPase have on the cardiac muscle cell?
|
Blocking na/katpase exchanger will cause intracellular Na+ to stay high. If Na+ is high, the Na+/Ca2+ will want to get rid of Na+ and hang on to Ca+. Higer intracellular Ca+
will Enhances force of contraction as tension development proportional to Ca 2+ |
|
|
|
What drugs inhibit Na/K-ATPase exchanger?
|
Digitalis, Digoxin
|
|
|
|
T h e f o r c e d e v e l o p e d b y
contraction of cardiac muscle depends on... |
Initial fiber legnth
|
|
|
|
Describe Length-Tension Relationship & Starling’s Law of the Heart
|
the greater the volume of blood entering the heart during diastole (end-diastolic volume), the greater the volume of blood ejected during systolic contraction (stroke volume) and vice-versa, such that Initial length of myocardial fibers determines the initial work done during the cardiac cycle.
|
|
|
|
Increasing cardiac muscle length has what impact on Ca+:
(3) |
• increases the Ca 2+ sensitivity of troponin C
• increases Ca 2+ release from the SR • Produce large changes in tension |
|
|
|
Positive inotropic effect
|
increase in contractility and rate
of tension development at a given fiber length. |
|
|
|
Negative inotropic effect
|
decrease in contractility and a
decrease in the rate of tension development at a given fiber length. |
|
|
|
What factors have a - negative inotropic effect?
|
parasympathetic stimuation
heart failure |
|
|
|
What factors have a + positive inotropic effect?
|
Sympathetic NS stimulation
Catecholamines Heart Rate |
|
|
|
Nuclei of cardiac muscle are...
|
usually single, central
|
|
|
|
What is contraction of cardiac muscle like (compared to smooth and skeletal)
|
slower onset, cannot be tetanized
|
|
|
|
What is the significance of the only slightly curved line on the volume/pressure graph during diastole?
|
It indicates that the ventricle is easy to fill and that the heart is difficult to "overfill"
|
|
|
|
On a Pressure-Volume loop what point would indicate where the mitral valve opens?
|
lower left "corner"
|
|
|
|
On a Pressure-Volume loop what point would indicate where the mitral valve closes?
|
lower right "corner"
|
|
|
|
On a Pressure-Volume loop what point would indicate where the aortic valve opens?
|
upper right "corner"
|
|
|
|
On a Pressure-Volume loop what point would indicate where the aortic valve closes?
|
upper left "corner"
|
|
|
|
Where is the EDV indicated on a PV Loop?
|
lower right "corner" on the X axis... Mital valve is closing, so at end volume for the ventricle
|
|
|
|
How do you find the stroke volume in the PV loop?
|
It is the measure of the horozontal line inside the loop (the equivialent of measuring 0 volume to EDV and subtracting 0-start of the loop on the x axis which is equivialent to the ESV
|
|
|
|
Where is the end systolic point on the PV loop?
|
Top left corner b4 isov relaxation
|
|
|
|
If you added 2nd loop to the PV loop with the preload increased and the afterload and contractility remained the same how would it look?
|
The EDV for loop 2 would be at a higher volume on the x axis and the pressure at this point is higer than that of loop1. The slope for the end systolic pressure/volume line is the same and the afterload lines are parallel, so they are considered the same. The stroke volume of loop 2 is larger.
|
|
|
|
If you added 2nd loop to the PV loop with the afterload increased and the preload and contractility remained the same how would it look?
|
The EDV point would be the same for both loops
loop 2 would have a greater angle/slope on the line from the end systolic point to the x axis indicating the afterload was increased. The stroke volume would decrease |
|
|
|
How do you find preload on the PV loop?
|
Its the EDV or lower right "point"
|
|
|
|
How do you find afterload on the PV loop?
|
Its the line from the top left "corner" to the EDV on the x axis. The greater the angle (more upright the line) the greater the afterload
|
|
|
|
What would cause the endsystolic PV line to have an increased slope?
|
if contractiltiy was increased, like with and adrenaline rush
|
|
|
|
着る
Kiru |
To be wearing
|
きる
|
|
|
Factors that determine preload
|
Ventricular filling time
Ventricular compliance Filling pressure Contribution of atrial systole to filling Pericardial constraint |
|
|
|
Preload in absence of sympathetic stimulation has what effect on cardiac output?
|
– CO usually not affected since decreased SV compensated for by increased HR.
– CO adversely affected at HR > 150 to 180 BPM. |
|
|
|
Preload With sympathetic stimulation has what effect on cardiac output?
|
With sympathetic stimulation:
– SV preserved due to increased contractility – CO can increase dramatically. (associate with exercise) |
|
|
|
Decreasing intrathoracic pressure (inspiration) will have what affect on stroke volume and preload?
|
Increase RIGHT ventricular SV & Preload, which increase
|
|
|
|
Increasing central venous pressure will have what affect on stroke volume and preload?
|
Increase RIGHT ventricular SV & Preload
|
|
|
|
How much does atrial kick contribute to EDV?
|
20-30% but has greater impact when filling times are reduced
|
|
|
|
Effect of cardiac tamponade on cardiac cycle...
|
reduces ventricular compliance, reduces EDV, reduces SV
|
|
|
|
Factors that affect Afterload
|
– arterial pressure
– peripheral vascular resistance (PVR) – arterial wall compliance – mass of the column of blood in the aorta – viscosity of the blood |
|
|
|
How is afterload measured?
|
Estimated by mean arterial pressure (= DP + 1/3 PP)
|
|
|
|
What is the reelationship between the afterload and SV and maximum velocity of ejection?
|
Inverse
if afterload is bigger (greater resistance) it will decrease volume and velocity |
|
|
|
An increased afterload w/ a constant EDV will cause what changes in the PV loop?
|
– increased ESV
– reduction in SV |
|
|
|
Clinically, afterload is increased by what pathologies.factors?
|
– aortic stenosis
– elevated arterial pressure – ↑ PVR – ↑ blood viscosity – ↓ arterial compliance |
|
|
|
What is Systole?
|
contraction of a chamber and blood is being ejected (contraction and emptying)
|
|
|
|
What is Diastole?
|
period of relaxation during which the chamber is filling (relaxation and filling) and coronary arteries are perfused
|
|
|
|
When are the coronary arteries perfused?
|
During relaxation/diastole.
Coronary blood flow (70%) Diastole and 30% during systole. |
|
|
|
What are the phases of the cardiac cycle?
|
A: Atrial systole
B: Isovolumetric contraction C: Rapid ejection D: Reduced ejection E: Isovolumetric relaxation F: Rapid filling G: Reduced filling |
|
|
|
For the given phase, what are the valves doing and what phase is the left ventricle in?
A: Atrial systole |
AV Valves Open
Diastole |
|
|
|
For the given phase, what are the valves doing and what phase is the left ventricle in?
B: Isovolumetric contraction |
Closing of AV valves (all 4)
Systole |
|
|
|
For the given phase, what are the valves doing and what phase is the left ventricle in?
C: Rapid ejection |
Opening of SL valves
Systole |
|
|
|
For the given phase, what are the valves doing and what phase is the left ventricle in?
D: Reduced ejection |
Opening of SL valves
Systole |
|
|
|
For the given phase, what are the valves doing and what phase is the left ventricle in?
E: Isovolumetric relaxation |
Closing of SL valves (all 4)
Diastole |
|
|
|
For the given phase, what are the valves doing and what phase is the left ventricle in?
F: Rapid filling & G: Reduced Filling |
Diastole
Opening of AV valves |
|
|
|
At what phase might a 4th heart sound be heard?
|
During Atrial Systole
caused by vibration of ventricular walls noted when ventricular compliance is reduced, as in LV hypertrophy, MI, or ischemic heart disesase |
|
|
|
What are the values for EDV for normal, atheletic and heart failure patients?
|
) Normal: ~120 ml
) Endurance athletes: ~180-240 ml ) Heart failure: ~180-240 ml |
|
|
|
When does the mitral valve close on the cardiac cycle chart? What else does this point signify?
|
at end of atrial systole (part a)
Also the point of EDV (can't fill anymore, valves closed) |
|
|
|
What phase is the S1 sound heard? What causes it?
|
During Isovolumetric contraction causes Rise in pressure causes the AV valves to close,
|
|
|
|
What's happening During Isovolumetric contraction?
|
depolarization leads to a rapid
increase in LV pressure Pressure rises without a change in blood volume |
|
|
|
What phase of the EKG corrosponds with Isovolumetric contraction?
|
QRS
|
|
|
|
What phase of the EKG corrosponds with atrial systole?
|
P wave
|
|
|
|
What happens to Isovolumetric contraction and relaxation under sympathetic control?
|
rates of pressure development
and dissipation are increase |
|
|
|
What happens in the rapid ejection phase?
|
When intraventricular pressures
exceeds pressures within the great vessels, pulonic/aortic valves open and blood is ejected Maximal LV systolic and RV systolic pressure is achieved Atrial filling begins |
|
|
|
the rapid ejection phase corrosponds to what on the ekg?
|
End of this phase coincides with the end of the ST segment
|
|
|
|
What happens in the reduced ejection phase?
|
Ventricles begin to repolarize
Blood continues to be ejected due to inertial energy of blood Atrial pressure continue to rise due to venous return |
|
|
|
What part of the EKG corrosponds to the reduced ejection phase?
|
T wave
|
|
|
|
When is the S2 sound heard?
|
Isovolumetric relaxation when LV pressure drops below vessel pressure and aortic and pulmonic valves to close
|
|
|
|
In what phase is the ESV found? What is it approximatly?
|
Isovolumetric relaxation
(ESV) is ~ 50 ml |
|
|
|
What causes splitting of S2 sound?
|
Inspiration causes splitting of S 2 (A 2 P 2 ) During the isovolumetric relaxation, the aortic valve closes before the pulmonary valve
|
|
|
|
What happens during rapid filling phase?
|
Ventricular pressures fall below
atrial pressures; AV valves open; LV filling begins |
|
|
|
When might you hear a 3rd sound?
|
Durong rapid ventricular filling phase
indicates recoil of blood against LV wall--sudden deceleration of flow |
|
|
|
What is the longest phase of the cardiac cycle?
|
Reduced ventricular filling
|
|
|
|
What happens in the Reduced ventricular filling phase?
|
Final portion of the passive ventricular filling
As ventricles continue to fill with blood and expand, compliance decreases This reduces the pressure gradient across the AV valves rate of filling therefore falls Increase in heart rate decreases the time available for this phase |
|
|
|
What phase of the cardiac cycle might get shortened in an increase HR situation
|
Reduced ventricular filling phase
|
|
|
|
What are peaks a,c,v?
|
venous pulses that occur in the right atrium that are transmitted as peaks in the large veins
|
|
|
|
What/when occuring:
a wave |
Occurs during atriol systole:
atrial contraction increase right atrial pressure and reflected back to the veins |
|
|
|
What/when occuring:
c wave |
Rapid ejecting phase
Caused by bulging of the tricuspid valve into the right atrium during ventricular systole |
|
|
|
What/when occuring:
v wave |
(isovolumic relaxation)
filling of central veins and right atrium behind a closed tricuspid |
|
|
|
Which opens first, pulmonary or aortic valve?
|
Pulmonary
(less pressure to overcome?) |
|
|
|
Which closes first, pulmonary or aortic valve?
|
aortic
greater pressure pulmonary |
|
|
|
Which opens first, tricuspid or mitral?
|
tricuspid
|
|
|
|
Which measurement is an indicator of contractiltiy?
|
Ejection fraction
|
|
|
|
When might S4 be heard?
|
heard during atrial systole where ventricular compliance is decreased as in ventricular hypertrophy
|
|
|
|
What pathological conditions can widen S 2?
|
pulmonic stenosis
right ventricular failure right bundle branch block |
|
|
|
What Pathology can cause S2 split to narrow or disappear?
|
Left bundle branch block
Delayed depolarization of left ventricle Aortic stenosis |
|
|
|
Whats a pradoxical split?
|
When P2 is heard before A2 i
>severe aortic stenosis |
|
|
|
What are most common causes of
turbulence? |
Valve dysfunctions
stenotic valve insufficient (regurgitant) valve |
|
|
|
Whats a stenotic valve?
|
stiff narrow valve that does not open completely
turbulence created when blood must be forced through |
|
|
|
What's an insufficient valve?
|
One that does not completly close
blood flows backwards and collides with incoming blood |
|
|
|
Whats a systolic murmur?
|
heard during systole or after S1
|
|
|
|
What are possible causes of systolic murmurs?
|
aortic or pulmonary valve stenosis
mitral or tricuspid regurg |
|
|
|
Whats a midsystolic murmur?
|
crescendo decrescendo character
caused by aortic or pulmonary valve stenosis |
|
|
|
Whats a holostolic murmur?
|
caused by AV valve regurgitation or ventricular septal defect
|
|
|
|
Whats a diastolic Murmur?
|
murmur heard after S2
|
|
|
|
What are causes of diastolic murmurs?
|
atrial and pulmonary regurg
tricuspid or mitral stenosis |
|
|
|
What causes mitral stenosis?
|
rheumatic heart disease.
congenital lesions, calcium depositions, and myxoma |
|
|
|
What are the effects of aortic stenosis on the heart?
|
narrowing of vessel makes LV have to contract harder increasing LVP and causing hypertophy of the heart and eventual failure
|
|
|
|
What are the effects of mitral valve stenosis on the cardiac cycle?
|
LAP is greater than LVP during filling
atrial have to contract harder, and left ventricles fill less. increase in pressure leads to pulmonary congestion |
|
|
|
What are the effects of aortic regurgitation on the cardiac cycle?
|
blood flow back iont left ventricle increasing preload which increase stroke volume
atria get back up as ventricles get backed up |
|
|
|
What causes a widening pulse pressure/
|
aortic regurge
|
|
|
|
What are the effects of mitral regurge on the cardiac cycle?
|
Regurgitant flow from left ventrical goes back int left atrium.
This decreases LVSV and causes enlargement of the atrial chamber Can lead to venous congestion |
|
|
|
What is main feature of Atrial Flutter?
|
P wave rate greater than 250 bpm
|
|
|
|
What are the features of Atrial Fibrillation?
|
•No discrete P-waves
|
|
|
|
What are the features Ventricular Fibrillation?
|
• random waveforms
• unidentifiable QRS |
|
|
|
What are the features Long QT Syndrome?
|
Prolonged interval between QRS &
T-wave. |
|
|
|
Ribbon looking EKG characterized by rapid ventricular rhythm.
|
Tosades de Pointes
|
|
|
|
Main characteristic of atrial tacycardia
|
rapid atrial rate (150-250)
P waves uniform Narrow QRS |
|
|
|
Main characteristic of Atrial Fibrilation?
|
Always irregular R-R
|
|
|
|
Main characteristic of junctional rhythms
|
Absent or inverted p waves
|
|
|
|
Main characteristic of ventricular rhythms
|
WIDE QRS (>.10 s)
|
|
|
|
Main characteristic of 1* AV block
|
Prolonged P-R interval (>.20s)
P:QRS 1:1 |
|
|
|
Main characteristic of Mobitz I
|
PR increasingly longer
P:QRS ratio variable |
|
|
|
Main characteristic of Mobitz II
|
PR fixed
P:QRS ratio variable, not all P's married to QRA |
|
|
|
Main characteristic 3* block
|
Reg PP
Reg RR Changing PR |
|

