![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
|
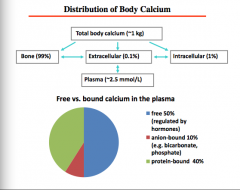
What is the distribution of total body Ca2+?
Bone Extracellular (plasma) Intracellular
What percent is free, anion-bound, and protein bound? |
|
|
|
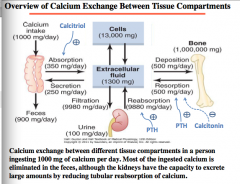
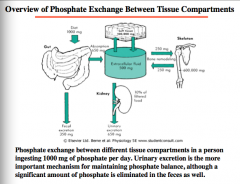
Calcium in extracellular fluid: 1300mg
Amount exchanged between bone, urine, calcium intake, intestines, etc.
Draw the pathways
What happens to most ingested calcium? |
|
|
|
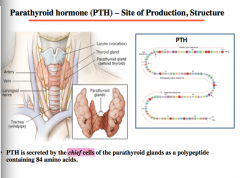
What cells secrete PTH? |
|
|
|
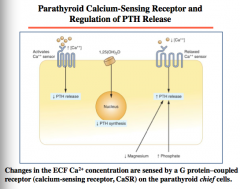
What are changes in ECF Ca2+ concentration sensed by? On what cells?
What is the effect of calcitriol (1,25 OH2D) on PTH synthesis?
What are the effect of magnesium and phosphate on PTH release?
|
Mg competes with calcium, just with lower affinity |
|
|
What is the affect of plasma Ca2+ on PTH and calcitonin levels? |

|
|
|
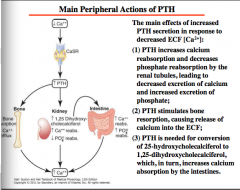
Draw the pathway of the effect of decrease in Ca2+ on CaSR and PTH on bone, kidney, and intestine.
Think about effects on Ca reabsorption, PO4, and 1,25 dihydroxycholecalciferol |
|
|
|
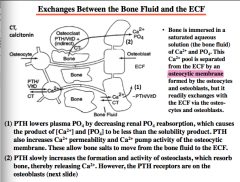
What is the Ca2+ and PO4 separated from the ECF by? What two cells form this?
How does PTH lower plasma PO4? What effect does PTH have on osteocytic membrane? What does this allow? (bone salts move from ______ to _______).
PTH slowly increases the formation and activity of ________, which resorb bone, thereby increasing Ca2+. Where are the PTH receptors located? |
|
|
|
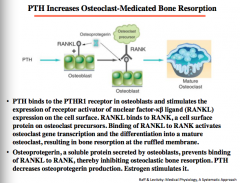
Draw the pathway of PTH involvement in osteoclast-mediated bone resorption.
What receptor bound? On what cells? Stimulation of what on cell surface? This then binds to what cells? What becomes activated? Differentiation into mature what?
What can prevent binding of RANKL to RANK, thereby inhibiting osteoclastic bone resorption? Does PTH increase or decrease production of this? What hormone stimulates it? |
|
|
|
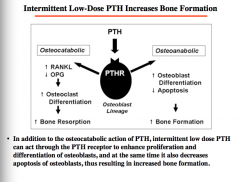
What can intermittent low dose PTH enhance? (opposite of what we normally think). |
|
|
|
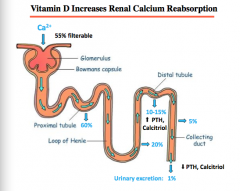
How much of Ca2+ is filterable? What percent is reabsorbed in proximal tubule?
What parts of calcium reabsorption can be regulated by PTH? |
Reabsorption in distal tubule... |
|
|
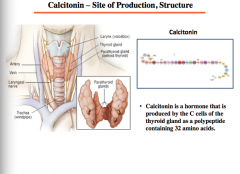
Where is calcitonin produced? What cells? |
|
|
|
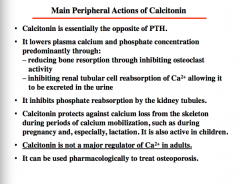
Calcitonin is essentially the opposite of _______.
Effect on plasma calcium and phosphate concentration? Through what two mechanisms?
What does it inhibit in the kidney tubules?
What does it protect against?
Is it a major regular of Ca2+ in adults?
What can it be used pharmacologically to treat? |
|
|

Draw this. |

|
|
|
What is the pathway of vitamin D synthesis? Effect on what 4 organs?
1-alpha hydroxylase is activated by what? Inhibited by what two things?
24-alpha hydroxyls activated by what three things? |

|
|
|
Provitamin D (7-dehydrocholesterol) in the skin is converted to _____________ by UV light. Cholecalciferol and ergocalciferol (from plants) are transported to the __________, where they undergo the first step in bioactivation, which is the hydroxylation at C-25 to ________________, the major circulating form of vitamin D. The second hydroxylation step, at C-1, occurs in the ______________ and results in the hormonally active_______________. This activation step is mediated by ____________. 1α-hydroxylase is stimulated by __________ and inhibited by ____________ and__________. Decreased activity of 1α-hydroxylase favors C-24 hydroxylation and formation of the less active ______________. 1,25(OH)2D __________ bone resorption, increases _________ absorption from the intestine (the major effect), __________ renal calcium reabsorption, and __________ the production of PTH by the parathyroid glands. The overall effect of 1,25(OH)2D3 is to __________ plasma [Ca2+]. |
Provitamin D (7-dehydrocholesterol) in the skin is converted to cholecalciferol by UV light. Cholecalciferol and ergocalciferol (from plants) are transported to the liver, where they undergo the first step in bioactivation, which is the hydroxylation at C-25 to 25-hydroxy- vitamin D (25OHD3), the major circulating form of vitamin D. The second hydroxylation step, at C-1, occurs in the kidney and results in the hormonally active 1,25(OH)2D3 (a.k.a. calcitriol). This activation step is mediated by 1α-hydroxylase. 1α-hydroxylase is stimulated by PTH and inhibited by calcium and 1,25(OH)2D3. Decreased activity of 1α-hydroxylase favors C-24 hydroxylation and formation of the less active 24,25(OH)2D3. 1,25(OH)2D increases bone resorption, increases calcium absorption from the intestine (the major effect), increases renal calcium reabsorption, and decreases the production of PTH by the parathyroid glands. The overall effect of 1,25(OH)2D3 is to increase plasma [Ca2+]. |
|
|
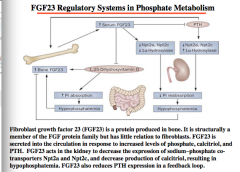
What is the main function of FGF23? |
Decreases phosphate reabsorption and increases phosphate excretion = > lower phosphate levels |
|
|
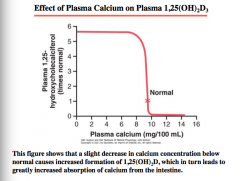
What is the effect of calcium on plasma 1,25-hydroxycholecalciferol levels? |
|
|
|
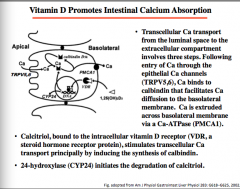
What are the three steps of transcellular transport of Ca2+ from the luminal space to the extracellular compartment?
Entry => binding => extruded how?
What hormone stimulates transcellular Ca transport by inducing synthesis of calbindin?
What enzyme initiates the degradation of calcitriol?
|
|
|
|
What is the effect of vitamin D on renal calcium reabsorption? |
|
|
|
How is phosphate most commonly found?
What is bone a precipitate of?
|
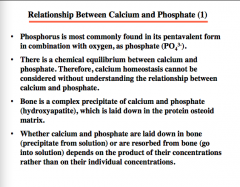
|
|
|
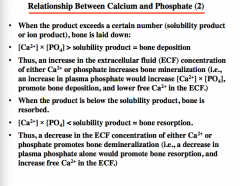
What determines bone deposition (general calcium phosphorus and solubility product relationship)?
Increase in what two EC things increases bone mineralization?
When product is below solubility product, bone is __________.
Decrease in ECF concentration of either Ca2+ or phosphate promotes bone _________.
|
|
|
|
Phosphate is used in the formation of what two things?
What three things is it a component of?
Intracellular or extracellular ion?
|

|
|
|
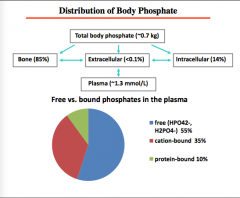
Draw the distribution of phosphate.
Total body phosphate
Bone, extracellular (plasma), intracellular
Free, cation bound, protein bound |
|
|
|
What is the most important mechanism for maintaining phosphate balance? |
|
|
|
How is phosphate metabolism affected in kidney failure? |
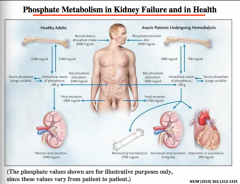
Removed by hemodialysis Decreased renal excretion Deposition in vasculature |
|
|
Where is FGF23 produced? Effect on 1-alpha hydroxyls? Effect on 1,25 dihydroxyvitaminD? Effect on Pi reabsorption => bone? |
|
|
|
How much of P is filterable? Where does most reabsorption occur? |
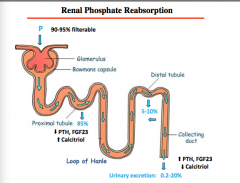
|
|
|
Which symptom is most common in patients with chronic kidney failure? |
Hyperphosphatemia
Could also have hypercalcemia also. |
|
|
What is likely to be the major consequence of this hyperphosphatemia? |
Secondary hyperparathyroidism |

