![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
184 Cards in this Set
- Front
- Back
|
G-protein receptor mnemonic
|
Kiss (QISS) and kick (QIQ) until your sick (SIQ) of sex (SQS).
Q = Gq(-> PLC -> IP3, DAG), S = Gs(-> +adenylate cyclase -> cAMP) , I = Gi ( -> -adenylate cyclase). Q(alpha1)I(alpha2)S(beta 1)S(beta 2) Q(M1/muscarinic Ach 1)I(M2)Q(M3) S(Dopamine 1)I(Dopamine 2)Q(Histamine 1) S(Histamine 2)Q(Vasopressin 1)S(Vasopressin 2) (Epinephrine(4)-Muscarinic(3)-Dopamine(2)-Histamine(2)-Vasopressin(2)) |
|
|
Aldosterone - stimuli for secretion
|
RNAs: Renin-angiotensin system, Na-concentration in blood, ANP, Stress
|
|
|
Effect of ACTH
|
Effects of ACTH
1. Stimulate glucorticoid release 2. Can stimulate androgen release 3. Permissive effect on mineralocorticoid (Netter fcards) |
|
|
Identify the substances that act on the hypothalamus to contribute to negative feedback regulation of GH (5)
|
1. GH
2. IGF-1 3. Hyperglycemia 4. FFA 5. GHIH (Netter fcards) |
|
|
Name the hypothalamic and anterior pituitary hormones controlling estrogen secretion
|
1. Hypothalamic GnRH ->↑LH, ↑FSH
2a. LH -> ↑Androgen production by theca interna cells 2b. FSH -> aromatization of these androgens to estradiol in the granulosa cells (Netter fcards) |
|
|
In addition to T3 and T4, which other two hormones can exert negative feedback on TSH
|
1. Cortisol
2. GH (Netter fcards) |
|
|
Describe the 6 steps in thyroid hormone synthesis
|
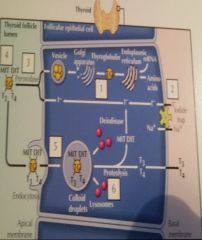
1. Thyroglobulin molecules are produced in the golgi apparatus and exocytosed into the follicular lumen
2. Iodide enter the cell through Sodium-iodide symporter (Iodide trap) and exits the cell into the lumen of the follicle (by pendrin\sodium-independent chloride\iodide transporter (also found in cortical collecting duct)) 3. Thyroid peroxidase: (inhibited by thioamide drugs: propylthiouracil, methimazole)(epitope in Hashiomoto's thyroiditis) a. Iodide -> iodine, b. Then iodine is substituted for the H+ on the benzene ring of tyrosine residues of thyroglobulin giving MIT (monoiodotyrosine) and DIT 4. Thyroid peroxidase: DIT + DIT -> T4, DIT + MIT -> T3 5. The mature thyroglobulin (containing DIT, MIT, T4, T3) is endocytosed and stored 6. TSH: lysosomal proteolysis of the thyroglobulin -> a. Release of T4, T3 to blood b. Reentry of MIT and DIT to synthetic pool (Netter fcards) |
|
|
Effect of TSH
|
Effect of TSH - Affect all the steps
1. Thyroglobulin synthesis 2. Sodium-iodide symporter 3. Tyrosine peroxidase 4. Lysosomal proteolysis of mature thyroglobulin (Random internet powerpoint) |
|
|
Thyroid hormones
a. Effect of TSH b. Major form of circulating TH c. Active form d. Effect |
a. Effect of TSH - Affect all the steps of thyroid hormone synthesis
1. Thyroglobulin synthesis 2. Na-I symporter 3.Tyrosine peroxidase 4. Lysosomal proteolysis of mature thyroglobulin b. T4 (20x more than T3) c. T3 (T4 is deiodinated intracellularly by 5'-deiodinase) d. ↑Metabolism (↑Mitochondria activity, respiratory enzymes, Na+-K+-ATPase, other enzymes, O2 consumption) (Netter fcards) |
|
|

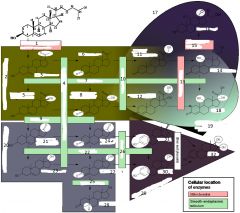
1. cholesterol side-chain cleavage enzyme\cholesterol desmolase
2. progestagens, 21 carbons 3. pregnenolone 4. 3-beta-hydroxysteroid dehydrogenase 5. 17-alpha-hydroxypregnenolone 6. Progesterone 7. 17-alpha-hydroxylase 8. 17-alpha-hydroxyprogesterone 9. 17,20-lyase 10. 21-alpha-hydroxylase 11. 11-deoxycorticosterone 12. 11-deoxycortisol 13. 11-beta-hydroxylase 14. Corticosterone 15. Aldosterone synthase 16. Aldosterone 17. Mineralocorticoids, 21 carbons 18. Cortisol 19. Glucocorticoids, 21 carbons 20. Androgens, 19 carbons 21. Dehydroepiandrosterone 22. 17-beta-hydroxysteroid dehydrogenase 23. Androstenediol 24. Androstenedione 25. 5-alpha-reductase 26. Aroamtase 27. Testosterone 28. Dihydrotestosterone 29. Estrogens, 18 carbons 30. Estradiol 31. Estrone 32. estriol |
|
|
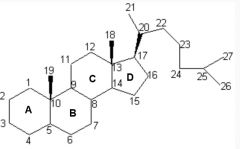
Draw cholesterol with numbers
|
|
|
|
C\Connecting-peptide
a. What b. Clinical application |
a. Peptide connecting A and B chain of proinsulin, its cleaved in Golgi apparatus and secreted with insulin
b. Reflect endogenous insulin production (Netter fcards) |
|
|
Synthesis of vitamin D
a. Steps in skin, liver, and kidney b. Which step do PTH influence |
a. Synthesis of Vitamin D
1. Skin - Ultraviolet light - 7-Dehydroxycholesterol -> cholecalciferol 2. Liver. <- skin, dietary intake Cholecalciferol -> 25-hydroxycholecalciferol 3. Kidney - 25-hydroxycholecalciferol -> 1,25-dihydroxycholecalciferol (active form) b. PTH influence renal 1-alpha-hydroxylase (Netter fcards) |
|
|
PTH - effect
a. In small intestine b. In kidneys c. In bone |
a. Effect of PTH in small intestine
Indirectly via activating vitamin D (Vitamin D increase Ca+ and Pi absorption by ↑Calbindin and basolateral Ca2+-ATPase) b. Effect of PTH in kidneys 1. ↑Ca2+ reabsorption in distal tubule 2. ↓Pi reabsorption proximal tubule 3. ↑renal 1-alpha-hydroxylase (vitamin D) c. Effect of PTH in bone ↑Osteoclast activity -> ↑Ca+, ↑Pi (Netter fcards) |
|
|
Testicular function
a. Name the hormone produced by the Sertoli cells that has negative effects on pituitary FSH secretion b. Name the 2 hormones involved in spermatogenesis and describe how |
a. Inhibin
b. The 2 hormones involved in spermatogenesis 1. FSH stimulate Sertoli cells which facilitate spermatogenesis and produce androgen-binding protein (↑Concentration of androgens in seminiferous tubules) 2. Testosterone from Leydig cells stimulate spermatogenesis and binds to androgen-binding protein (Netter fcards) |
|
|
XY embryo ->-> vas deferens and no falloopian tubes?
|
1. SRY (Sex determining region Y) gene -> Testis determining factor (TDF)
2. Testis -> a. Testosterone (week 8) -> Differentiation of Wolffian duct\Mesonephric duct to vas deferens b. Mullerian-inhibiting factor -> degeneration of Mullerian duct (which become Fallopian duct in female) (Female: absence of Mullerian inhibiting factor cause persistence & differentiation of Mullerian duct, Absence of testosterone cause degeneration of Wolffian duct) (Netter fcards) |
|

|

|
|

|
|
|

|

|
|
|
Calorimetry
a. Caloric value of carbohydrates b. Caloric value of fats c. Caloric value of proteins d. Which has not the same value in direct calorimetry (bomb calorimeter) and the body |
a. 4.1 kcal\g
b. 9.3 kcal\g c. 4.1 kcal\g d. Protein (5.3 kcal\g in direct calorimetry, less in the body due to incomplete combustion (urea)) (Ganong) |
|
|
Calorimetry
a. Method for indirect calorimetry b. Respiratory quotient (RQ) c. Respiratory quotient (RQ) for carbohydrate, protein, and fat d. How can an approximation of carbohydrate vs fat vs protein metabolism in the body be derived from this |
a. Measure oxygen consumption
(O2 is not stored, and except when an O2 debt is being incurred, the amount of O2 consumption per unit of time is proportionate to the energy liberated by metabolism) (Direct calorimetry is based on measuring temperature of water inside an isolated unit after combustion) (4.82 kcal\L O2 consumed) b. Respiratory quotient (RQ) I. The ratio of volume of CO2 produced to the volume of O2 consumed per unit time, during steady state c. Respiratory quotient I. Carbohydrate - 1.0 II. Fat - 0.7 (H and O are present in carbohydrate in the same proportions as in water, whereas in the various fats, more oxygen is necessary for the formation of H2O (\Less O in fat)) III. Protein - 0.83 d. Use RQ and the urinary nitrogen excretion (Can determine RQ of organs by multiplying their blood flow per unit of time by the AV difference for O2 and CO2 across the organ) (Ganong) |
|
|
Metabolic rate
a. Specific dynamic action (SDA) b. Basal metabolic rate (BMR) c. Maximum metabolic rate |
a. Specific dynamic action (SDA)
I. The increase in metabolic rate due to assimilation of food into the body, protein has 5x as high SDA as carbohydrate and 6x as high SDA as fat b. Basal metabolic rate (BMR) I. The metabolic rate determined at rest in a room at a comfortable temperature in the thermoneutral zone 12-14 hours after the last meal (10% lower during sleep, 40% lower during starvation) c. Maximum metabolic rate I. Peaks during exercise II. 10x normally, can reach 20x in trained athletes (Ganong) |
|
|
Metabolism
a. Intermediary metabolism b. High-energy compounds c. Average use of ATP |
a. Intermediary metabolism
I. The metabolism of the end products of digestion - Amino acids, fat derivatives, and monosaccharides (Stedman - The sum of all metabolic reactions between uptake of foodstuffs and formation of excretory products) b. High-energy compounds 1. ATP 2. Creatine phosphate 3. Thioesters - Acyl derivatives of mercaptans\thioalcohol I. Coenzyme A (Mercaptan-containing adenine, ribose, panthotenic acid, and thioethanolamine, forms activated compounds ie acetyl CoA) c. ATP I. Protein synthesis - 27% II. Na-K-ATPase - 24% (70% in neurons) III. Gluconeogenesis - 9% IV. Ca-ATPase - 6% V. Myosin ATPase - 5% VI. Ureagenesis - 3% (Ganong) |
|
|
Carbohydrate metabolism
a. Glycolysis synonym b. Connections between the products of fructose biphosphate aldolase c. How does epinephrine regulate glycogen metabolism d. McArdle's disease |
a. Embden-Meyerhof pathway
b. Fructose biphosphate aldolase : Fructose 1,6-BP -> 1. Dihydroxyacetone phosphate I. <-> alpha-glycerophosphate <--> glycerol (from fats) 2. Phosphoglyceraldehyde I. <- Hexose monophosphate shunt\pentose phosphate pathway c. Epinephrine - Glycogen metabolism 1. Beta-2 adrenergic receptor in liver and skeletal muscle -> 2. Gs -> adenylate cyclase -> cAMP -> 3. Protein kinase A -> 4a. Inhibit glycogen synthesis by phosphorylating glycogen synthase 4b. Activate phosphorylase kinase b -> 5b. Phosphorylase kinase b activate phosphorylase a 6.. Phosphorylase break 1:4alpha bonds between glucose residues (Also same result by alpha-1 adrenergic receptors. Acitvate phosphorylase kinase b via increased Ca) (Glucagon only activates Gs in the liver) d. McArdle's syndrome\Myophosphorylase deficiency glycogenosis I. Glycogen accumulates in skeletal muscle because of a deficiency of muscle phosphorylase (Patients have muscle pain and stiffness on exertion and a greatly reduced exercise tolerance) (Ganong) |
|
|
Energy stores in a 70 kg man
a. Carbohydrates b. Fat |
a. Carbohydrate
1. 2500 kcal I. 400g in muscle II. 100g in liver III. 20g in ECF b. Fat I. 110 000 kcal (80% of energy supplies, the remaining 20% is stored in protein) (The brain use 70-80% of glucose during resting state and red blood cells account for most of the rest) (Ganong) |
|
|
Protein
a. Selenocysteine b. Amino acids formed by posttranslational modification c. Amino acids which are found in the body but not in incorporated into protein |
a. Selenocysteine
I. Rare amino acid in which the sulfur of cysteine is replaced with selenium II. The codon UGA is usually a stop codon, but in certain situations it codes for selenocysteine b. Amino acids formed by posttranslational modification 1. Gamma-carboxyglutamic acid (Clotting factors) 2. Hydroxylysine (Collagen) 3. 4-Hydroxyproline (Collagen, elastin) c. 1. Ornithine 2. 5-Hydroxytryptophan (Serotonin) 3. L-Dopa 4. Taurine 5. Thyroxine (Ganong) |
|
|
Creatine and creatinine
a. Creatine - Synthesized where, made of b. Creatinuria - Physiological causes c. Creatinuria - Pathological causes |
a. Creatine
I. Synthesized in the liver and phosphorylated to creatine phosphate\phosphorylcreatine in skeletal muscle (The creatinine in urine is formed from phosphorylcreatine. The rate of creatinine excretion is relatively constant from day to day) II. Made of methionine, glycine, and arginine b. Creatinuria - Physiological causes 1. Children 2. Women during and after pregnancy 3. Occasionally in non-pregnant women (Very little, if any, creatine is present in the urine of normal men) c. Creatinuria - Pathological causes - Any condition with extensive muscle breakdown 1. Primary and secondary myopathies 2. Starvation 3. Thyrotoxicosis 4. Poorly controlled diabetes mellitus (Ganong) |
|
|
Uric acid
a. Formed from b. Mechanism of excretion c. Primary gout - What, causes d. Secondary gout - What, causes e. Pharmacological treatment |
a. Uric acid sources
1. Adenosine --> I. Hypoxanthine --Xanthine oxidase--> II. Xanthine --Xanthine oxidase--> III. Uric acid 2. Guanosine --> I. Xanthine --Xanthine oxidase--> II. Uric acid 3. From 5-PRPP + Glutamine (5-phosphoribosyl pyrophoshate) (Xanthine oxidase is inhibited by allopurinol) b. Excretion - Renal I. 80% of the excretion results from reabsorption followed by secretion II. 20% of the excretion results from non-reabsorption (98% of the filtrate is not reabsorbed) c. Primary gout - Gout caused by I. Increased uric acid production due to various enzyme abnormalities II. Deficit in renal tubular transport of uric acid d. Secondary gout - The uric acid levels in the body fluids are elevated as a result of decreased excretion or increased production secondary to some other disease process I. Thiazide diuretics decrease secretion II. Renal disease decrease secretion III. Production is increased in leukemia because of increased breakdown of uric-acid rich white blood cells IV. Pneumonia --||-- e. Pharmacological treatment 1. Colchicine (Relieves gouty attacks by inhibiting the phagocytosis of uric acid crystals by leukocytes, a process that in some way produces the joint symptoms) 2. Phenylbutazone and probenecid (Inhibit renal tubular reabsorption) 3. Allopurinol (Inhibit xanthine oxidase) (S&S - Recurrent arthritis most often in MPJ of great toe, urate deposits in joints, kidneys.., elevate blood and urine uric acid levels) (Ganong) |
|
|
Fats - Constituents of
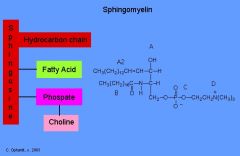
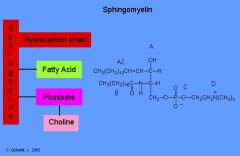
Phospholipids a. Phospholipids made of esters of glycerol, two fatty acids and x b. Sphingomyelin - Components c. Cerebrosides - Components |
a. Phospholipids made of esters of glycerol, two fatty acids, and x
1. Phosphatidic acid (x = Phosphate) 2. Phosphatidylinositol (x = Phosphate and inositol) 3. Phosphatidylcholine\Lecithin (x = Phosphate, choline) 4. Phosphatidylethanolamine\cephalin (x = Phosphate, ethanolamine) 5. Phosphatidylserine (x = Phosphate, serine) b. Sphingomyelin I. Sphingosine backbone (Amino alcohol) II. Ester of fatty acid III. Phosphate and choline c. Cerebrosides I. Sphingosine backbone II. Fatty acid ester III. Galactose (Ganong) |
|
|
Energy stores in a 70 kg man
a. Carbohydrates b. Fat |
a. Carbohydrate
1. 2500 kcal I. 400g in muscle II. 100g in liver III. 20g in ECF b. Fat I. 110 000 kcal (80% of energy supplies, the remaining 20% is stored in protein) (The brain use 70-80% of glucose during resting state and red blood cells account for most of the rest) (Ganong) |
|
|
Protein
a. Selenocysteine b. Amino acids formed by posttranslational modification c. Amino acids which are found in the body but not in incorporated into protein |
a. Selenocysteine
I. Rare amino acid in which the sulfur of cysteine is replaced with selenium II. The codon UGA is usually a stop codon, but in certain situations it codes for selenocysteine b. Amino acids formed by posttranslational modification 1. Gamma-carboxyglutamic acid (Clotting factors) 2. Hydroxylysine (Collagen) 3. 4-Hydroxyproline (Collagen, elastin) c. 1. Ornithine 2. 5-Hydroxytryptophan (Serotonin) 3. L-Dopa 4. Taurine 5. Thyroxine (Ganong) |
|
|
Creatine and creatinine
a. Creatine - Synthesized where, made of b. Creatinuria - Physiological causes c. Creatinuria - Pathological causes |
a. Creatine
I. Synthesized in the liver and phosphorylated to creatine phosphate\phosphorylcreatine in skeletal muscle (The creatinine in urine is formed from phosphorylcreatine. The rate of creatinine excretion is relatively constant from day to day) II. Made of methionine, glycine, and arginine b. Creatinuria - Physiological causes 1. Children 2. Women during and after pregnancy 3. Occasionally in non-pregnant women (Very little, if any, creatine is present in the urine of normal men) c. Creatinuria - Pathological causes - Any condition with extensive muscle breakdown 1. Primary and secondary myopathies 2. Starvation 3. Thyrotoxicosis 4. Poorly controlled diabetes mellitus (Ganong) |
|
|
Uric acid
a. Formed from b. Mechanism of excretion c. Primary gout - What, causes d. Secondary gout - What, causes e. Pharmacological treatment |
a. Uric acid sources
1. Adenosine --> I. Hypoxanthine --Xanthine oxidase--> II. Xanthine --Xanthine oxidase--> III. Uric acid 2. Guanosine --> I. Xanthine --Xanthine oxidase--> II. Uric acid 3. From 5-PRPP + Glutamine (5-phosphoribosyl pyrophoshate) (Xanthine oxidase is inhibited by allopurinol) b. Excretion - Renal I. 80% of the excretion results from reabsorption followed by secretion II. 20% of the excretion results from non-reabsorption (98% of the filtrate is not reabsorbed) c. Primary gout - Gout caused by I. Increased uric acid production due to various enzyme abnormalities II. Deficit in renal tubular transport of uric acid d. Secondary gout - The uric acid levels in the body fluids are elevated as a result of decreased excretion or increased production secondary to some other disease process I. Thiazide diuretics decrease secretion II. Renal disease decrease secretion III. Production is increased in leukemia because of increased breakdown of uric-acid rich white blood cells IV. Pneumonia --||-- e. Pharmacological treatment 1. Colchicine (Relieves gouty attacks by inhibiting the phagocytosis of uric acid crystals by leukocytes, a process that in some way produces the joint symptoms) 2. Phenylbutazone and probenecid (Inhibit renal tubular reabsorption) 3. Allopurinol (Inhibit xanthine oxidase) (S&S - Recurrent arthritis most often in MPJ of great toe, urate deposits in joints, kidneys.., elevate blood and urine uric acid levels) (Ganong) |
|
|
Fats
Phospholipids a. Phospholipids made of esters of glycerol b. Other phospholipids Others c. Cerebrosides - Components |
a. Phospholipids made of esters of glycerol, two fatty acids and x
1. Phosphatidic acid (x = Phosphate) 2. Phosphatidylinositol (x = Phosphate and inositol) 3. Phosphatidylcholine\Lecithin (x = Phosphate and choline) 4. Phosphatidylethanolamine\Cephalin (x = Phosphate and ethanolamine) 5. Phosphatidylserine (x = Serine) b. Other phospholipids 1. Sphingomyelins (Amino alcohol sphingosine as backbone, ester of a fatty acid, and phosphate-choline) c. Cerebrosides I. Sphingosine backbone II. Ester of fatty acid III. Galactose (Ganong) |
|
|
Lipoproteins - Exogenous system
a. Apoproteins b. Chylomicrons - Origin, relative composition, apoproteins, fate c. Chylomicron remnants - Origin, apoproteins, fate |
a. Apoproteins
I. The protein constituents of lipoproteins II. The major ones are called APO E, APO C, and APO B. APO B has two forms - APO B-48, a lower molecular-weight form which is characteristic of the exogenous system and APO B-100, a high molecular-weight form which is characteristic of the endogenous system III. APO E is synthesized in many tissues and is greatly increased in injured nerves (APO E-4 is a risk factor for Alzheimer's disease) b. Chylomicrons I. From intestinal mucosa II. Almost only triglyceride (TG: 90%, C: 5%, PL: 3%) III. Apo C, Apo E, Apo B-100 IV. Becomes chylomicron remnants after lipoprotein lipase on surface of endothelial cells in capillaries remove much of the triglycerides (Absorbed by lymphatic ducts, can be >12 x the size of the second largest lipoproteins VLDL and chylomicron remnants (1000 nm vs 80 nm) (After the action of lipoprotein lipase, APO C is removed from both chylomicrons and VLDL, APO C-II activates lipoprotein lipase) c. Chylomicron remnants I. From chylomicrons after lipoprotein lipase has exerted its action II. APO E, APO B-48 III. Receptor-mediated endocytosis via chylomicron and LDL receptors and degradation in lysosomes (Ganong) |
|
|
Lipoproteins - Endogenous system
a. Very low density lipoproteins - Origin, fate, composition, Apoproteins b. Intermediate-density lipoproteins - Origin, fate, composition, Apoproteins c. Low-density lipoproteins - Origin, fate, composition, Apoproteins d. High-density lipoproteins - Origin, fate, composition |
a. Very low density lipoproteins
I. From liver and intestine II. Becomes IDL after the action of lipoprotein lipase III. Mainly triglycerides (TG: 55%, C: 20%, PL: 17%, P: 8%) IV. APO E, APO C, APO B-100 b. Intermediate-density lipoproteins I. From VLDL after lipoprotein lipase extracts triglycerides II. Becomes LDL after they receive cholesteryl esters from LDL by lecithin-cholseterol acyltransferase (LCAT) and lose more triglycerides and protein mainly in the liver sinusoids III. Mainly triglycerides (TG: 40%, C: 30%, PL: 20%, P: 10%) I. APO E, APO B-100 c. Low-density lipoproteins I. From IDL II. Taken up by receptor-mediated endocytosis by LDL receptor in hepatic and extrahepatic tissue (Some of the LDL enter the subendothelial space of arteries and are oxidized, then taken up by scavenger receptors on macrophages which become foam cells) III. Mostly cholesteryl esters (C: 53%, TG: 6%, PL: 21%, P: 20%) IV. APO B-100 e. High-density lipoproteins I. From liver and intestine II. HDL-receptor in liver and steroid-synthesizing endocrine glands III. Mainly protein (P: 50%, C: 20%, PL: 25%, TG: 5%) (Take up cholesterol that leaves extrahepatic cells via BC cassette proteins) (Ganong) |
|
|
Cholesterol
a. Fate of LDL b. Effect of Cholesterol intracellularly |
a. LDL
I. Binds to LDL receptors and are internalized by receptor-mediated endocytosis into endosomes with low pH II. Receptors are freed adn recycled to the membrane III. The cholesteryl esters enter lysosomes where free cohlesterol is released b. Cholesterol intracellularly -> 1. Inhibit HMG-CoA reductase 2. Processed partly to other cholesteryl esters by acetyl-CoA cholesterol acyltransferase (ACAT) 3. Inhibits the formation of LDL receptors (Ganong) |
|
|
Free fatty acid metabolism
a. The two lipases that regulate the supply of FFAs to tissues b. Regulation of hormone sensitive lipase |
a. Lipases
1. Lipoprotein lipase (I. Found on the surface of the endothelium of the capillaries II. Hydrolyzes the triglycerides in chylomicrons and VLDL, providing FFA and glycerol, which are reassembled into new triglycerides in the fat cells) 2. Hormone-sensitive lipase (I. In adipose tissue) b. Regulation of hormone-sensitive lipase + 1. Glucagon (Via Gs) 2. Catecholamines (Via beta-3 adrenergic receptors, Gs) 3. Growth hormone (Produce a protein that increase the ability of catecholamines to activate cAMP) 4. Glucocorticoids (Produce a protein that increase the action of cAMP) 5. Thyroid hormones - 1. Insulin 2. Prostaglandin E (Ganong) |
|
|
Eicosanoids
a. Origin of name b. Eicosanoids - Members and which enzyme they origin from c. Prostaglandins - Structure d. Prostaglandins - Organization |
a. The term eicosanoids reflect their origin from the 20-carbon (eicosa-) polyunsaturated fatty acid arachidonic acid
b. Eicosanoids 1. Coycloxygenases (COX1, COX2) I. Prostaglandins II. Prostacyclin (Cause vasodilation and inhibit platelet aggregation) III. Thromboxanes (TXA2 - synthesized by platelets, cause vasoconstriction and platelet aggregation) (COX1 is constitutive, COX2 is inducible, PGH2 is the precursor for the rest of the group) 2. Lipoxygenases I. Lipoxins (Via 15-lipoxygenase) II. Leukotrienes (Via 5-lipoxygenase) (Also 5-HETE, 12-HETE, 15-HETE) (3. CYP monoxygenases - 12-HETE, EETs, DHTs) c. Prostaglandins I. 20-carbon unsaturated fatty acids containing a cyclopentane ring d. Prostaglandins I. Divided into groups like PGE and PGF on the basis of the configuration of the cyclopentane ring II. The number of double bonds in the side chains is indicated by subscript numbers - ie PGE2, PGH2 (Ganong) |
|
|
Eicosanoids
a. Leukotrienes - Aminolipids - Members b. Leukotrienes - Aminolipids - Function |
a. Aminolipid leukotrienes
1. Leukotriene C4 (Contain glutathione) 2. Leukotriene D4 (Gly, Cys (Glutathione minus Glu)) 3. Leukotriene E4 (Cys) 4. Leukotriene F4 (Glu, Cys) b. Leukotrienes - Aminolipids - Function - Mediators of allergic responses and inflammation I. Bronchoconstriction II. Constrict arterioles III. Increase vascular permeability IV. Attract neutrophils and eosinophils (Ganong) |
|
|
Obesity
a. Body mass index (BMI) - Equation, values b. If human volunteers are fed a fixed high-calorie diet, some gain weight more rapidly than others. What is the slower weight gain most likely due to |
a. BMI
I. BMI = Body weight (kg) \ height^2 (m) II. > 25 is abnormal, 25-30 is overweight, >30 is obese (In USA > 55% is overweight and > 20% is obese) b. Increased energy expenditure in the form of small, fidgety movements (nonexercise activity thermogenesis, NEAT)) (Ganong) |
|
|
Trace elements believed essential for live
|
Trace elements believed essential for life
1. Chromium (↓-> Insulin resistance) 2. Cobalt (Part of vitamin B12, ↓ -> megaloblastic anemia) 3. Iron (↓ -> Microcytic anemia, ↑ -> Hemochromatosis) 4. Copper (↓ -> Anemia, changes in ossification. ↑ -> Wilson's disease) 5. Fluorine (↓ -> ↑Incidence of dental caries9 6. Arsenic 7. Iodine (-> Goiter) 8. Manganese 9. Nickel 10. Arsenic 11. Zinc (↓ -> Skin ulcers, depressed immune response, hypogonadal dwarfism) 12. Selenium (Ganong) |
|
|
Vitamin
a. Definition b. Which of the vitamins can be inadequately absorbed in the presence of obstructive jaundice or exocrine pancreas disorders |
a. Vitamin
I. Any organic dietary constituent necessary for life, health, and growth that does not function by supplying energy b. A, D, E, K (Ganong) |
|
|
Vitamin A
a. Synonym b. Action c. Deficiency symptoms d. Toxicity symptoms |
a. Vitamin A\Retinoids
b. Action 1. Constituents of visual pigments 2. Necessary for fetal development 3. Necessary for cell development throughout life c. Deficiency symptoms 1. Night blindness 2. Dry skin d. Hypervitaminosis A 1. Anorexia 2. Headache 3. Hepatosplenomegaly 4. Irritability 5. Scaly dermatitis 6. Hyperostosis and bone pain 7. Patchy loss of hair (First described by Arctic explorers who developed it after eating polar bear liver) (Ganong) |
|
|
Vitamin B1
a. Synonym b. Action c. Deficiency symptoms |
a. Thiamine
b. Action 1. Cofactor in decarboxylations 2. Cofactor in some dehydrogenases - pyruvate DH, branched-chain alpha-keto acid DH, 3. Cofactor in ketolase c. Deficiency symptoms 1. Beriberi I. Wet - High-output heart failure, edema II. Dry - Painful polyneuritis 2. Neuritis (Ganong) |
|
|
Vitamin B2
a. Synonym b. Action c. Deficiency symptoms |
a. Vitamin B2\Riboflavin
b. Action 1. Constituent of flavoproteins I. Flavin mononucleotide (FMN) II. Flavin dinucleotide (FAD) c. Deficiency symptoms 1. Glossitis 2. Cheilosis (Dry scaling and fissuring of the lips) (Ganong) |
|
|
Vitamin B3
a. Synonym b. Action c. Deficiency symptoms |
a. Vitamin B3\Niacin
b. Action 1. Constituent of NAD+ and NADP+ c. Deficiency symptoms - Pellegra I. 3Ds - Dermatitis, diarrhea, dementia (Can also be caused by tryptophan (niacin precursor) deficiency) (Ganong) |
|
|
Vitamin B6
a. Synonym b. Action c. Deficiency symptoms d. Toxicity symptoms |
a. Vitamin B6\Pyridoxine
b. Action 1. Forms prosthetic groups of certain decarboxylases and transaminases c. Deficiency symptoms 1. Convulsions 2. Hyperirritability d. Toxicity symptoms 1. Peripheral neuropathy (Require very high doses) (Ganong) |
|
|
Pantothetic acid
a. Action b. Deficiency symptoms |
a. Action
1. Constituent of CoA b. Deficiency symptoms 1. Dermatitis 2. Enteritis 3. Alopecia 4. Adrenal insufficiency (Ganong) |
|
|
Biotin
a. Action b. Deficiency symptom |
a. Action
1. Cofactor responsible for CO2 in several carboxylase enzymes (Acetyl-CoA carboxylase, propionyl-Coa carboxylase) b. Deficiency symptoms 1. Dermatitis 2. Enteritis (Ganong) |
|
|
Folates
a. Action b. Deficiency symptoms |
a. Action
1. Coenzymes for 1-carbon transfer - involved in methylating reactions b. Deficiency symptoms 1. Sprue (Primary intestinal malabsorption with steatorrhea) 2. Anemia 3. Neural tube defects in children born to folate-deficient women (Ganong) |
|
|
Vitamin B12
a. Synonym b. Structure c. Action d. Deficiency symptoms |
a. Cyanocobalamin
b. Complex of four substituted pyrrole rings around a cobalt atom c. Action 1. Coenyzme in amino acid metabolism 2. Stimulate erythropoiesis d. Deficiency symptoms 1. Pernicious anemia (Ganong) |
|
|
Vitamin E
a. Synonym b. Action c. Deficiency symptoms |
a. Tocopherols (alpha, beta, gamma)
b. Action 1. Antioxidant 2. Cofactors in electron transport in cytochrome chain (?) c. Deficiency symptoms 1. Ataxia and other S&S of spinocerebellar dysfunction (Ganong) |
|
|
Vitamin D
a. Source b. Action c. Deficiency symptoms d. Hypervitaminosis D |
a. Fish liver
b. Increase intestinal absorption of calcium and phosphate c. Rickets d. Hypervitaminosis D 1. Weight loss 2. Calcification of many soft tissues 3. Renal failure (Ganong) |
|
|
Vitamin K
a. Action b. Deficiency symptoms c. Hypervitaminosis K |
a. Action
1. Catalyze gamma-carboxylation of glutamic acid residues on various proteins concerned with blood clotting b. Deficiency symptoms 1. Hemorrhagic phenomena c. Hypervitaminosis K 1. GI disturbances 2. Anemia (Ganong) |
|
|
Thyroid gland
a. Histological structure b. Cell characteristics |
a. Made of multiple follicles\acini with a proteinaceous matter called colloid. Its surrounded by a single layer of cells.
(Active - Small follicles, cuboid or columnar cells, reabsorption lacunae on cells (sites of endocytosis of colloid). Inactive - Large colloid, flat cells) (Capillaries are fenestrated like in all endocrine glands) b. Cell characteristics 1. Flat in inactive state, cuboid or columnar in active state 2. Micrvolli projecting into the colloid 3. Prominent ER 4. Visible secretory droplets of thyroglobulin (Ganong) |
|
|
Thyroid gland
a. T4 vs T3 - Which is produced in highest quantities, which is most active b. What is the minimum daily iodine intake that will maintain normal thyroid function c. How is iodide transported into the thyroid colloid |
a. T4\Thyroxine is produced in highest quantities while T3 is most active. T4 is converted to T3 in peripheral tissues by 5' deiodinase (D1, D2, D3)
(T3 is more potent (3-5x) than T4 because it is less tightly bound to plasma proteins but binds more avidly to thyroid hormone receptors. RT3 is inert) b. 150 ug\day (The thyroid gland secretes 80 ug\day as iodine in T3 and T4. Most is excreted renally) c. Transport of iodide into the colloid 1. Via basolateral membrane - Na-I symporter (NIS) 2. Via apical membrane - Diffusion or iodide channel (Also taken up in various other tissues, such as the mammary gland, where diiodotyrosine is formed) (Ganong) |
|
|
Thyroid gland
a. How is iodide oxidized to iodine b. Incorporation of iodine and coupling c. Reverse T3 (RT3) d. Mechanism of release of T4\T3 from colloid to blood stream |
a. By thyroid peroxidase at the apical membrane of the thyroid cells
b. Incorporation of iodine and coupling I. By thyroid peroxidase I. First iodinated to 3-monoiodotyrosine (MIT), then 3-5-diiodotyrosine (DIT). Some are only iodinated to MIT II. Then thyroid peroxidase is involved in coupling of DIT and DIT\MIT -> T4 and T3 + Alanine c. Reverse T3 I. Inactive form with other pattern of iodination II. Produced iodination-coupling process in the thyroid gland and in peripheral deiodination of T4, mainly the last mechanism d. Mechanism of release of T4\T3 from colloid to blood stream 1. Colloid is endocytosed 2. Merge with lysosome 3. Proteases in the lysosome release T3, T4, T1, T2 (T1 and T2 is deiodinated by iodotyrosine deiodinase. Deficiency of this enzyme cause hypothyroidism, its the main source for iodine) 4. Exocytosis (Ganong) |
|
|
Transportation of thyroid hormones
a. Plasma proteins binding thyroid hormones b. Which has the largest capacity for transportation c. Which has the largest affinity d. Factors increasing binding proteins e. Factors decreasing binding proteins f. Agents inhibiting binding of thyroid hormones to their binding proteins - thus mimicking drugs lowering binding proteins |
a. Plasma proteins binding thyroid hormones
1. Transthyretin (Prealbumin-type) 2. Thyroxine-binding globulin (TBG) (Between alpha1 and alpha2) 3. Albumin b. Albumin c. Thyroxine-binding globulin (Most are bound to TBG. 99.98% of T4 and 99.8% of T3 is protein-bound) d. Factors increasing binding proteins 1. Estrogens 2. Methadone 3. Heroin 4. Major tranquilizers 5. Fibrates e. Factors decreasing binding 1. Glucocorticoids 2. Androgens 3. L-asparaginase (Chemotherapeutic agent) (The effects of decreasing or increasing the concentration of binding proteins cause a immediate effect on the free thyroid hormone, but this is compensated so the patient will stay euthyroid with the same free thyroid hormone levels) f. Agents inhibiting binding of thyroid hormones to their binding proteins 1. Salicylates 2. Phenytoin 3. 5-fluorouracil (Chemotherapeutic agent) (Ganong) |
|
|
Deiodination - T4 -> T3 conversion
a. Isotypes of deiodinases b. Which two tissues have an especially high T3\T4 ratio c. Which amino acid is present in all the deiodinases and necessary for their function d. T3\T4 ratio in fetuses e. Effect of burns, trauma, advanced cancer, cirrhosis, MI, renal failure, and fever on T3\T4 ratio f. Effect on T3 conversion during fasting |
a. D1-3
(They're presence in various tissues varies) b. Cerebral cortex and pituitary gland (D2 for cerebral cortex, D1 and D2 for pituitary) c. Selenocysteine (Deficiency cause fall in T3 levels and rise in RT3) d. Low, more RT3 is produced e. Depress it (Lower T3 -> Lower metabolism -> Save calories?) e. Decreased with simultaneous increase in RT3 (10-20% in 24 hours, 50% in 3-7 days, mechanism for preserving calories) (Ganong) |
|
|
Effects of thyroid hormones on
a. Heart b. Adipose tissue c. Muscle d. Bone e. Nervous system f. Gut g. Lipoprotein |
a. Heart
I. Chronotropic II. Inotropic (Increase number of beta-adrenergic receptors and G proteins, enhance response to catecholamines, increase proportion of alpha-myosin heavy chain (with higher ATPase activity, increased dromotropy in atria), decrease Na-Ca exchanger and increase Na-K-ATPase) b. Adipose tissue I. Catabolic (Stimulate lipolysis) c. Muscle I. Catabolic (Increase protein breakdown) (Hyper- -> thyrotoxic myopathy (extreme weakness), hypo- -> muscle weakness, stiffness, and cramps) d. Bone I. Developmental (Promote normal growth and skeletal development) (Euthyroidism is necessary for GH secretion, and thyroid hormones potentiate the effect of GH) e. Nervous system I. Developmental (Promote normal brain development - especially of cerebral cortex (->mental retardation), basal ganglia (motor rigidity), cochlea (->deaf-mutism)) II. Increased responsiveness\irritability (From increased responsiveness to catecholamines with consequent increased activation of the RAS?. Hyperhyroidism also cause hyperreflexia while hypothyroidism cause hyporeflexia) f. Gut I. Increase rate of carbohydrate absorption (Hyper- -> plasma glucose levels rise rapidly after a meal and can exceed the renal reabsorption threshold) g. Lipoprotein I. Lower circulating cholesterol levels from increased formation of hepatic LDL receptors, causing increased LDL clearance (Calorigenic (heat generating) effect - Stimulate oxygen consumption by metabolically active tissues and increase metabolic rate (exceptions - brain, anterior pituitary, uterus)(some of the increased metabolism is from the increased FFAs from increased lipolysis) (Also increase the dissociation of oxygen from hemoglobin by increasing 2,3DPG and increase Na-K-ATPase in many tissues) (Ganong) |
|
|
TSH
a. Structure b. Pattern of secretion c. Effects of TSH on the thyroid d. TSH receptor |
a. Structure
I. Glycoprotein (211 residues with hexoses, hexosamines, and sialic acid) II. Alpha and beta subunit (Alpha subunit is shared with FSH, LH, and hCG-alpha. -> ↑↑hCG as in placental tumors can activate TSH receptors and cause mild hyperthyroidism) b. Pattern of secretion I. Pulsatile II. Peak around midnight, declines during the day c. Effects of TSH on the thyroid I. Affect all phases of synthesis and release and cause hypertrophy of the follicular cells (↑Iodide binding, synthesis of T3 and T3, iodotyrosines, secretion of TG into the colloid, endocytosis of the colloid, iodide trapping) (Overstimulation cause goiter) d. Gs receptor (Also activate PLC) (Ganong) |
|
|
Thyroid hormones - Control mechanisms
a. Effect of temperature on TRH b. Effect of stress of TRH c. Agents inhibiting TSH |
a. Effect of temperature on TRH
I. Low temperature -> ↑TRH and vice versa - Thyroid hormone thermogenesis (Negligible in adults, more prominent in infants and certain animals) b. Inhibitory effect c. Agents inhibiting TSH 1. Dopamine 2. Somatostatin 3. Glucocorticoids (Ganong) |
|
|
Hypothyroidism
a. Synonym for hypothyroidism in adults b. General causes c. S&S |
a. Myxedema
(Also used specifically for the skin changes that occur in the syndrome) b. General causes 1. At thyroid gland 2. At pituitary gland 3. At hypothalamus c. S&S 1. ↓BMR (40% in athyreotic individuals) 2. Coarse and sparse hair 3. Dry and yellowish skin (carotenemia) (Carotenemia from decreased hepatic conversion of carotene to vitamin A and the following accumulation of carotene in the bloodstream, not yellow on sclera as in jaundice) 4. Low cold tolerance 5. Husky and slow voice 6. Slow mentation - Memory (Some people experience myxedema madness - psychiatric involvement) 7. ↑Plasma cholesterol (Ganong) |
|
|
Hypothyroidism in children
a. Synonym for the condition where children are hypothyroid from birth or before b. Causes c. S&S |
a. Cretinism
b. Causes 1. Maternal iodine deficiency 2. Fetal thyroid dysgenesis 3. Fetal hypopituitary hypothyroidism 4. Maternal antithyroid antibodies that cross the placenta 5. Inborn errors of thyroid hormone synthesis (Despite of deficiencies in utero, maternal T4 can cross the placenta and maintain euthyroidism until birth) (One of the most common causes of preventable mental retardation) c. S&S 1. Stunned growth 2. Mental retardation (Cerebral hemispheres) 3. Motor rigidity (Basal ganglia) 4. Deaf-mutism (Cochlea) 5. Potbellies 6. Enlarged, protruding tongues (Ganong) |
|
|
Hyperthyroidism
a. S&S b. Causes |
a. S&S
1. Nervousness and ↑irritability 2. Weight loss and hyperphagia 3. Heat intolerance 4. ↑Pulse pressure 5. Fine tremor (Especially of outstretched fingers) 6. ↑BMR b. Causes Thyroid overactivity 1. Grave's disease (60-80% of cases, antibodies to the TSH receptor, 50% of patients have exophthalmus, fibroblasts with TSH receptors transform to adipocytes and release cytokines that promote inflammation and edema in the presence of TSH, other antibodies are present as well (TG, thyroid peroxidase) 2. Hashimoto's thyroiditis (Autoimmune, can cause thyrotoxicosis initially, hypothyroidism later) 3. Solitary toxic adenoma 4. Toxic multinodular goiter 5. TSH-secreting pituitary tumor 6. Mutations causing constitutive activation of TSH receptor Extrathyroidal 1. Administration of T3 or T4 2. Ectopic thyroid tissue (Ganong) |
|
|
Antithyroid drugs
a. Substances competing with iodide for transport into the thyroid via the Na-I symporter b. Drugs inhibiting the iodination of monoiodotyrosine and block the coupling reaction c. Effect of iodide on thyroid function, what is this effect called d. Effect of vegetables of the Brasicacea family (cabbage, turnips) on thyroid gland function |
a. Chlorate, pertechnate, nitrate
b. Thiourylenes - Propylthiouracil, Methimazole (Compete with tyrosine residues for iodine and become iodinated, also propylthiouracil inhibits D2 deiodinase, both drugs may also ameliorate hyperthyroidism by suppressing the immune system and thus depressing the formation of stimulatory antibodies) c. Wolff-Chaikoff effect I. Large doses of iodides produce a mild and transient inhibition of organic binding of iodide (Greater when iodide transport is increased as in hyperthyroidism, also act by reducing the effect of TSH on the thyroid gland by reducing cAMP and inhibits proteolysis of thyroglobulin) d. Inhibit and is thus goitrogenic (Goitrogenic from increased TSH due to decreased circulating thyroid hormones. Contains progoitrin and a substance that converts this to goitrin, the active substance. The converter is heat-labile, but there also converters in the intestine) (Ganong) |
|
|
Islet cells
a. Volume % of pancreas, most numerous where b. Number of islets c. Cell types and their secretory product |
a. 2%, tail
(80% exocrine, rest is made up of ducts and blood vessels) b. 1-2 million c. Cell types 1. A\Alpha cells - Glucagon (Up to 20% of the cells) 2. B\Beta cells - Insulin (Up to 75% of the cells) 3. D\Delta cells - Somatostatin 4. F cells - Pancreatic polypeptide (The A-cell-rich islets arise embryologically from the dorsal pancreatic bud (tail, body, anterior and superior part of head), and the F-cell-rich islets arise from the ventral pancreatic bud (posterior part of head of pancreas)) (Ganong) |
|
|
Insulin
a. Size and structure b. Insulin activity that is not suppressed by antiinsulin antibodies has been called nonsuppressible insulin-like activity (NSILA) - Which agents are responsible for this c. Half-life of insulin d. Degradation |
a. Size and structure
I. 51 amino acids, 5.8 kD II. Preproinsulin, -pre cleaved after entering ER, pro- cleaved in vesicles to release connecting (C) peptide (C peptide level provide an index of B cell function in patients receiving exogenous insulin) b. NSILA I. IGF-I and IGF-II (Bound (high-molecular weight) and free (low-molecular weight)) c. Half-life - 5 minutes d. Degradation I. Destroyed by proteases in the endosomes after being endocytosed (Ganong) (Ganong) |
|
|
Effects of insulin
a. Rapid effects (seconds) b. Intermediate effects (minutes) c. Delayed effects (hours) |
a. Rapid effects (seconds)
1. Increased transport of glucose, amino acids, and K into insulin-sensitive cells b. Intermediate effects (minutes) 1. Stimulation of protein synthesis 2. Inhibition of protein degradation 3. Activation of glycolytic enzymes and glycogen synthase 4. Inhibition of phosphorylase and gluconeogeneic enzymes c. Delayed effects (hours) 1. Increase in mRNA for lipogenic and other enzymes (Ganong) |
|
|
Insulin - Effects on various tissues
a. Adipose tissue b. Muscle tissue c. Liver d. General |
a. Adipose tissue
1. Increased glucose entry (↑GLUT-4) 2. Increased fatty acid synthesis 3. Increased glycerol phosphate synthesis 4. Increased triglyceride deposition 5. Activation of lipoprotein lipase (Facilitate release of lipids from lipoproteins which subsequently can get stored in adipocytes) 6. Inhibition of hormone-sensitive lipase 7. Increased K uptake b. Muscle tissue 1. Increased glucose entry (↑GLUT-4) 2. Increased glycogen synthesis 3. Increased amino acid uptake 4. Increased protein synthesis in ribosomes 5. Decreased protein catabolism 6. Decreased release of gluconeogenic amino acids 7. Increased ketone uptake 8. Increased K uptake c. Liver 1. Decreased ketogenesis 2. Increased protein synthesis 3. Increased lipid synthesis 4. Increased glucose entry from activation of glucokinase 5. Decreased glucose output due to decreased gluconeogenesis, increased glycogen synthesis, and increased glycolysis d. General - Increased cell growth (Ganong) |
|
|
Glucose transporters
a. Transporters in the renal tubules and intestine - Type of transport, which b. Transporters in the rest of the body - Type, which c. Which is the transporter in muscle and adipose tissue that is stimulated by insulin d. How does insulin lower blood sugar |
a. Renal and GI transport
I. Secondary active transport with Na II. Sodium-dependent glucose transporters (SGLT) 1 and 2 (1 in both places, 2 in renal tubules only) b. Glucose transporters except renal and intestinal I. Facilitated diffusion II. Glucose transporters (GLUT) 1-7 c. GLUT-4 (A pool of GLUT-4 molecules is maintained in vesicles in the cytoplasm of insulin-sensitive cells, associated with phosphoinositol-3 kinase) d. Because insulin-sensitive tissues also contain a population of GLUT-4 vesicles that move into the cell membrane in response to exercise and are independent of the action of insulin (5'-AMP kinase?) (Ganong) |
|
|
Glucose transporters (GLUT) - Function, Km, Major sites of expression
a. GLUT 1 and 3 b. GLUT 2 c. GLUT 4 d. GLUT 5 |
a. GLUT 1 and 3
I. For basal glucose uptake II. Km 1-2 mM for GLUT 1, < 1 mM for GLUT 3 III. Placenta, brain, red cells (only GLUT 1), kidneys.. (Organs that critically depend upon glucose) b. GLUT 2 I. Function 1. Beta-cell glucose sensor 2. Transport out of intestinal and renal epithelial cells II. Km 12-20 mM III. Beta cells of islets, liver, epithelial cells of small intestine, kidneys c. GLUT 4 I. Insulin-stimulated glucose uptake II. Km 5 mM III. Skeletal and cardiac muscle, adipose tissue... d. GLUT 5 I. Fructose transport II. Km 1-2 mM III. Jejunum, sperm (The function of GLUT 6 and 7 is not known) (The Km is the glucose concentration at which transport is half-maximal) (Ganong) |
|
|
Insulin receptors
a. Structure b. Intracellular effects of activation of insulin receptors |
a. Structure
I. 340 kD II. Tetramer of two alpha and two beta glycoprotein subunits 1. The alpha subunits bind insulin and are extracellular 2. The beta subunits span the membrane and the intracellular portion have tyrosine kinase activity (Autophosphorylation is a necessary step for it to exert its effect) b. Intracellular effects of activation of insulin receptors 1. Trigger phosphorylation of some proteins and dephosphorylation of others, mostly on serine and threonine residues 2. Insulin receptor substrate 1 (IRS-1) some some of the effects 3. The growth-promoting anabolic effects are mediated via phosphoinositol 3-kinase (PI3K) (Its very similar to the receptor for IGF-1 and IGF-1 and insulin have some cross-binding to the other receptor) (Ganong) |
|
|
Diabetes mellitus
a. S&S b. The two fundamental biochemical defects to which most of the abnormalities can be traced c. Mechanisms causing hyperglycemia |
a. S&S
1. Polydipsia (From polyuria) 2. Polyuria (Excessive loss of water from hyperosmolar urine) 3. Polyphagia (Deficient glucose utilization in the cells of the satiety area of the hypothalamus) 4. Weight loss 5. Hyperglycemia 6. Glycosuria 7. Ketosis (Excess acetyl-CoA -> acetoacetyl-CoA --liver--> acetoacetate and other ketone bodies) 8. Acidosis (Acetoacetic acnd and beta-hydroxybutyric acid, -> Kussmaul breathing) 9. Coma (Acidosis, dehydration, hyperosmolar coma (coma due to hyperosmolarity independently), lactic acidosis, brain edema (1% of children with ketoacidosis, 25% mortality rate)) b. 1. Reduced entry of glucose into various "peripheral" tissues 2. Increased liberation of glucose into the circulation from the liver "Starvation in the midst of plenty" (The entry of amino acids into muscle is also decreased and lipolysis is increased) c. Mechanisms causing hyperglycemia 1. Failure of GLUT-4 expressing tissues to take up glucose (Skeletal, cardiac, and smooth muscle, adipose tissue) 2. Glycogenolysis and gluconeogenesis of the liver (Insulin normally stimulate glycogen synthesis and inhibit gluconeogenesis) 3. Glucagon (Hyperglucagonemia is generally present in diabetes) 4. Catecholamines, cortisol and GH (When the stress of illness is severe) (Ganong) |
|
|
Oral glucose tolerance test
a. Procedure b. Values indicating diabetes mellitus c. Values indicating impaired glucose tolerance |
a. Oral glucose tolerance test
I. Adults are given 75 g of glucose in 300 mL of water II. In normal individuals, 1. The fasting venous plasma glucose is less than 6.3 mM\115 mg\dl 2. The 2-hour value is less than 7.8 mM\140 mg\dL 3. No value is greater than 11.1 mM\200 mg\dL b. Values indicating diabetes mellitus I. The 2-hour value and one other value are greater than 11.1 mM\200 mg\dL c. Impaired glucose tolerance I. Diagnosed if any of the values are above the upper limits of normal but below the values diagnostic of diabetes (Ganong) |
|
|
Diabetes
a. Changes in protein metabolism b. Changes in fat metabolism c. Effect of acidosis on Na and K levels |
a. Changes in protein metabolism
1. The rate at which amino acids are catabolized to CO2 and H2O is increased 2. More amino acids are converted to glucose in the liver I. Hyperglucagonemia II. Glucocorticoids III. Increased supply of amino acids due to the absence of the stimulus for protein synthesis from insulin IV. The gluconeogenic enzymes activity are increased (phosphoenolpyruvate carboxykinase, fructose 1,6-DPase, glucose 6-phosphatase) V. ↑Acetyl-CoA -> ↑Pyruvate carboxylase (->↑oxaloacetate) (Insulin deficiency increase acetyl-CoA because lipogenesis is decreased) (Protein depletion\wasting from any cause is associated with poor resistance to infections) b. Changes in fat metabolism 1. ↑Lipid catabolism I. Insulin inhibits hormone-sensitive lipase, in the absence the plasma levels of FFAs is increased II. Hyperglucagonemia 2. ↑Ketogenesis (The acetyl-CoA supply exceeds the capacity of the liver to catabolize it and ketone bodies are formed) 3. ↓Synthesis of fatty acids and triglycerides I. Lipoprotein lipase is not stimulated by insulin to release lipid products to adipocytes II. Triglyceride synthesis and FA synthesis is not stimulated by insulin (↓acetyl-CoA carboxylase - acetyl-CoA -> malonyl-CoA) 4. ↑Plasma cholesterol I. ↑Hepatic VLDL production II. ↓Removal of VLDL and LDL from the circulation c. Effect of acidosis on Na and K levels I. Na is lowered because it follows the organic anions from the ketoacids in the urine II. Total K is low, but plasma K is usually normal (1. ECF volume is decreaed, 2. K move from cells to ECF when ECF H concentration is high, 3. Lack of insulin-induced entry of K into cells) (Ganong) |
|
|
Insulin excess - Effects at various plasma glucose levels
a. 4.6 mM b. 3.8 mM c. 3.2 mM d. 2.8 mM e. 2.2 mM f. 1.7 mM g. 1.1 mM h. 0.6 mM |
a. 4.6 mM
I. Inhibition of insulin secretion b. 3.8 mM I. Secretion of glucagon, GH, and epinephrine II. Accompanied by autonomic sympathetic symptoms such as palpitations, sweating, and nervousness III. Hunger c. 3.2 mM I. Cortisol secretion d. 2.8 mM - Neuroglycopenic symptoms 1. Confusion 2. Slurred speech 3. Coordination problems (Can mimic drunkenness) e. 2.2 mM - Lethargy f. 1.7 mM - Coma g. 1.1 mM - Convulsions h. 0.6 mM - Permanent brain damage, death (Ganong) |
|
|
Insulin
a. Peripheral venous level in fasting humans b. Amount secreted in basal state per hour, increase following ingestion of food c. Factors stimulating insulin secretion d. Factors inhibiting insulin secretion |
a. 0-500 pM
b. 1 U\h, 5-10x increase (40 U\287 nmol is secreted per day) c. Factors stimulating insulin secretion 1. Glucose, mannose 2. Amino acids (Insulin stimulates protein synthesis - free amino acids can be used for protein synthesis, via metabolism -> ↑ATP) 3. Intestinal hormones I. Gastric inhibitory peptide (GIP) III. Glucagon-like peptide 1 (GLP-1) (GLP is produced by preproglucagon, GIP and GLP-1 have receptors on beta cells, explain why oral glucose and amino acids cause higher insulin release, CCK (oral amino acids), secretin, and gastrin is also involved) 4. Beta-keto acids (Insulin combats the fat catabolism that produce beta-keto acids such as acetoacetate, via metabolism -> ↑ATP) 5. Acetylcholine (M4 receptors, activates PLC -> ↑IP3 -> ↑Ca) 6. Glucagon 7. Beta-adrenergic stimulators 8. Sulfonylureas (Tolbutamide, acetohexamide, tolazemide, glipizide, glyburide, directly inhibit ATP-sensitive K-channels) 9. Theophylline (tea) (Phosphodiesterase inhibitor -> ↑cAMP) 10. NO (L-arginine is the precursor) (Substances that increase cAMP in general - theophylline, glucagon, epinephrine) d. Factors inhibiting insulin secretion 1. Somatostatin 2. Alpha-adrenergic stimulators 3. Beta-adrenergic blockers 4. Thiazide diuretics (Via K depletion) 5. Hypokalemia (Pancreatic cell damage? Less intracellular K to cause depolarization of beta cells?) 6. Insulin (+Galanin, diazoxide, phenytoin, alloxan, microtubule inhibitors) (The net effect of catecholamines is usually inhibition (alpha-2 adrenergic) (Ganong) |
|
|
Effects of the plasma glucose level
a. Effect of plasma glucose on insulin secretion by beta cells |
a. Effects of plasma glucose on insulin secretion by beta cells - Biphasic
1. Short-lived immediate increase in secretion I. Glucose enters beta cells via GLUT-2 transporters -> (12-20 Km) II. Phosphorylated by glucokinase -> III. Glycolysis -> citric acid cycle -> oxidative phosphorylation -> IV. ↑ATP -> inhibit ATP-sensitive K-channels -> reduce K efflux -> V. Depolarization -> VI. Stimulate voltage-sensitive Ca channels VII. Ca cause exocytosis of insulin-containing secretory granules, causing the initial spike of insulin secretion 2. More slowly developing prolonged release of insulin I. Metabolism of pyruvate via the citric acid cycle -> II. ↑Glutamate -> III. Act on a second pool of secretory granules, committing them to the releasable form (decrease pH?) (Ganong) |
|
|
Oral hypoglycemic agents
a. Sulfonylureas - Mechanism, members b. Metformin - Mechanism c. Thiazolidinediones - Mechanism, members |
a. Sulfonylureas
I. Inhibit ATP-sensitive K-channels in beta cells II. Tolbutamide, tolazamide, acetohexamide, glipizide, glyburide b. Metformin I. Reduce gluconeogenesis and thus decrease hepatic glucose output (However, associated with lactic acidosis. The other biguanide phenformin was withdrawn due to the incidence of lactic acidosis) c. Thiazolidinediones I. Agonist for peroxisome proliferator-activated receptor gamma (PPAR-gamma) -> increase insulin-mediated peripheral glucose utilization (PPAR-gamma is part of the hormone-sensitive nuclear transcription factors, its activated during satiety states) II. Troglitazone (Ganong) |
|
|
Metabolic syndrome\Syndrome X
a. What b. It is assumed that fat produce a chemical signal or signals that act on muscles and the liver to increase insulin resistance - What substance could that be |
a. Metabolic syndrome\Syndrome X
I. A name for a group of risk factors that occur together and increase the risk for coronary artery disease, stroke, and type 2 diabetes II. S&S 1. Abdominal\central obesity 2. Hypertension 3. Dyslipidemia - High triglyceride levels, Low HDL levels 4. Increased fasting glucose (Prediabetic or type 2 diabetes) b. 1. FFAs 2. Signaling molecules - Adipokines I. Leptin ando adiponectin decrease insulin resistance II. TNFalpha and resistin increase insulin resistance (Congenital lipodystrophy (fat depots fail to develop) is accompanied by marked insulin resistance as well) Ganong) |
|
|
Glucagon
a. Structure b. Where is the preproglucagon produced c. Actions |
a. Glucagon
I. Polypeptide II. 29 amino acids, 3.5 kD b. Preproglucagon I. Alpha cells of pancreas (-> Glucagon, major proglucagon fragment (MPGF) II. L cells in the lower gastrointestinal tract (-> GLP-1, GLP-2, Glicentin. GLP-1 is further processed and then function as a potent stimulator of insulin secretion and also increase glucose utilization)) III. Brain (-> GLP-1, GLP-2, uncertain function, nucleus solitarius -> hypothalamus, GLP-2 inhibit food intake) c. Actions (Via G proteins\serpentine receptors) 1. Glycogenolytic in liver (Gs -> ↑cAMP -> ↑PKA -> ↑phosphorylase, part of effect also via other Gq receptor -> PLC -> IP3 -> Ca) 2. Gluconeogenic (PKA inhibit glycolysis via inhibiting the conversion of phosphoenolpyruvate to pyruvate and decrease concentration of fructose 1,6-BP) 3. Lipolytic 4. Ketogenic (↓malonyl-CoA levels in the liver) 5. Calorigenic effect (From hepatic deamination of amino acids) 6. Stimulate the secretion of GH, insulin, and pancreatic somatostatin (Ganong) |
|
|
Factors affecting glucagon secretion
a. Stimulators b. Inhibitors |
a. Stimulators
1. Amino acids (Particularly the glucogenic amino acids (Ala, Ser, Gly, Cys, Thr), protective method against hypoglycemia from simultaneous stimuli of insulin secretion?) 2. CCK, gastrin (Explain why oral amino acids cause a more powerful release of glucagon than intravenous, both CCK and gastrin are released in response to high-protein meals) 3. Cortisol 4. Exercise 5. Infections and other stresses (At least partly via sympathetic response) 6. Beta-adrenergic stimulators (Predominates over the inhibitory effect of alpha receptors. Opposite as with insulin) 7. Theophylline 8. Acetylcholine b. Inhibitors 1. Glucose 2. Somatostatin 3. Secretin 4. FFA 5. Ketones (4 and 5 can be overridden since glucagon is increased during ketoacidosis) 6. Insulin 7. Alpha-adrenergic stimulators 8. GABA (The beta cells contain GABA which is assumed to be secreted with insulin in response to hyperglycemia, GABA acts on GABAa receptors (Cl channels) to hyperpolarize the cell) 9. Phenytoin |
|
|
Somatostatin
a. Which of the pancreatic cells produce it b. Structure c. Gastrointestinal\Metabolic effect d. Somatostatinoma - S&S e. Stimuli for release |
a. Delta cells
b. Polypeptide 14 and 28 amino acid variant, SS28 is more active than SS14 in inhibiting insulin secretion) c. Gastrointestinal\metabolic effect 1. Inhibit the secretion of the other pancreatic hormones - Insulin, glucagon, and pancreatic polypeptide 2. d. Somatostatinoma - S&S 1. Hyperglycemia and other diabetes manifestations 2. Dyspepsia (Due to slow gastric emptying and decreased gastric acid secretion, due to inhibition of CCK) 3. Gallstones (Due to inhibition of CCK) e. Stimuli for release - Many of the same as for insulin 1. Glucose 2. Amino acids (Arginine and leucine in particular) 3. CCK (Ganong) |
|
|
Pancreatic polypeptide
a. Source b. Function c. Stimuli for release d. Inhibitors of release |
a. F cells of pancreatic islets
b. function 1. Slows the absorption of food (Might smooth out the peaks and valleys of absorption, but its exact physiological function is still uncertain) c. Stimulators 1. Acetylcholine 2. Protein-containing meal 3. Fasting and hypoglycemia 4. Exercise d. Inhibitors 1. Somatostatin 2. Glucose (Ganong) |
|
|
Pancreatic islets
a. Internal regulation b. Morphology c. The two types of pancreatic islets |
a. Internal regulation
I. Somatostatin inhibit insulin, glucagon, and pancreatic polypeptide II. Insulin inhibit glucagon III. Glucagon stimulate insulin and somatostatin b. Morphology I. A and D cells peripherally II. B cells centrally c. Pancreatic islets 1. Glucagon-rich\A-rich 2. Pancreatic polypeptide-rich\F-rich (Gap junctions have been demonstrated between A, B, and D cells) (Ganong) |
|
|
Carbohydrate metabolism
a. Explain the rise in hepatic glycogen content following the initiate decrease after catecholamine stimulation b. Effect of thyroid hormones c. Effect of adrenal glucocorticoids d. effect of growth hormone |
a. Catecholamines convert large amount of pyruvate to lactate in muscle cells -> the lactate is released and oxidized in the liver to pyruvate -> pyruvate is converted to glycogen
b. Effect of thyroid hormones - Hyperglycemic 1. Increase absorption of glucose from the intestine 2. Increase the sensitivity of catecholamines -> deplete hepatic glycogen (Glycogen-depleted liver cells are easily damaged, and when the liver is damaged, the glucose tolerance curve is diabetic cause the liver takes up less of the absorbed glucose) 3. Accelerate degradation of insulin c. Adrenal glucocorticoids - hyperglycemic (80% of patients with Cushing's have reduced glucose tolerance and 20% have diabetes, they are gluconeogenic themselves, but their role is mainly permissive to glucagon) (Patients with adrenal insufficiency reach hypoglycemia easier and the plasma-glucose lowering effect of insulin is improved) d. Growth hormone - Hyperglycemic I. Mobilizes FFA from adipose tissue II. Decrease glucose uptake into some tissues (anti-insulin) III. Increase hepatic glucose output IV. May decrease binding of isnulin (Both direct and via IGF-1, 25% of patients with GH-tumors have diabetes and hypophysectomy is more effecting in ameliorating diabetes than adrenalectomy) (Ganong) |
|
|
Hypoglycemia
a. Causes b. Hypoglycemia unawareness - What, caused by |
a. Hypoglycemia
1. Type 1 diabetics 2. Insulinoma 3. Malignant tumors secreting IGF-II 4. Liver disease (The glucose tolerance curve is diabetic but the fasting glucose level is low) 5. Infants with GLUT 1 deficiency - Cerebral hypoglycemia (GLUT 1 is responsible for transport across BBB, seizures and developmental delays are characteristic) b. Hypoglycemia unawareness I. Absence of the autonomic warning signals with decreasing glucose concentration II. Prone to develop in patients with insulinoma and in diabetics with intensive insulin therapy (Appears that repeated bouts of hypoglycemia cause the eventual development of hypoglycemia unawareness) (Ganong) |
|
|
Diabetes mellitus
a. Proportion of type 1 and 2 b. Pathophysiology of diabetes c. Explain the increased susceptibility to chronic ulceration and gangrene |
a. 90% is type 2
b. Pathophysiology 1. Microvascular abnormalities I. Diabetic retinopathy (Microaneurysms, exudates, and hemorrhages. Can lead to blindness) II. Diabetic nephropathy 2. Macrovascular abnormalities I. ↑Plasma LDL -> ↑Atherosclerosis -> ↑MI, stroke 3. Neuropathies I. Autonomic nervous system II. Peripheral nerves c. 3 factors 1. Atherosclerotic circulatory insufficiency 2. Autonomic neuropathy 3. Reduced resistance to infection (Intracellular glucose -> Amadori products -> advanced glycosylation end products (AGEs) -> cross-link matrix proteins -> damage blood vessels, inhibit leukocyte response to infection) (Ganong) |
|
|
Adrenal medulla
a. % of adrenal glands b. Types of cells and their characteristics c. Paraganglia |
a. 28%
b. Types of cells 1. Epinephrine-secreting cells I. 90% II. Large, less dense granules 2. Norepinephrine-secreting cells I. 10% II. Small, dense granules that fail to fill the vesicles c. Paraganglia I. Small groups of cells resembling those in the adrenal medulla II. Found near the thoracic and abdominal sympathetic ganglia (Ganong) |
|
|
Adrenal cortex
a. Layers - Characteristics, products b. Fetal adrenal cortex c. Cellular characteristics of steroid-secreting cells |
a. Layers
1. Zona glomerulosa I. Whorl\spiral arrangement of cells II. Aldosterone (15% of adrenal gland, regenerate adrenal cortex) 2. Zona fasciculata I. Columns of cells separated by venous sinuses II. Glucocorticoids (50% of adrenal glands) 3. Zona reticularis I. Cell columns become interlaced into network II. Sex hormones (7%) b. Fetal adrenal cortex I. Makes up 80% of the adrenal gland during fetal life and undergoes rapid degeneration at the time of birth II. Produce and secrete sulfate conjugates of androgens that are converted to estrogens in the placenta c. Cellular characteristics of steroid-secreting cells 1. Prominent smooth endoplasmic reticulum 2. Pleomorphic (polymorphic) mitochondria 3. Lipid droplets (Ganong) |
|
|
Adrenal medulla
a. Steps in synthesis of epinephrine b. Most of the dopamine (95%), norepinephrine (70%) and epinephrine (70%) circulates in an conjugated inactive form. What substance is it conjugated to c. Relative concentration of dopamine, norepinephrine, and epinephrine d. Half-life e. Other substances secreted by the adrenal medulla |
a. Epinephrine synthesis
1. Tyrosine hydroxylase I. Tyrosine -> Dopa II. Tetrahydrobiopterin (Dihydroxyphenylalanine\dopa) 2. Dopa decarboxylase I. Dopa -> Dopamine II. Pyridoxal phosphate 3. Dopamine beta-hydroxylase I. Dopamine -> Norepinephrine II. Ascorbate 4. Phenylethanolamine-N-methyltransferase (PNMT) I. Norepinephrine -> Epinephrine II. S-adenosylmethionine (Found in appreciable quantities only in the brain and the adrenal medulla, induced by glucocorticoids in high doses, as in adrenal medulla with the veins draining the adrenal cortex) b. Sulfate c. 1. NE (300 pg\mL) 2. Dopamine (35 pg\mL) 3. Epinephrine (30 pg\mL) (Epinephrine need concentration > 50 pg\mL to produce cardiac and metabolic effects, while norepinephrine must be > 1500 pg\mL. Only epinephrine normally exceed this threshold) d. Around 2 minutes e. Other substances secreted by the adrenal medulla 1. Chromgranin A 2. ATP 3. Met-enkephalin (only in epinephrine-granules, responsible for most of the circulating enkephalins, don't cross BBB) (Ganong) (Ganong) |
|
|
Norepinephrine and epinephrine
a. Effect on vasoconstriction b. Effect on blood pressure c. Effect on cardiac output d. Effect on thermogenesis e. Effect on insulin secretion |
a. Vasoconstriction
I. Norepinephrine primarily vasoconstricts via alpha-1 II. Epinephrine primarily vasodilates skeletal and liver vasculature via beta-2 and overrides the effect of alpha-1 b. Blood pressure I. Norepinephrine - Increased systolic and diastolic blood pressure II. Epinephrine - Increased pulse pressure\Increased systolic and decreased diastolic c. Cardiac output I. NE: Decreased via reflex bradycardia that overrides the cardioacceleratory effect of NE II. E: Increased, exceed strength of reflex bradycardia from baroreceptor reflex d. Thermogenesis - Increased I. First from cutaneous vasoconstriction, which decrease heat loss and leads to a rise in body temperature II. Second via oxidation of lactate in the liver (Lactate levels are increased by catecholamines) e. Insulin secretion I. Increase secretion of insulin and glucagon via beta-adrenergic receptors II. Inhibit secretion of insulin and glucagon via alpha-adrenergic mechanisms (Ganong) |
|
|
Dopamine
a. Physiologic function b. Effects of injected dopamine c. When is it useful |
a. Uncertain
(Made in the renal cortex, cause natriuresis possibly by inhibiting Na-K-ATPase) b. Effects of injected dopamine 1. Renal and mesenteric vasodilation (Via specific dopamineric receptor) 2. Vasoconstriction elsewhere (Via conversion to NE probably) 3. +Inotropic effect (Beta-1 adrenergic) (Net effect is an increase in systolic pressure and no change in diastolic pressure) c. In the treatment of traumatic and cardiogenic shock. |
|
|
Adrenocortical hormones
a. Cholesterol - Number of carbons b. Pregnane derivatives - Number of carbons, members c. Androstane derivatives - Number of carbones, members d. Estrane derivatives - Number of carbons, members |
a. Cholesterol - C27
b. Pregnane derivatives I. C21 II. Progesterone, Corticoids (Two-carbon side chain at position 17) c. Androstane derivatives I. C19 II. Androgens (Keto (->17-ketosteroids) or hydroxyl group at position 17) d. Estrane derivatives I. C18 II. Estrogens (17-keto or hydroxyl group, no methyl group at position 10) (The groups that lie above the plane of the steroid rings are indicated by beta and solid line while those that lie below are indicated by alpha and dashed line. Except 17-hydroxygroups which is in alpha, all the others are beta - 3, 11, 21) (Ganong) |
|
|
Adrenocortical steroids
a. Steroids secreted by zona glomerulosa b. Steroids secreted by zona fasciculata c. Steroids secreted by zona reticularis |
a. Zona glomerulosa
I. Aldosterone II. 11-deoxycorticosterone (Zona glomerulosa lack 17-alpha-hydroxylase activity (for producing glucocorticoids and androgens (-> estrogens) and 11-beta hydroxylase (for next step in glucocortid synthesis). Its the only part that has aldosterone synthase which can convert corticosterone to aldosterone) (Aldosterone - 0.15 mg\day, deoxycorticosterone - 0.20 mg\day) b. Zona fasciculata I. Cortisol (10 mg\day) II. Corticosterone (3 mg\day) (Zona fasciculata has more 3-beta-hydroxysteroid DH than zona reticularis) c. Zona reticularis I. Dehydroepiandrosterone (DHEA) (20 mg\day, only the steroid where the majority is conjugated to sulfate) II. Androstenedione (Zona reticularis has more 17,20-lyase activity than zona fasciculata) (Both are 17-ketosteroids, DHEA from 17-hydroxypregnenolone, androstenedione from 17-hydroxyprogesterone, DHEA is the only steroid that is primarily in the sulfated form, sulfated by adrenal sulfokinase) (Ganong) |
|
|
Potencies of mineralocorticoids and glucocorticoids
a. Which substance is used as a reference (1.0) for glucocorticoid and mineralocorticoid activity b. Aldosterone c. Corticosterone d. Prednisolone e. Dexamethasone f. Cortisone |
a. Cortisol
b. Aldosterone I. G: 0.3 II. M: 3000 (Deoxycorticosterone have similar G (0.2) and 100 M) c. Corticosterone I. G: 0.3 II. M: 15 d. Prednisolone I. G: 4 II. M: 0.8 e. Dexamethasone I. G: 25 II. 0 (High affinity to glucocorticoid receptors and long half-life) f. Cortisone I. G: 0.7 II. M: 0.8 (Ganong) |
|
|
Adrenal steroid synthesis
a. Source of cholesterol b. Which enzymes are in the mitochondria and which are in the SER |
a. Source of cholesterol
I. Some is synthesized from acetate, but most is taken up. II. LDL-receptors are especially abundant in adrenocortical cells. b. Mitochondrial and SER enzymes Mitochondria 1. Cholesterol desmolase\side-chain cleavage enzyme (CYP11A1) 2. Complex of 17-alpha hydroxylase and 17-20-lyase (CYP17, Highest expression in zona reticularis produce androgens) 3. 11-beta hydroxylase (CYP11B1, Final step in glucocorticoid synthesis, not expressed in zona glomerulosa, highest expression in zona fasciculata) 4. Aldosterone synthase (CYP11B2) SER 1. 3-beta-hydroxysteroid dehydrogenase (Only thats not part of cytochrome P450 superfamily, (hydroxy)pregnenolone to (hydroxy)progesterone, and DHEA to androstenedione) 2. 21-beta-hydroxylase (For glucocorticoid and mineralocorticoid synthesis, CYP21A2) (Ganong) |
|
|
Adrenal steroid synthesis
a. Action of ACTH b. Action of ATII |
a. ACTH
1. Gs -> 2. cAMP -> 3. PKA -> 4. ↑Cholesterol ester hydrolase (CEH) 5. Release cholesterol from lipid droplets to be converted to pregnenolone by cholesterol desmolase in the mitochondria) Also increase the synthesis of the P450s involved in the synthesis b. ATII 1. AT1 receptor in zona glomerulosa -> 2. Gq -> 3. PLC -> 4. PKC -> 5. ↑Cholesterol desmolase and aldosterone synthase (Ganong) |
|
|
Adrenal steroid synthesis deficiencies
a. Congenital defects in any of the enzymes lead to ...., why b. Loss-of-function mutation of the gene for the steroidogenic acute regulatory (StAR) protein - Function of gene, effect of mutation c. 3-beta-hydroxysteroid dehydrogenase - Effect of mutation d. 17-alpha hydroxylase deficiency - Effects |
a. Congenital adrenal hyperplasia, due to increased ACTH secretion
b. Steroidogenic acute regulatory (StAR) protein I. Necessary in the adrenal and gonads but not the placenta for the normal movement of cholesterol into the mitochondria to reach cholesterol desmolase (Cholesterol desmolase is located on the matrix side of the internal mitochondrial membrane) II. Mutation -> 1. Severe congenital adrenal hyperplasia (Called congenital lipoid adrenal hyperplasia due to lipid accumulation) 2. No androgen production -> Female genitalia develops regardless of sex c. 3-beta-hydroxysteroid dehydrogenase deficiency I. Incomplete masculinization in males (Hypospadias is common) II. Partial masculinization in females (Only DHEA is present, androstenedione needs 3-beta-hydroxysteroid dehydrogenase for its conversion) d. 17-alpha hydroxylase deficiency I. No sex hormones are produced -> Female external genitalia regardless of sex II. Accumulation of glucocorticoid and mineralocorticoid steroids -> hypertension, hypokalemia (Cortisol is absent (need 17-alpha hydroxylase for its conversion), this is partly compensated by corticosterone) (Ganong) |
|
|
Enzyme deficiencies for adrenal steroid synthesis
a. 21-beta-hydroxylase deficiency - Effects b. 11-beta-hydroxylase deficiency - Effects c. Glucocorticoid treatment is idnicated in all of the virilizing forms of congenital adrenal hyperplasia. Why |
a. 21-beta-hydroxylase deficiency
I. ↓Mineralocorticoid and glucocorticoid synthesis -> specific effects, ↑ACTH II. ↑Androgens due to accumulative effect since the other pathway is blocked and effect from ACTH (Cause adrenogenital syndrome in females (from virilization), account for > 90% of enzyme deficiencies of adrenal steroid synthesis because the gene is located in the highly polymorphic site in chromosome 6 adjacent to the HLA complex) b. 11-beta-hydroxylase deficiency I. Virilization and ↑11-deoxycortisol and 11-deoxycorticosterone with mineralocorticoid activity -> salt and water retention, hypertension (2\3 of patients)) c. Repairs the glucocorticoid deficiency and inhibits ACTH secretion (Ganong) |
|
|
17-Ketosteroids
a. The major adrenal androgen b. Other 17-ketosteroids c. Which metabolite of the adrenal androgens can cause fever when it is unconjugated |
a. Dehydroepiandrosterone (DHEA)
b. 17-Ketosteroids 1. Androstenedione 2. From cortisol and cortisone by side-chain cleavage in the liver (11-oxy-17-ketosteroids) 3. Testosterone can be converted to 17-ketosteroids c. Etiocholanolone (Certain individuals have episodic bouts of fever due to periodic accumulation of unconjugated etiocholanolone) (Ganong) |
|
|
Physiologic effects of glucocorticoids
a. On intermediary metabolism b. Permissive action c. Vascular reactivity d. Water metabolism e. Blood cells and lymphatic organs |
a. On intermediary metabolism
1. ↑Protein catabolism 2. ↑Hepatic gluconeogenesis and glycogenolysis, ↑Glucose-6-phosphatase 3.Antiinsulin action in peripheral tissues (In adrenal insufficiency, fasting can cause hypoglycemia that can be fatal) b. Permissive action - Small amounts of glucocorticoids must be present for a number of metabolic reactions to occur, but glucocorticoids don't produce these actions themselves 1. For glucagon and catecholamines to exert their calorigenic effect 2. For catecholamines to exert their lipolytic effects 3. For catecholamines to produce pressor responses and bronchodilation c. Vascular reactivity I. Necessary for the responsiveness of smooth muscle to catecholamines (In its absence the capillaries dilate and have decreased vascular compensation for hypovolemia) d. Water metabolism I. Repair the accumulated water load from adrenal insufficiency (In patients who have not received glucocorticoids with severe water retention, glucose infusion may cause high fever ("glucose fever") followed by collapse and death. Glucose is metabolized -> dilute plasma -> osmotic gradient between plasma and the cells cause swelling to a dysfunctional state of the cells of the thermoregulatory centers of the hypothalamus) e. Blood cells and lymphatic organs 1. ↑Total WBC, neutrophils, RBCs, platelets 2. ↓Lymphocytes, eosinophils, and basophils (Reduced secretion of IL-2 -> ↓Lymphocyte proliferation and lymphocyte apoptosis, increased eosinophil sequestration in spleen and lungs) 3. ↓Lymph nodes and thymus (Also accelerate the maturation of surfactant in the lungs, inhibit growth, decrease GH and TSH secretion) (Ganong) |
|
|
Cushing's syndrome
a. Causes b. S&S |
a. Causes
ACTH-independent 1. Glucocorticoid-secreting adrneal tumors 2. Adrenal hyperplasia 3. Exogenous glucocorticoid treatment 4. Abnormal receptor expression on adrenocortical cells (Ie for GIP, vasopressin, IL-1..) ACTH-dependent 1. ACTH-secreting tumors of the anterior pituitary glands - Cushing's disease 2. Ectopic ACTH syndrome from lung cancer b. S&S 1. Poor muscle development (<- ↑↑Protein catabolism) 2. Thin skin and thin hair (<- ↑↑Protein catabolism) 3. Poor wound healing and minor injuries cause bruises and ecchymoses (<- ↑↑Protein catabolism) 4. Hirsutism and acne (<- ↑Adrenal androgens) 5. Changed body fat distribution I. Thin extremities II. Abdominal\truncal obesity III. Fat in neck - bufallo hump IV. Facial obesity - rounded 'moon-face' 6. Reddish-purple striae (<- From rupture of subdermal tissue of stomach due to increased subcutaneous fat deposition) 7. Glucose-abnormalities from impaired glucose tolerance to diabetes mellitus 8. Electrolytes I. Hypernatremia II. Hypokalemia (In cases of ACTH hypersecretion) 9. Hypertension (85% of patients) 10. Osteoporosis (From increased bone dissolution) 11. Mental aberrations I. Increased appetite II. Insomnia III. Euphoeria IV. Psychosis (Ganong) |
|
|
ACTH
a. Effect of ACTH on the adrenal b. Circadian rhythm - When is most secreted c. Afferent nerve pathways converging on the paraventricular nuclei to control CRH-ACTH-glucorticoid during stress |
a. Effect of ACTH on the adrenal
I. Increase output of glucocorticoids and adrenal androgens II. Increase the sensitivity of the adrenal to subsequent doses of ACTH (Single doses of ACTH do not increase glucocorticoid output in patients with hypopituitarism. Same effect with long-term treatment with exogenous glucocorticoids depressing ACTH) b. Circadian rhythm I. In the early morning (75% between 4 am and 10 am, not from 'stress' of getting up, happens before waking up, suprachiasmatic nucleus of hypothalamus regulates it) c. 1. Fibers from amygdaloid nuclei I. Mediate response to emotional stresses - fear, anxiety 2. Nociceptive pathways and the reticular formation mediate increased stress in response to injury 3. Afferents from tractus solitarius (Ganong) |
|
|
Glucocorticoids
a. What can happen when prolonged treatment with glucocorticoids (ie antiinflammatories) is stopped suddenly, why |
a. Acute adrenal insufficiency
I. The adrenal gland is atrophic and unresponsive II. The pituitary can be unable to secrete normal amounts of ACTH for as long as a month (Ganong) |
|
|
Mineralocorticoids
a. Actions b. Mechanism of action c. How can mineralocorticoids exert its effect when the affinity of its receptors to glucocorticoids is higher and the concentration of glucocorticoids is higher |
a. Actions
I. Increase the reabsorption of Na from the urine, sweat, saliva, and the contents of the colon -> Expand ECF volume II. 'Exchange' Na for K and H on the principal (P) cells of the renal tubules -> 1. Hypernatremia 2. Hypokalemia 3. Increased acidity of urine b. Mechanism of action 1. Immediate effect - Increase the activity of epithelial Na channels (ENaCs) I. Increase the insertion of these channels into the cell membrane from a cytoplasmic pool II. Via activation of the early response gene serum- and glucocorticoid-regulated kinase (sgk), also binds glucocorticoids) 2. Delayed effect - Increase mRNA of ENAC (The main effect takes 10-30 and is thus delayed) c. Mineralocortiocid-sensitive tissue (kidneys..) contain 11-beta-hydroxysteroid DH type 2 that converts cortisol to cortisone and corticosterone to its 11-oxy derivative which don't bind to the receptor (Dysfunction of this enzyme cause apparent mineralocorticoid excess (AME) due to glucocorticoids activating the mineralocorticoid receptor, licorice contains a substance that inhibits this hormone) (Ganong) |
|
|
Mineralocorticoids
a. Effects of adrenalectomy b. Effects of excess mineralocorticoids c. Escape phenomenon of excess mineralocorticoids |
a. Effect of adrenalectomy
I. Na is lost in the urine with water -> hypotension, circulatory insufficiency, fatal shock II. K is retained (Chronic adrenocortical insufficiency\Addison's disease) b. Effect of excess mineralocorticoids I. K depletion (< 2.5 mM) II. Retained Na and water (-> Na concentration is not markedly elevated since water follows) -> ECF expands, blood pressure rises (Primary hyperaldosteronism\Conn syndrome) c. Escape phenomenon of excess mineralocorticoids I. When the ECF expansion reach a certain point, Na excretion is usually increased in spite of the continued action of mineralocorticoids on the renal tubules (Probably due to increased secretion of ANP, why patients with hyperaldosteronism not normally get edema) (Ganong) |
|
|
Effects of adrenocortical hyper- and hypofunction in humans - Give name of syndrome and main effects
a. Excess androgen secretion b. Primary hyperaldosteronism c. Primary adrenal insufficiency |
a. Adrenogenital syndrome - Excess androgen secretion
I. Precoucious pseudopuberty II. Female pseudohermaphroditism b. Conn's syndrome I. K depletion and Na retention II. Weakness III. Hypertension IV. Tetany V. Polyuria VI. Hypokalemic alkalosis c. Primary adrenal insufficiency - Addison's disease I. Lose weight II. Tired III. Chronically hypotensive (-> Hearts become smaller) IV. Fasting cause fatal hypoglycemia and any stress cause collapse V. Water is retained - water intoxication VI. Pigmentation abnormalities (tan, vitiligo, on scars from lesions that occurred after the disease, of skin creases, of areolas, of pressure points (elbows), of gums) (From MSH activity mainly) (From tuberculosis, autoimmune inflammation..) (No pigmentation and milder electrolyte abnormalities in secondary and tertiary causes) (Isolated functional aldosterone deficiency is seen in 2 conditions - hyporeninemic hypoaldosteronism (renal disease), pseudohypoaldosteronism (receptor dysfunction)) (Ganong) |
|
|
Calcium metabolism
a. Involved hormones b. Ca store in the body c. Functions of free ionized calcium d. Main feature of hypocalcemia e. Factors affecting funtional calcemia levels |
a. Involved hormones
1. 1,25-Dhydroxycholecalciferol (Increase Ca uptake from intestine) 2. Parathyroid hormone (Mobilize Ca from bone, excrete P) 3. Calcitonin (Lower Ca by inhibiting bone resorption 4. Parathyroid hormone-related protein (PTHrP) (Act on one of the PTH receptors and is important in skeletal development in utero) b. 1100g\27.5 mol I. 99% in skeleton b. Functions of free ionized calcium I. Blood coagulation II. Muscle contraction III. Nerve function d. Hypocalcemia -> hypocalcemic tetany (Laryngospasm can be severe enough to result in asphyxia) e. Factors affecting functional calcemia levels 1. Plasma protein level (↓ -> ↓Ca binding -> ↑Free Ca) 2. pH (↑pH -> ↑Ionization of plasma proteins -> ↑binding of Ca -> ↓Free Ca) (Ganong) |
|
|
Calcium metabolism
a. The total body store is 1100g\27.5 mol - How much is in the rapidly exchangeable pool of the bones and how much is in the stable\slowly exchangeable pool of the bones b. Distribution in plasma c. Renal handling |
a.
I.27.2 mol in the slowly changeable pool (7.5 mmol are subject to reabsorption and accretion per day) II. 100 mmol are in the rapidly exchangeable pool (500 mmol can be rapidly mobilized to ECF) b. Distribution in plasma 1. Total diffusible - 1.34 mM I. Ionized (Ca2+) - 1.18 mM II. Complex to HCO3, citrate.. 0.16 mM 2. Total nondiffusible (protein-bound) - 1.16 I. Bound to albumin - 0.92 mM II. Bound to globulins - 0.24 mM Total 2.50 mM c. Renal handling I. A large amount is filtered II. 98-99% is reabsorbed - 60% in PCT, the rest in loop of henle and distal tubule (controlled by PTH) (Ganong) |
|
|
Phosphorus
a. Total body phosphorus b. Distribution in plasma c. Renal handling |
a. 500-800g
(85-90% in skeleton) b. Distribution in plasma 1. In organic compounds - 2\3 2. Inorganic - 1\3 I. Phosphate II. Hydrogen phosphate III. Dihydrogen phosphate c. Renal handling I. 85-90% is reabsorbed II. Most is reabsorbed by active transport in PCT (Inhibited by PTH) (Ganong) |
|
|
Bone physiology
a. Main salt b. Main protein c. Structure of cortical\compact bone d. Structure of trabecular\spongy bone |
a. Hydroxyapatite
(Ca10(PO4)6(OH)2)) b. Type 1 collagen (>90%) c. Cortical\compact bone I. Outer layer of most bone II. Blood supply via nutrient artery -> vessel in Haversian canal -> vessel in Volkmann's canals (Volkmann's canals runs transverse of osteons\haversian systems) II. Osteocytes in lacunae III. Collagen is arranged around each canal in concentric layers (80% of the bone in the body) d, Trabecular\spongy bone I. Made of spicules\plates with osteocytes sitting on them II. Nutrients diffuse from ECF into the trabeculae (Ganong) |
|
|
Bone physiology
a. The two types of bone development b. Which structure is responsible for longitudinal bone growth |
a. Bone development
1. Enchondral bone formation I. Most of the bones II. From mesenchyme via cartilage to bone 2. Intramembranous bone formation I. Clavicles, mandibles, certain bones of the skull II. Directly from mesenchyme to bone b. The epiphysial plate (Connect shalf (diaphysis) with ends (epiphyses). The epiphyses of the various bones close in an orderly temporal sequence, the last epiphyses closing after puberty) (Ganong) |
|
|
Bone formation and resorption
a. Osteoblasts - Origin, characteristics b. Osteoclasts - Origin, characteristics c. Bone-remodeling units d. Regulation of bone-remodeling e. Osteoclasts - Mechanism of resorption |
a. Osteoblasts
I. Modified fibroblasts II. Fibroblast->Osteoblast by ossification-specific factors, the most important being Cbfa1 (When its knocked out mice develop without ossification) b. Osteoclasts I. From monocytes II. Conversion is Induced by stromal cells in the bone marrow, osteoblasts and T lymphocytes which express RANKL (RANK ligand) (bind to RANK on monocytes) and secrete M-CSF (bind to c-fins on monocytes) b. Bone-remodeling units I. Combination of osteoclasts and osteoblasts in a small area that carry out bone resorption and accretion) II. Cycle takes approximately 100 days III. Responsible for changing shape IV. Related in part to the stresses and strains imposed on the skeleton by gravity (100% of the calcium in bones of infants is turned over per year, 18% in adults) d. Regulation of bone-remodeling I. PTH accelerate bone resorption II. Estrogens slow bone resorption (By inhibiting the production of bone-eroding cytokines - IL-1, IL-6, TNFalpha and stimulate TGF-beta which increase apoptosis of osteoclasts) e. Osteoclasts - Mechanism of resorption I. Attach to integrins of bone to form a sealing zone - the area within is functionally like a lysosome II. Secrete H from H-ATPase and acidic proteases III. Acidity dissolve hydroxyapatite crystals while the acidic proteases digest collagen IV. Products are transcytosed through the osteoclasts (One of the breakdown products of collagen pyridinolines can be measured in the urine as an index of the rate of bone resorption) (Ganong) |
|
|
Osteopetrosis
a. Mechanism b. Effects |
a. Mechanism
I. Osteoclasts are defective and are unable to resorb bone in their usual fashion so the osteoblasts operate unopposed b. Effects I. Steady increase in bone density II. Neurologic defects due to narrowing and distortion of foramina III. Hematological abnormalities due to crowding of the marrow cavities (Mice lacking the immediate-early gene c-fos develop osteopetrosis) (Ganong) |
|
|
Osteoporosis
a. Mechanism b. Effects\S&S c. Causes d. Treatment strategies |
a. Mechanism
I. Excess of osteoclastic function which cause loss of bone matrix b. Effects\S&S 1. ↑Incidence of fractures I. Colle's fracture II. Vertebral body III. Hip (Bones with high content of trabecular bone, which is more active metabolically) 2. Kyphosis (From vertebral body fracture with compression, 'widow's hump in elderly women with osteoporosis) c. Causes 1. Involutional osteoporosis I. Accelerated physiological loss of bone matrix with age (Males have up to 1500g calcium at age 30 and > 1000g at age 90, women have 1100 at age 30 and 600 at age 90) II. Women lose bone more rapidly after menopause (Estrogen) 2. Disuse osteoporosis I. Immobilized, space flight 3. Cushing's syndrome d. Treatments 1. Increased Ca intake 2. Selective estrogen receptor modulators (SERM) (Raloxifene is agonist at bone and antagonist at breast and uterus) 3. Moderate exercise 4. Bisphosphonates - Inhibit osteoclastic activity (Etidronate) (Ganong) |
|
|
Vitamin D
a. Vitamin D - Structure b. Vitamin D3\Cholecalciferol - Source c. Further activating steps of vitamin D3 |
a. Secosteroid - Steroid in which one of the rings is opened
(B in this case) b. Vitamin D3 - Source 1. Diet 2. From conversion of 7-dehydrocholesterol by sunlight in the skin (Transported in the plasma bound to vitamin D-binding protein (DBP)) c. 1. 25-hydroxylase in the liver I. Cholecalciferol\Vitamin D3 -> 25-hydroxycholecalciferol\calcidiol 2. 1-alpha hydroxylase in PCT of kidneys I. 25-hydroxycholecalciferol\calcidiol -> 1,25-dihydroxycholecalciferol\calcitriol (Also made in placenta, keratinocytes, and macrophages. Macrophage production is increased by pulmonary alveolar macrophages in patients with sarcoidosis) (The kidneys can also produce the almost inactive metabolite 24,25-dihydroxycholecalciferol) (Ganong) |
|
|
Calcitriol\1,25-dihydroxycholecalciferol
a. Actions b. Regulation c. Deficiency |
a. Actions
1. ↑Expression of calbindin-D proteins I. -> Increased intestinal uptake of Ca 2. ↑Ca-H ATPase of enterocytes I. To pump Ca into the ECF 3. Increase synthetic activity of osteoblasts (Necessary for normal calcification) (Also facilitate Ca reabsorption in the kidneys, receptors on immune cells (-> stimulate differentiation? Vitamin D deficient patients have more infections), keratinocytes (vitamin D is beneficial in psoriasis) b. Regulation 1. 1-alpha-hydroxylase is facilitated by PTH I. PTH secretion is increased plasma Ca is low (When PTH is low, the kidneys produce more of the inactive metabolite 24,25-dihydroxycholecalciferol) 2. PO4 inhibits 1-alpha hydroxylase directly 3. High levels inhibit expression of PTH in the parathyroid glands c. Deficiency - Inadequate mineralization 1. Rickets in children I. Weakness and bowing of weight-bearing bones II. Dental defects III. Hypocalcemia 2. Osteomalacia in adults (Low sunlight exposure or low provitamin intake) (Vitamin D-resistant rickets is caused by inactivating mutations of the receptors) (Ganong) |
|
|
Parathyroid glands
a. Location b. Cells |
a. 4 glands - 2 in superior poles and 2 in inferior poles of the thyroid gland
(Only mm size) b. Cells 1. Chief cells I. Prominent proteosynthetic apparatus (RER, GA, secretory vesicles) II. Secrete PTH III. Most abundant 2. Oxyphil cells I. Oxyphil granules II. Many mitochondrias III. Unknown function IV. Larger than chief cells (Increase with age after puberty, degenerated chief cells?) (Ganong) |
|
|
Parathyroid hormone
a. Type b. Action c. Regulation |
a. Polypeptide
b. Action 1. Stimulate osteoclasts -> stimulate bone resorption -> mobilize Ca 2. Increased renal reabsorption of Ca in distal tubules (Ca excretion is often increased in hyperparathyroidism because the amount reaching the distal tubules overwhelm the reabsorptive capacity) 3. Phosphaturic (Decrease reabsorption of phosphate in the proximal tubules (Gs and Gq-mediated effects, receptor dysfunction cause pseudophypoparathyroidism) c. Regulation 1. Hypocalcemia stimulate, hypercalcemia inhibit (Via G protein receptor for Ca. Gain-of-function mutation of this receptor -> familial hypercalciuric hypocalcemia (increased sensitivity of the parathyroid glands to plasma Ca), heterozygous inactivating mutation -> familial benign hypocalciuric hypercalcemia (decreased feedback inhibition of PTH), homozygous inactivating mutation -> neonatal severe primary hyperparathyroidism) 2. Calcitriol decrease preproPTH expression 3. Increased plasma phosphate stimulate PTH (By lowering calcitriol) (Ganong) (Ganong) |
|
|
Parathyroid hormone
a. Which mineral is needed b. Parathyroidectomy can occur inadvertently during thyroid surgery. Effects, signs c. Secondary parathyroidism - Causes |
a. Magnesium
(Accounts for the hypocalcemia that sometimes occur with hypomagnesemia) b. Parathyroidectomy I. -> Hypocalcemia, hyperphosphatemia II. Signs 1. Tetany 2. Chvostek's sign (A quick contraction of the ipsilateral facial muscles elicited by tapping over the facial nerve at the angle of the jaw) 3. Trousseau sign (Spasm of the muscles of the upper extremity that cause flexion of the wrist and thumb with extension of the fingers) (Can be elicited in mild tetany by occluding the circulation for a few minutes by a blood pressure cuff) c. Secondary parathyroidism 1. Rickets 2. Chronic renal disease (From decreased 1-alpha hydroxylase) (Ganong) |
|
|
Parathyroid hormone related protein (PTHrP)
a. Structure b. Function c. Receptor d. Hypercalcemia from malignancy - Causes |
a. Polypeptide
(2x long as PTH) b. Function 1. Stimulate cartilage cells to proliferate in utero (Via indian hedgehog) 2. Inhibit excitotoxic damage to developing neurons in the brain (Absence of PTHrP -> breasts fail to develop (PTHrP in breast milk), teeth cannot erupt (found in enamel)) c. hPTH\PTHrP receptor (PTHrP is primarily a paracrine factor, acting where it is produced. maybe PTH can't reach the sites since it don't have the same effects) d. Hypercalcemia from malignancy 1. Local osteolytic hypercalcemia (20%, from bone metastases, tumor release PGE which is the main erosive agent) 2. Humoral hypercalcemia of malignancy (80%, ↑PTHrP, cancers of breast, kidney, ovary, skin) (Ganong) |
|
|
Calcitonin
a. Source b. Structure c. Action d. Regulation e. Clinical use |
a. Source
I. Parafollicular\C cells of the thyroid gland (Ultimobranchial bodies in some animals, probably incorporation of ultimobranchial bodies in thyroid glands in humans) b. Structure I. Polypeptide (32AA, its mRNA give rise to calcitonin gene-related peptide (CGRP) in the nervous system) c. Action 1. Inhibit bone resorption by osteoclasts (-> Hypocalcemic and hypophosphatemic) 2. Calciuric (Uncertain role in humans, don't cause deficiency syndrome or hypercalcitonin syndrome, protect pregnant mother from bone loss due to bone formation in the infant and lactation?) d. Regulation 1. Stimulated by hypercalcemia 2. Stimulated by beta-adrenergic agonists, dopamine, and estrogens 3. Stimulated by gastrin, CCK, glucagon, and secretin (To inhibit postprandial hypercalcemia?, calcitonin is increased in Zollinger-ellison syndrome and pernicious anemia where the gastrin level is increased) e. Clinical use 1. Paget's disease (Where incrased osteoclastic activity trigger compensatory formation of disorganized new bone) 2. Severe hypercalcemia (Ganong) |
|
|
Other agents affecting calcium metabolism
a. Glucocorticoids b. Growth hormone c. Thyroid hormone d. Insulin |
a. Glucocorticoids
I. First lower plasma Ca by inhibiting resorption II. Later cause osteoporosis by decreasing bone formation (Inhibit protein synthesis in osteoblasts) b. Growth hormone I. Increase Ca excretion in urine but increase Ca absorption in GIT, the later effect is stronger II. IGF-1 stimulate protein synthesis in bone c. Thyroid hormones I. -> Hypercalcemia, hypercalciuria, osteoporosis d. Insulin I. Increase bone formation (Bone loss in diabetes) (Ganong) |
|
|
Osteogenesis imperfecta
a. What b. Cause c. S&S |
a. What
I. A group of connective tissue disorders of type 1 collagen b. Genetic disorder - AD c. S&S 1. Bone fragility 2. Fractures 3. Skeletal deformity 4. Blue sclerae 5. Hearing loss 6. Ligament laxity (Stedman) |
|
|
The renin-angiotensin system
a. Renin - Function, produced by b. Angiotensinogen - Produced by, levels increased by c. Angiotensin-converting enzyme (ACE) - Location, function |
a. Renin
I. Angiotensinogen -> Angiotensin I II. Formed by juxtaglomerular cells (Prorenin is also formed by many other tissues, including the ovaries, it has no known effect) (Polypeptide 340 AA, 37 kDa) b. Angiotensinogen I. Produced by hepatocytes II. Increased production by glucocorticoids, thyroid hormones, estrogens, ATII, cytokines c. Angiotensin-converting enzyme I. ATI -> ATII, inactivate bradykinin II. Most is located on endothelial cells of lung capillaries (Bradykinin acts on beta-2 receptors to produce the cough that is an side effect in up to 20% of patients on ACE inhibitors) (Carboxypeptidase) (Ganong) |
|
|
Angiotensin II
a. Half-life b. Metabolism c. Actions d. ATII receptors |
a. 1-2 minutes
b. Metabolism I. Various peptidases II. An aminopeptidase create ATIII (7 AAs) which has some activity III. Another aminopeptidase remove one more AA at the amino terminal which produce ATIV (6 AAs), also with some activity c. Actions 1. Arteriolar constriction I. -> Rise in systolic and diastolic BP (4-8x as potent as norepinephrine -> One of the most active vasoconstrictors knownt) 2. ↑Secretion of aldosterone by zona glomerulosa 3. Facilitation of the release of norepinephrine by postganglionic sympathetic neurons 4. Contraction of mesangial cells -> decrease in GFR 5. Direct effect on the renal tubules to increase Na reabsorption 6. Act on the brain to I. Decrease the sensitivity of the baroreflex (Via area postrema, a circumventricular organ outside the BBB) II. Increase secretion of vasopressin and ACTH III. Increase water intake (Via subfornical organ (SFO) and organum vasculosum of the lamina terminalis (OVLT), both are circumventricular organ outside the BBB) d. AT receptors 1. AT1 receptor I. Gq, activate tyrosine kinases II. Mediates most of the known effects - vascular, brain, adrenal gland (Via caveolin 1 -> caveolae in vascular tissue, AT1A and AT1B only demonstrated in rodents, receptors in vascular tissue is down-regulated to increasing ATII while receptors in adrenal gland are upregulated) 2. AT2 receptor I. G protein to activate phosphatases (-> antagonize growth effects, open K channels), NO -> cGMP pathway II. Higher in fetal and neonatal life, uncertain function (Angiotensin II\Angiotonin\Hypertensin) (Ganong) |
|
|
The juxtaglomerular apparatus
a. Juxtaglomerular (JG) cells - Location, function b. macula densa - What, location c. Juxtaglomerular apparatus - Members |
a. Juxtaglomerular (JG) cells
I. In tunica media of afferent arterioles as they enter the glomeruli II. Contain and secrete renin b. Macula densa I. Modified tubular epithelial cells at the point where the distal tubule is close to the glomeruli c. Juxtaglomerular apparatus 1. Juxtaglomerular cells 2. Macula densa cells 3. Lacis cells (Lacis ('network'), agranular cells containing renin, located in junction between afferent and efferent arterioles, uncertain function) (Ganong) |
|
|
Renin-Angiotensin system
a. Factors that affect renin secretion - Stimulatory, Inhibitory b. Conditions that increase renin secretion |
a. Factors that affect renin secretion
Stimulatory 1. Increased sympathetic activity via renal nerves (Beta-1-adrenergic receptors on JG cells) 2. Increased circulating catecholamines 3. Prostaglandins 4. Decreased afferent arteriolar pressure Inhibitory 1. Increased Na and Cl reabsorption across macula densa (TAL of loop of Henle, Na-K-2Cl, detect amount of Na and Cl entering loop of Henle and feedback to JG cells, via NO?) 2. Increased afferent arteriolar pressure ('Intrarenal baroreceptor', mediated via JG cells) 3. ATII (Via ATII receptors on JG cells) 4. Vasopressin b. Conditions that increase renin secretion 1. Na depletion 2. Diuretics 3. Hypotension 4. Hemorrhage 5. Upright posture 6. Dehydration 7. Cardiac failure 8. Cirrhosis (Pooling of blood in splanchnic circulation - effective hypovolemia) 9. Constriction of renal artery or aorta 10. Various psychological stimuli (Sympathetic NS-mediated) (Ganong) |
|
|
Renin-angiotensin system
a. How can the RAS be inhibited pharmacologically |
a. How can the RAS be inhibited pharmacologically
1. Inhibitors of prostaglandin synthesis - NSAIDs (Indomethacin) 2. Beta-adrenergic blockers (Proproanolol) 3. Renin-inhibitors (Pepstatin, Enalkiren) 4. ACE-inhibitors (Captopril, enalapril) 5. ATII blockers (Saralasin is non-selective, losartan is selective to AT1 receptors) (Ganong) |
|
|
Erythropoietin
a. Structure b. Action c. Sources d. Regulation of secretion e. Clinical use |
a. Glycoprotein
(165 AAs) b. Action 1. Increase rate of differentiation\maturation of committed stem cells -> Erythrocytes (EPO-sensitive committed stem cells.., cytokine receptor superfamily (tyrosine kinase), circulating mature red cells take 2-3 days to appear) (Brain - protective effect against excitotoxic damage triggered by hopxia, uterus and oviducts - mediate estrogen-dependent angiogenesis) c. Sources 1. Kidneys I. 85% II. Interstitial cells in the peritubular capillary bed 2. Liver I. 15% II. Perivenous hepatocytes (The liver cannot compensate adequately after renal failure, 90% of renal failure patients on dialysis are anemic) d. Regulation of secretion 1. Hypoxia (Maybe heme protein that stimulate transcription of EPO gene in deoxy state) 2. Androgens 3. Facilitated by catecholamines e. Clinical use I. Use epoetin alfa - a recombinant version II. For anemia associated with renal failure III. Stimulate erythrocyte production in individuals who are banking a supply of their own blood in preparation for autologous transfusions during elective surgery (Ganong) |
|
|
Natriuretic hormones
a. Location b. Types and structurem c. Actions d. Regulation of secretion e. Metabolism |
a. Location
I. Mainly cardiomyocytes of the atria b. Types 1. Atrial natriuretic peptide (ANP) I. Polypeptide (28 AAs, ring form by disulfide bond) 2. Brain natriuretic peptide (BNP) I. Similar structure (Extracted from brain first, higher concentration in cardiac tissue) (3rd one is identified and named C-type natriuretic factor, involved with paracrine functions in brain, pituitary, kidneys, and vascular endothelial cells) c. Actions 1. Increase Na excretion I. Dilate afferent arterioles and relax mesangial cells -> increase GFR II. Act on renal tubules directly to inhibit Na reabsorption 2. Increase in capillary permeability (-> Extravasation of fluid -> decline in blood pressure) 3. Relax vascular smooth muscle (Arterioles, venules) 4. Inhibit renin secretion 5. ANP mediates neural circuits in the brain that is involved in lowering blood pressure and promoting natriuresis (Oppose ATII pathways ('sympathetic'), anteromedial hypothalamus -> lower brain stem areas involved with the cardiovascular system) (NPR-A,B,C receptors) d. Regulation of secretion 1. Increased when the ECF volume is increased 2. Increased when the atria (ANP) and ventricles (BNP) are stretched 3. Increased when the body is immersed in water up to the neck (Counteract the effect of gravity on the circulation and increase CVP -> atrial pressure, RAS is simultaneously inhibited) e. Metabolism I. By neutral endopeptidase (ENP) (ENP also metabolize enkephalins, thiorphan inhibits ENP and is the active metabolite of acetorphan\racecadotril, and antidiarrheal drug that act by peripherally increasing enkephalins which has an antisecretory effect on the GIT) (Ganong) |
|
|
The pineal gland\epiphysis
a. Structure, cells, characteristics b. Formation of melatonin c. Regulation of secretion of melatonin d. Function of melatonin |
a. Structure of the pineal gland
I. Pinealocytes that secrete melatonin and neuroglia cells arranged in alveoli II. Highly permeable fenestrated capillaries III. Pineal sand\corpora arenacea\acervulus are small concretions of calcium phosphate and bicarbonate that begin to accumulate after puberty b. Formation of melatonin 1. Tryptophan -> 5-hydroxytropthan -> 5-hydroxytrypamine (5-HT)\Serotonin 2. N-acetyltransferase I. 5-hydroxytryptamine -> N-acetyl-5-hydroxytryptamine\N-acetylserotonin I. Use acetyl-CoA 3. Hydroxyindole O-methyltransferase (HIOMT) I. N-acetyl-5-hydroxytryptamine -> N-acetyl-5-methoxytryptamine\Melatonin II. Use S-adenosylmethionine (Mel 1 (Gs) and 2 (Gq) receptors) (Metabolized by liver to 6-hydroxylation followed by conjugation and by brain) c. Regulation of secretion 1. By light hitting the retina I. Low light -> ↑Melatonin, vice versa II. Light -> Retina -> retinohypothalamic tract -> suprachiasmatic nuclei of hypothalamus -> thoracic intermediolateral cell column -> superior cervical ganglion -> pineal gland) (Beta-adrenergic receptors in pineal gland is Gs mediated and cause increase in N-acetyltransferase activity) d. Function of melatonin I. Uncertain, timing signal that coordinate endocrine and other internal events with the light-dark cycle in the environment? (Can be both stimulatory or inhibitory on gonads, some pineal tumors cause sexual precocity, decline dramatically with age (<1\4 in elderly compared to 20-30s) (Ganong) |
|
|
The pituitary glands
a. Which of the anterior pituitary hormones are polypeptides or proteins and which are glycoproteins b. Which hormones are produced by the intermediate lobe c. Histology of the posterior lobe d. Histology of the intermediate lobe e. Histology of the anterior lobe |
a. Structure
I. Polypeptides\Proteins - GH, PRL, ACTH (Those not acting on a endocrine gland and the one with the strange precursor) II. Glycoproteins - TSH, LH, FSH (Made of alpha and beta subunits, alpha are from the same gene and only differs by carbohydrate residues) b. Hormones produced by the intermediate lobe 1. Alpha-MSH 2. Beta-MSH (Not secreted into the bloodstream in significant amounts, the intermediate lobe is formed from the dorsal half of Rathke's pouch, separated from the anterior lobe by the residual cleft) c. Histology of the posterior lobe I. Axons of supraoptic and paraventricular nuclei are visible II. Pituicytes (Stellate cells that are modified astrocytes) d. Histology of the intermediate lobe I. Most of its cells are incorporated into the anterior pituitary since its rudimentary in humans II. Thyroid-like follicles are found along the residual cleft e. Histology of the anterior lobe I. Interlacing cell cords II. Extensive network of sinuosidal capillaries that are fenestrated III. Granule-containing cells (Ganong) |
|
|
The anterior pituitary
a. The 2 groups of cell types and their function b. Link the 6 hormones produced to cell types and cell groups |
a. 2 groups of cell types
1. Chromophilic cells I. Active secretory cells 2. Chromophobic cells I. Many of them are secretory cells that are inactive and thus have few secretory granules II. Others are folliculostellate cells which sends processes between established cells b. Chromophilic cells Acidophilic cells 1. Somatotrope cells - GH (50% of total secretory cells, large granules) 2, Lactotrope\Mammotrope cells - PRL (10-30%, small granules) Basophilic cells 1. Corticotrope - ACTH (10%, largest granules) 2. Thyrotrope - TSH (5%, smallest granules) 3. Gonadotrope - FSH, LH (20%, intermediate granules) (Ganong) |
|
|
Proopiomelanocortin (POMC)
a. Produced by b. Which products are produced by corticotrope cells c. Which products are produced by intermediate-lobe cells |
a. Produced by
1. Intermediate-lobe cells 2. Corticotropes of the anterior pituitary (+ Hypothalamus, lungs, GIT, placenta..) (Known as POMC after the pre- segment has been cleaved in RER) b. Products of corticotrope cells 1. ACTH (Middle) 2. Beta-lipotropin hormone (beta-LPH) (carboxy terminal) 3. Beta-LPH product - beta-endorphin 4. Amino-terminal fragment product - Gamma-MSH c. Intermediate lobe cells - More processing than in corticotrope cells 1. Amino terminal fragment product - gamma-MSH 2. ACTH products - Alpha-MSH and corticotropin-like intermediate-lobe peptide (CLIP) 3. Beta-LPH products - gamma-LPH (-> beta-MSH), beta-endorphin (-> met-enkephalin) (Ganong) |
|
|
Control of skin coloration
a. Cells producing melanin and their receptor b. Ligand for receptor c. Pigment changes in hypopituitarism d. Pigment changes in Cushing's syndrome e. Albinism - Cause f. Piebaldism - What, cause g. Vitiligo - What, cause |
a. Melanocytes, melanotropin-1 receptor
b. MSHs c. Abnormal pallor (↓POMC) c. Hyperpigmentation (↑POMC) d. Albinism I. Congenital inability to synthesize melanin e. Piebaldism I. Patches of skin that lack melanin II. Congenital defects in migration of pigment cell precursors from the neural crest (Pattern of patches is also inherited) g. Vitiligo I. Progressive patches of skin without melanin II. Autoimmune (Ganong) |
|
|
Growth hormone
a. Growth hormone receptor - Type b. Most important intracellular cascade c. Effects on metabolism |
a. Member of the cytokine receptor superfamily
I. GH has 2 binding sites for receptors and cause a necessary dimerization of the receptor upon binding b. JAK2-STAT pathway (Janus kinase 2 - tyrosine kinase, STAT - Signal transducers and activation of transcription, also in insulin) c. Effects on metabolism I. General - ↑Metabolic rate II. Protein - +Nitrogen and phosphorus balance, increased protein deposition III. Fat - ↓Plasma cholesterol, ↑circulating FFAs IV. Carbohydrates - ↑Hepatic glucose output, anti-insulin effect on muscle (Ganong) |
|
|
Acromegaly - S&S
|
Acromegaly
1. Increased size of most viscera 2. Increased protein content of the body 3. Decreased fat content of the body 4. Bitemporal hemianopia 5. Prognathism and acromegalic facies (Pro-, gnathos (jaw) - protruding jaw) 6. Hirsutism 7. Gynecomastia and lactation 8. Enlarged hands and feet 9. Osteoarthritic vertebral changes (Ganong) |
|
|
Somatomedins
a. Types in humans and their function b. Similarity to insulin c. Effects of GH assumed to be mediated by GH and effects assumed to be mediated indirectly via IGF-1 |
a. Types in humans
1. IGF-1\Somatomedin c I. Skeletal and cartilage growth II. After birth III. Regulated by GH 2. IGF-2 I. Growth during fetal development (Their mRNA is expressed in the liver, cartilage...) b. Similarity to insulin I. Closely related, except that their C chains are not cleaved and they have an extra D domain (Insulin have A-C-B, C is cleaved and A-B connect by disulfide bridges) II. IGF-I receptor is very similar to the insulin receptor c. Direct and indirect effects of GH I. Direct effects 1. Na retention (Accumulate in tissues with increased protein deposition) 2. Decreased insulin sensitivity 3. Lipolysis 4. Protein synthesis 5. Epiphysial growth II. Indirectly via IGF-I 1. Insulin-like activity 2. Antilipolytic activity 3. Protein synthesis 4. Epiphysial growth (Ganong) |
|
|
Growth hormone
a. Factors regulating its secretion b. Plasma level c. Stimuli that increase secretion d. Stimuli that decrease secretion |
a. Factors regulating its secretion
1. GRH from hypothalamus 2. Somatostatin from hypothalamus 3. Ghrelin from hypothalamus - ↑GH (Involved in regulation of food intake, produced in GIT) 4. Feedback control by IGF-I on hypothalamus (↑SS), and hypophysis (↓GH) b. 2-4 ng\mL c. Stimuli that increase secretion I. Deficiency of energy substrates 1. Hypoglycemia 2. Exercise 3. Fasting II. Increase in circulating levels of certain amino acids 1. Protein meal (Or by directly infusing arginine and some others) III. Glucagon IV. Stressful stimuli 1. Pyrogens 2. Various psychological stressors V. Going to sleep VI. Estrogens and androgens (Increase GH responses to other stimuli such as arginine) (Also increased by L-dopa and the dopamine receptor agonist apomorphine (derivative of morphine used as emetic agent)) d. Stimuli that decrease secretion I. REM sleep II. Glucose III. Cortisol IV. FFAs V. Progesterones VI. GH (Ganong) |
|
|
Growth
a. The two growth periods of humans B. Cause of cessation of growth in length |
a. The two growth periods of humans
1. Infancy (Continuation of fetal growth period) 2. Late puberty just before growth stops (Due to GH, androgens, estrogens..) (Peak at 12 years for girls and 15 years for boys) b. Closure of epiphyses by estrogen |
|
|
Dwarfism - Causes
|
Dwarfism
1. Deficiency of GRH, GH, or IGF-I 2. Growth hormone insensitivity\Laron dwarfism I. Loss-of-function mutation of GH -> ↓IGF-I and IGFBP-3 (IGFBP is also GH-dependent) 3. Cretinism I. Infantile features\Failure of development of normal proportions of the body 4. Patients with precocious puberty I. Premature closure of epiphysial growth plates by excessive estrogen 5. Gonadal dysgenesis - XO 6. Constitutional delayed growth I. Caused by various bone and metabolic conditions 7. Psychosocial dwarfism\Kaspar Hauser syndrome I. From chronic abuse and neglect 8. Achondroplasia I. Short limbs, normal trunk II. Most common form of dwarfism III. AD, gene for fibroblast growth factor receptor 3 (FGFR3) 9. Excessive mineralocorticoids - Endogenous or exogenous (Ganong) |
|
|
Panhypopituitarism
a. Effect on adrenal cortex function b. Effect on Insulin sensitivity c. Effect on Water excretion d. Causes |
a. Adrenal cortex function
I. ↓Glucocorticoids -> ↓Sensitive to stress II. Basal mineralocorticoid level is maintained (at least initially, RAS) III. The ability to increase mineralocorticoid secretion in response to stress is absent b. Insulin sensitivity - Increased I. Lack antiinsulin effect of GH II. Deficiency of glucocorticoids c. Water excretion - Cause transient polyuria I. ↓GH -> ↓GFR II. ↓Thyroid hormone -> ↓Metabolic rate, ↓ACTH -> ↓Protein catabolism -> ↓Osmotically active products of catabolism are filtered and urine volume declines (Selective lesions of the supraoptic-posterior pituitary path cause diabetes insipidus) d. Causes 1. Tumors of the anterior pituitary 2. Suprasellar cysts - remnants of Rathke's pouch 3. Sheehan's syndrome (Pituitary infarction after postpartum hemorrhage, pituitary is enlarged during pregnancy, anterior pituitary blood supply is via pituitary stalk - combination of hypoperfusion and compression) (Ganong) |
|
|
Gonads
a. Function b. Produced hormones c. Gene on Y chromosome responsible for male gender, region, function |
a. Function
I. Gametogenesis II. Sex hormone synthesis b. Produced hormones 1. Testosterone - Mainly testes 2. Estrogens - Mainly ovaries 3. Progesterone - Ovaries 4. Relaxin - Ovaries during pregnancy (Loosens the ligaments of the pubic symphysis and softens the cervix) 5. Inhibin B (Polypeptide that inhibit FSH secretion) c. Gene - Testis-determining gene (Testis-determining factor (TDF)), I. Sex-determining region of the Y chromosome (SRY) II. Transcription factor 1. Gene for Mullerian inhibiting substance (MIS) (Ganong) |
|
|
Gonads
a. From which structure does the primitive gonad develop from b. Components of primitive gonad c. When does the gonad differentiate, what happens to it |
a. The genital ridge
b. Cortex and medulla c. Gonadal differentiation I. Males - 7-8th week - Medulla develops into testis, cortex regress (Leydig and sertoli cells appear, testosterone and MIS are secreted) II. Female - Cortex develops to ovary, medulla regress (Don't secrete hormones) (Ganong) |
|
|
Embryology of the genitalia
a. When does a fetus primordial genital ducts start to differentiate into male and female structures b. Development of genital ducts in male and female c. Until when are the external genitalia bipotential d. Which testosterone is responsible for internal genitalia development and which for external genitalia development |
a. Until the 7th week
b. Genital duct development I. Female 1. Mullerian duct -> Uterine tubes, uterus 2. Wolffian duct degenerate (Some persist as epoophoron and Gartner's duct\longitudinal duct of epoophoron) (In absence of MIS and testosterone) II. Male 1. Wolffian duct -> Epididymis, vas deferens (Testosterone) 2. Mullerian ligament regress (From MIS (< Sertoli cells)) c. 8th week (Thereafter the urogenital slit disappears and female genitalia form, or it remains open and female genitalia forms) d. Genitalia development I. Internal - Testosterone (And 'male brain') II. External Dihydrotestosterone (And male secondary sex characteristics) (Ganong) |
|
|
Aberrant sexual differentiation
a. Chromosomal abnormalities b. True hermaphroditism - What, cause c. Pseudohermaphroditism - What d. During which fetal period can androgen exposure cause development of male external genitalia in genetic females, what happens as a result of androgen exposure later |
a. Chromosomal abnormalities
1. Gonadal dysgenesis\Ovarian dysgenesis\Turner's syndrome - XO (Gonads are rudimentary or absent, short stature, other congenital abnormalities, no sexual maturation at puberty) 2. Seminiferous tubule dysgenesis\Klinefelter syndrome - XXY (Most common, normal male genitalia, abnormal seminiferous tubules, ↑frequency of mental retardation) 3. Superfemale - XXX (Not associated with any characteristic abnormalities) (Most often from nondisjunction in the first meiotic division) b. True hermaphroditism I. The condition in which the individual has both ovaries and testes II. Probably due to XX\XY mosaicism c. Pseudohermaphroditism I. Condition in which a individual has the genetic constitution and gonads of one sex, and the genitalia of the other II. Name after the genetic constitution and gonad (XX -> Female pseduohermaphroditism) d. 8-13 weeks, hypertrophy of clitoris (Ganong) |
|
|
Pseudohermaphroditism
a. Female pseudohermaphroditism - Causes b. Male pseudohermaphroditism - Causes |
a. Female pseudohermaphroditism
I. Congenital virilizing adrenal hyperplasia II. Maternal androgen - Virilizing ovarian tumor, exogenous source b. Male pseudohermaphroditism I. Defective testicular development (No MIS -> Female internal genitalia) II. Androgen resistance 1. 5-alpha-reductase deficiency 2. Androgen receptor defects - Complete loss of function is called testicular feminizing syndrome\complete androgen resistance syndrome (MIS -> Male internal genitalia, vagina ends blindly because there are no female internal genitalia, lack of menstruation) III. Congenital 17-alpha hydroxylase deficiency IV. Congenital adrenal hyperplasia due to blockade of pregnenolone formation (Ganong) |
|
|
Puberty
a. Puberty b. Puberty in females - Chronological steps c. The age at the time of puberty d. Puberty and its relation to leptin |
a. Puberty
I. The period when the endocrine and gametogenic functions of the gonads have developed to the point where reproduction is possible b. Puberty in females - Chronological steps 1. Adrenarche (Increase in the secretion of adrenal androgens, arche - beginning) 2. Thelarche (Development of breasts) 3. Pubarche (Development of axillary and pubic hair) 4. Menarche (the first menstrual period) c. The age at the time of puberty I. Females - 8-13 years of age II. Males - 9-14 years of age d. Relation to leptin I. Appears that a critical body weight must normally be reached before puberty can occur (Girls which lose weight in sports or anorexia nervosa stop menstruating ('stop puberty')) II. Leptin as link between body weight and puberty? (Obese mice that cannot make leptin are infertile, and their fertility is restored by injections of leptin. Leptin treatment induce precocious pubert in immature female mice) (Ganong) (Ganong) |
|
|
Precocious puberty
a. True precocious puberty - What, causes b. Precocious pseudopuberty - What, causes |
a. True precocius puberty
I. Premature normal pubertal pattern of gonadotropin secretion II. Causes 1. Constitutional (idiopathic) 2. Disorders involving posterior hypothalamus - tumor, infection, dysgenesis (Most common endocrine symptom of hypothalamic disease, lesion interrupt a pathway that normally holds pulsatile GnRH secretion in check) 3. Gonadotropin-independent precocity - Mutation causing increased sensitivity of LH receptor to GnRH b. Precocious pseudopuberty I. Early development of secondary sexual characteristics without gametogenesis II. Causes 1. Adrenal - 1a. Congenital adrenal virilizing adrenal hyperplasia 1b. Androgen-secreting tumors 1c. Estrogen-secreting tumors 2. Gonadal 2a. Leydig cell tumors of testis 2b. Granulosa cell tumors of ovary (Ganong) |
|
|
FSH and LH
a. Structure b. Receptors c. Action of FSH d. Action of LH |
a. Glycoproteins
(Alpha and beta subunit) b. Gs c. FSH I. Males - Maintain spermatogenic epithelium by stimulating Sertoli cells II. Females - Early growth of ovarian follicles d. LH I. Males - Tropic to Leydig cells II. Females 1. Final maturation of the ovarian follicles and estrogen secretion from them 2. Ovulation 3. The initial formation of the corpus luteum and secretion of progesterone (Ganong) |
|
|
Prolactin
a. Structure b. Receptor c. Action d. Hyperprolactinemia - S&S e. Regulation |
a. Protein
b. Linked to tyrosine kinase (JAK-STAT) (Superfamily of receptors that includes GH receptor and receptors for many cytokines and hematopoietic growth factors) c. Action I. Milk secretion from the breast after estrogen and progesterone priming (-> ↑Casein and lactalbumin) II. Inhibits the effects of gonadotropin (Prevent ovulation in lactating women) d. Hyperprolactinemia 1. Galactorrhea 2. Secondary amenorrhea (>15% of cases is caused by elevated prolactin) (Seen in > 70% of patients with chromophobe adenomas of the anterior pituitary) e. Regulation 1. - Prolactin-inhibiting hormone (PIH)\Dopamine (-> ↓Dopamine agonists (L-Dopa, bromocriptine, ↑Dopamine antagonists - Chlorpromazine, phenothiazine) 2. - Prolactin 3. - Nursing 4. + Pregnancy 5. + TRH and TSH (-> + hypothyroidism) (Ganong) |
|
|
The male reproductive system
a. What forms the blood-testis barrier b. Function of the blood-testis barrier c. Differences in the fluid of the lumen of the seminiferous tubules compared to plasma |
a. Blood-testis barrier
I. Tight junctions between adjacent Sertoli cells near the basal lamina (Maturing germ cells pass through without disruption of the barrier) b. Blood-testis barrier 1. Maintain different composition of fluid than plasma 2. Protects the germ cells from blood-borne noxious agents 3. Prevents antigenic products of germ cell division and maturation from entering the circulation c. Fluid in lumen of seminiferous tubules 1. ↓Protein and glucose 2. ↑Androgens, estrogens, K, inositol, glutamic acid, and aspartic acid (Ganong) |
|
|
Spermatogenesis
a. Steps b. Duration of spermatogenesis c. Secretory products of Sertoli cells and their function d. Morphology of spermatozoon |
a. Spermatogenesis
1. Mitotic division of spermatogonium to primary spermatocyte 2. Meiotic division of the primary spermatocyte to secondary spermatocyte and then to spermatid 3. Spermiogenesis - Maturation of spermatid to spermatozoa (Spermiogenesis is in folds of Sertoli cells, only part dependent on androgens) (Further maturation and increase in motility in epididymis and female genital organs (called capacitation here)) b. 74 days c. Secretory products of Sertoli cells 1. Androgen-binding protein (ABP) - Maintain high and stable concentration of androgens in the tubular fluid 2. Inhibin - Inhibits FSH secretion (Type A and B, members of the TGF-beta superfamily of dimeric growth factors. Also include MIS and activins (activins are active in embryonal life, in the brain, and in development of leukocytes)) (Studied for use as male contraceptives) 3. Aromatase (CYP19) (Not secreted, source of estrogen in lumen) 4. MIS - Regression of the mullerian ducts in males during fetal life d. Spermatozoon - 4 parts 1. Head - Acrosome, nucleus, 5 um 2. Middle piece - Mitochondria, 5 um 3. Principal piece - 50 um (CatSper - cAMP-mediated Ca-channel) 4. End piece - 5 um (65 um total) (Ganong) |
|
|
Semen
a. Sperm count b. Produced by c. Average volume per ejaculate d. Components |
a. 100 million\mL
(With < 20% abnormal) (50% with counts < 40 million\mL are sterile, almost all < 20 million\mL are sterile) b. Produced by 1. Seminiferous tubules 2. Seminal vesicles (60%) 3. Prostate (20%) 4. Cowper's gland 5. Urethral glands c. 2.5-3.5 mL d. Components 1. From seminal vesicles I. Fructose II. Prostaglandins III. Ascorbic acid 2. From prostate I. Citric acid II. Zinc III. Acid phosphatase IV. Fibrinogenase and fibrinolysin V. Prostate-specific antigen (PSA) (Serine protease, hydrolyze the sperm motility inhibitor semenogelin. Elevated plasma levels in prostate cancer, BPH, and prostatitis) (Ganong) |
|
|
The male reproductive system
a. Ejection is Initiated by b. Neurotransmitters released by the pelvic splanchnic nerves\nervi erigents to trigger erection c. Ejaculation - Components |
a. Initiated by
I. Afferents from the genitalia II. Descending tracts that mediate erection in response to erotic psychological stimuli b. Neurotransmitters I. Acetylcholine and VIP (vasodilator) II. Nonadrenergic noncholinergic fibers have NO synthase (Sildenafil inhibits PDE5. PDE6 is found in the retina, and one side effect of sildenafil is transient loss of the ability to discriminate between blue and green) c. Ejaculation 1. Emission I. The movement of the semen into the urethra II. Sympathetic response, hypogastric nerves III. Contraction of the smooth muscle of the vasa deferentia and seminal vesicles 2. Ejaculation proper I. The propulsion of the semen out of the urethra at the time of the orgasm II. Skeletal muscle - bulbocavernosus (Ganong) |
|
|
Testosterone
a. Secretion per day in normal adult males b. Form in plasma c. Fate\metabolism d. Actions |
a. 4.9 mg\day
(300-1000 ng\dL\10.4-34.7 nM in adult males, 30-70 ng\dL in adult females) b. Form in plasma I. Bound to gonadal steroid-binding globulin (GBG)\Sex-steroid binding globulin - 65% (Also binds estradiol) II. Bound to albumin - 33% III. Free - 2% (Androstenedione has 7% free, the rest binds mainly to albumin) c. Fate\metabolism 1. Converted to dihydrotestosterone in some target tissues by 5-alpha-reductase type 1 or 2 2. Aromatized to estradiol by aromatase 3. Converted to 17-ketosteroids and excreted in the urine (Androsterone (20% potency of testosterone) and its isomer etiocholanolone mainly (0%)) (Not all 17-ketosteroids are androgens (etiocholanolone) and not all androgens are 17-ketosteroids) d. Actions 1. Male characteristics during fetal development 2. Feedback effect on pituitary LH 3. Develop and maintain secondary sexual characteristics 4. Protein-anabolic growth promoting effect 5. Maintain spermatogenesis along with FSH (Ganong) |
|
|
Testosterone
a. Effects on male secondary sex characteristics b. Anabolic effects c. Which effects are mediated by testosterone and which are mediated by dihydrotestosterone d. Dihydrotestosterone - Mechanism of higher potency than testosterone |
a. Effects on male secondary sex characteristics
1. Enlarge and increase activity of all sex organs - Penis, testis, prostate, seminal vesicles, Cowper's gland 2. Deepen voice (Anabolic effects - Larynx enlarge, vocal cords increase in length and thickness) 3. Hair growth I. +Beard, facial hair, pubic hair, axillary hair, chest hair II. -Hairline on scalp recedes anterolaterally 4. Mental - More aggressive, interest in opposite sex 5. Body conformation I. Broader shoulders II. +Muscle 6. Skin - Sebaceous gland secretion thickens and increase (By dihydrotestosterone via 5-alpha-reductase in target tissues) b. Anabolic effects I. Increase synthesis and decrease catabolism of protein -> ↑Rate of growth II. Moderate retention of most electrolytes and water (Na, K, Ca, sulfate, P) (Don't fuse epiphyses of long bones, appears to be estrogen-mediated) c. Effects I. Testosterone 1. Gonadotropin feedback 2. Spermatogenesis, 3. Internal sexual differentiation 4. Anabolic effect 5. Male sex drive and libido II. Dihydrotestosterone 1. External virilization 2. Secondary sexual characteristics d. Dihydrotestosterone I. Bind to same intracellular receptor as testosterone but has higher affinity (Type 1 5-alpha reductase in skin and scalp, type 2 in genital skin, prostate..) (Ganong) |
|
|
5-alpha-reductase
a. Types and their distribution b. 5-alpha-reductase inhibitor, use |
a. 5-alpha reductase
1. Type 1 - Skin and scalp 2. Type 2 - Prostate, genital skin, other genital tissue b. Finasteride, benign prostatic hyperplasia (Finasteride has highest affinity for type 2) (Ganong) |
|
|
The male reproductive system
a. Sources of estrogens b. Cryptorchidism - Factors involved in descent c. Cryptorchidism - Complete or incomplete - % in newborns, 1 year olds, and puberty |
a. Sources of estrogen in males
1. Estradiol - >80% from extragonadal aromatization 2. Estrone - >95% from extraadrenal aromatization 3. Rest from Leydig cells b. MIS (For descent to the inguinal region, descent from the inguinal region to the scrotum depend on other factors (androgens?), facilitated by administration of gonadotropic hormones) c. Cryptorchidism I. Newborn - 10% II. 1 year - 2% III. Puberty - 0.3% (Early treatment is recommended despite these figures because the incidence of malignant tumors is higher in undescented than scrotal testes and because after puberty the higher temperature in the abdomen eventually cause irreversible damage to the spermatogenic epithelium) (Ganong) |
|
|
The female reproductive system
a. Terminology of follicle after ovulation b. Number of follicles - Fetal development, birth, puberty c. Number of ovarian cycles during a lifetime d. Sequence of meiosis |
a. Terminology of follicle after ovulation
1. Corpus hemorrhagicum -> 2. Corpus luteum 3. Corpus albicans b. Number of follicles I. Fetal development - 7 million (Many undergo atresia\involution) II. Birth - 2 million (50% are atretic) III. Puberty - 300 000 c. 500 d. Sequence of meiosis 1. Undergo meiosis 1 during fetal development but are arrested in prophase 2. Just before ovulation - Complete meiosis 1, arrested in metaphase 3. Meiosis 2 is completed when a sperm penetrates the oocyte |
|
|
The female reproductive system
a. The uterine cycle - Its 2 stages and the characteristic changes that take place b. Arterial supply of the endometrium c. Mechanism of menstruation |
a. The uterine cycle
1. The proliferative phase - 5-14 day I. The endometrium increase rapidly in thickness II. The uterine glands are drawn out by the increased thickness so that they lengthen (Represents restoration of the epithelium from the preceding menstruation) 2. The secretory phase - 14-28 day I. Endometrium become more vascularized and slightly edematous II. The glands become coiled and tortuous and begin to secrete a clear fluid (Phase represent preparation of the uterus for implantation of the fertilized ovum) (Resulting from increased estrogen and progesterone from corpus luteum) (Very constant at 14 days, most variation in the proliferative phase) b. Arterial supply of the endometrium 1. Spiral arteries I. Long, coiled II. Supply stratum functionale (The superficial 2\3 of the endometrium that is shed during menstruation) 2. Basilar arteries I. Short, straight II. Supply stratum basale (The part that is not shed) c. Mechanism of menstruation 1. Degeneration of corpus luteum -> Endometrium becomes thinner -> Adds to the coiling of the spiral arteries 2. Spasm of the vascular walls (Locally released prostaglandins - infusion of PGF2alpha produce endometrial necrosis and bleeding) (Ganong) |
|
|
Menstruation
a. Duration of menstrual flow b. Content of menstruation c. Volume of menstruation |
a. 3-5 days
b. Content of menstruation 1. Mostly arterial blood 2. Tissue debris 3. Prostaglandins 4. Fibrinolysin (Fibrinolysin prevents clotting in the menstrual blood) c. 30 mL (Loss of > 80 mL is abnormal) |
|
|
The female reproductive system
a. Cyclic changes in the uterine cervix b. Cyclic changes in the breast c. Intercourse - Sensation d. What happens during orgasm |
a. Cyclic changes in the uterine cervix
I. The mucosa don't undergo cyclic desquamation II. Estrogen makes the mucus thinner, more elastic (spinnbakeit), and more alkaline -> The mucus is thinnest at the time of ovulation (Promote survival and transport of sperm) II. Progesterone makes it thick and cellular -> Thick after ovulation and during pregnancy (The same changes in mucus is seen to a lesser extent in vaginal mucosa as well. + Vaginal epithelium cornifies under influence of estrogen and proliferates under influence of progesterone) b. Cyclic changes in the breast 1. Estrogens cause proliferation of mammary ducts (The breast swelling, tenderness, and pain experienced by many women during the 10 days preceding menstruation are probably due to distention of the ducts, hyperemia, and edema of the interstitial tissue of the breast) 2. Progesterone cause growth of lobules and alveoli c. Intercourse - Sensation I. Tactile sensation from labia minora and clitoris II. The upper part of the vagina is sensitive to stretch (Reinforced by tactile stimuli of the breast and psychological stimuli) d. Orgasm I. Autonomically mediated rhythmic contractions II. Pudendal nerve-mediated contractions of bulbocavernosus and ischiocavernosus (Ganong) |
|
|
Ovulation and fertility
a. Indicators of ovulation b. Fertility during different stages of the ovulatory cycle |
a. Indicators of ovulation
1. Rise in basal body temperature I. Starts 1-2 days after ovulation II. Caused by progesterone which is thermogenic III. Only slight increase - decimals c. Fertility during different stages of the ovulatory cycle 1. > 35% chance of pregnancy of intercourse from 2 days before ovulation to one day after 2. Decreased chance on 3-5 day before ovulation (8% on the fifth day) (-> Sperm can survive in the female genital tract and fertilize the ovum for up to 120 hours before ovulation) (Ovum can survive for 72 hours, but it is fertilizable for a much shorter period) (Ganong) |
|
|
Ovarian hormones
a. Estrogens - Naturally occurring b. Estrogens - Structure c. Estrogens - Sources d. Estrogen production in the follicle |
a. Estrogens
1. Estradiol\17-beta-estradiol 2. Estrone 3. Estriol b. Estrogens - Structure I. 18 carbons II. Lack methyl group at 10 position III. Lack keto-configuration in the A ring c. Estrogens - Sources 1. Granulosa cells of the ovarian follicles 2. Corpus luteum 3. Placenta 4. Peripheral conversion of androstenedione to estrone - Fat, liver, muscle, brain (Produced by aromatase\CYP19. Aromatase converts testosterone to estradiol and androstenedione to estrone) d. Estrogen production in the follicle I. LH -> Gs on theca interna cells -> ↑Androstenedione production 1. Androstenedione is converted to estradiol and enter the circulation 2. Androstenedione is supplied to the granulosa cells which converts it to estradiol and secretes it into the follicular fluid II. FSH -> Granulosa cells -> ↑Aromatase and ↑estradiol secretion (LH also stimulate their estradiol production) (Ganong) |
|
|
Estrogens
a. Distribution in plasma b. Metabolism c. Secretion - The two peaks |
a. Distribution in plasma
I. Bound to albumin - 60% II. Bound to Gonadal steroid-binding globulin (GBG) - 38% III. Free - 2% b. Metabolism I. Converted to glucuronide and sulfate conjugates -> excreted in urine (Also enterohepatic circulation) c. Secretion - The two peaks 1. Just before ovulation (Along with LH and FSH, 10x in early follicular phase) 2. Midluteal phase (Ganong) |
|
|
Estrogen
a. Effects on the female genitalia - Uterine tubes, Uterus except endometrium b. Effects on endocrine organs c. Effects on the CNS d. Other effects |
a. Effects on the female genitalia
I. Uterine tubes - Increased motility II. Uterus 1. ↑Smooth muscle 2. ↑Activity and excitability of smooth muscle 3. ↑Sensitivity to oxytocin b. Effects on endocrine organs 1. Inhibit FSH secretion 2. Negative or positive feedback for LH 3. ↑TBG 4. Breast - Duct growth, pigmentation of the areolas (Largely responsible for breast enlargement at puberty - 'GH of breast') (Given in high doses estrogen interfere with implantation and is used as 'morning-after contraception') c. Effects on the CNS 1. Increase libido (By direct effect on certain neurons in the hypothalamus (suprachiasmatic nuclei?). Increase the proliferation of dendrites and the number of synaptic knobs) d. Other effects 1. Salt and water retention (Salt and water retention is higher in the follicular phase, but aldosterone is also slightly increased) 2. Make sebaceous gland secretions more fluid and thus counter testosterone's acne-genic effect 3. Plasma cholesterol-lowering effect 4. Vasodilating effect via production of NO 5. Closure of epiphysial plates (The liver palms and spider angiomas seen in advanced liver disease are due to estrogen accumulation) (Ganong) |
|
|
Estrogens
a. Receptors b. Selective estrogen receptor modulators (SERMs) |
a. Receptors
I. 2 receptors ER-alpha and ER-beta, coded for by genes on different chromosomes II. Members of the nuclear receptor superfamily III. Form homo- and heterodimers IV. Different expression in different tissues b. SERMs I. Both agonist and antagonist on different estrogen receptor combinations I. Tamoxifene and raloxifene are bone-preserving, but tamoxifen does not stimulate the breast, and raloxifene does not stimulate the breast or uterus (Ganong) |
|
|
Progesterones
a. Structure b. Sources c. Distribution in plasma d. Metabolism |
a. C21 steroid
b. Sources 1. Corpus luteum 2. Placenta 3. Small amounts from follicle, testes, and adrenal cortex (Follicle - Theca cells provide pregnenolone to the granulosa cells, which convert it to progesterone) c. Distribution in plasma I. Bound to albumin - 80% II. Free - 2% III. Bound to corticosteroid-binding globulin - 18% d. Metabolism 1. Converted in the liver to pregnanediol and conjugated to glucuronic acid -> 2. Excreted in the urine (Ganong) |
|
|
Progesterone
a. Actions on uterus b. Actions on the breasts c. Other actions d. Mechanism of action |
a. Action on uterus
I. Progestational changes in endometrium II. Cyclical changes in cervix (And vagina) III. ↓Estrogen receptors in endometrium (And increase metabolism of estradiol) IV. Antiestrogenic effect on the myometrium 1. ↓Excitability 2. ↓Sensitivity to oxytocin 3. ↑Membrane potential b. Actions on the breasts I. Stimulate development of lobules and alveoli (Induce differentiation of estrogen-prepared ductal tissue) c. Other actions I. Feedback inhibition on LH (Large doses prevent ovulation) II. Thermogenic (Rise in body temperature at the time of ovulation) III. Stimulate respiration (The alveolar pCO2 falls as progesterone secretion rises in pregnancy) IV. Natriuresis (In large doses, block action of aldosterone on the kidney?) d. Mechanism of action I. Nuclear receptor superfamily II. The receptor is bound to a heat shock protein in the absence of the steroid, and progesterone binding releases the heat shock protein (The synthetic steroid mifepristone\RU 486 bind to the receptor but does not release the heat shock protein and block binding of progesterone) (Ganong) |
|
|
Control of ovarian function
a. GnRH secretion - Characteristics, effects b. GnRH secretion - Regulation c. Luteolysis - The regression of corpus luteum 3-4 days before menses. Mechanism |
a. GnRH secretion
I. Pulsatile - Frequency and amplitude determines effect II. Stimulate the secretion of FSH and LH III. Constant administration cause down-regulation of the GnRH receptors in the anterior pituitary and LH secretion declines to zero (-> Mechanism for long-acting GnRH analogs to inhibit LH secretion in precocious puberty and prostate cancer) b. GnRH secretion - Regulation I. Frequency is increased by estrogens (The frequency increases late in the follicular phase of the cycle, culminating in the LH surge which cause ovulation) II. Frequency is decreased by progesterone and testosterone (The frequency decrease in the secretory phase) c. Mediated by PGF2alpha and facilitated by endothelin-1 (ET-1) (PGF2alpha is also involved in the necrosis of endometrium prior to menses) (Ganong) |
|
|
Contraceptive methods
|
Contraceptive methods
1. Vasectomy (0.02) 2. Tubal ligation (0.13) 3. Oral contraceptives I. > 50 mg estrogen (ethinyl estradiol) and progestin (norethindrone) (0.32) II. < 50 mg estrogen and progestin (0.27, hinder ovulation by negative feedback on gonadotropins, progestins make the cervical mucus thick and unfavorable for sperm migration) III. Progestin only (1.2, implants of ie levonorgestrel are inserted under the skin and can prevent pregnancy for up to 5 years) 3. IUD - Loop, Copper (1.4, copper is spermatocidal, prevent sperms from fertilizing ova) 4. Diaphragm (1.9) 5. Condom (3.6) 6. Withdrawal (6.7) 7. Spermicide (11.9) 8. Rhythm (15.5) (Failure per 100 woman-years) (Ganong) |
|
|
Abnormalities of ovarian function
a. Anovulatory cycles - When is it physiological b. Primary amenorrhea c. Secondary amenorrhea - Causes d. Hypomenorrhea e. Menorrhagia f. Metrorrhagia g. Oligomenorrhea h. Dysmenorrhea |
a. Anovulatory cycles
I. First 1-2 years after menarche II. Before menopause b. Primary amenorrhea I. Condition where menstruation has never occurred c. Secondary amenorrhea 1. Pregnancy 2. Emotional stimuli and changes in the environment 3. Hypothalamic disorders 4. Pituitary disorders 5. Primary ovarian disorders 6. Various systemic diseases d. Hypomenorrhea I. Scanty flow during menstruation e. Menorrhagia\Hypermenorrhea I. Abnormally profuse flow during menstruation f. Metrorrhagia I. Bleeding from the uterus between periods g. Oligomenorrhea I. Reduced frequency of periods h. Dysmenorrhea I. Painful menstruation (Most of the symptoms are due to accumulation of prostaglandins in the uterus, and symptomatic relief has been obtained by treatment of prostaglandin synthesis inhibitors) (Ganong) |
|
|
Pregnancy
a. Fertilization - Most common location b. Steps of fertilization c. Acrosomal reaction d. How is polyspermy prevented |
a. Ampulla of uterine tube
(Fimbria->Ampulla->Isthmus) b. Steps of fertilization 1. Chemoattraction of the sperm to the ovum by substances produced by the ovum 2. Adherence of the sperm to the zona pellucida 3. Penetration of the zona pellucida and the acrosome reaction 4. Adherence of the sperm head to the cell membrane of the ovum, with fusion and penetration of the nucleus of the sperm into the ovum (Fusion is mediated by fertilin, a protein on the surface of the sperm head that resembles the viral fusion proteins) c. Acrosomal reaction I. Initiated by binding of sperm to receptors in zona pellucida II. Refers to the breakdown of the acrosome (lysosome-like organelle) - Various enzymes are released, including acrosin (trypsin-like protease) d. Prevention of polyspermy I. Fusion of sperm-ovum -> 1. Reduction in the membrane potential of the ovum that prevents polyspermy - Short-term 2. Structural changes in the zona pellucida - Long-term |
|
|
Pregnancy
a. Mechanisms which inhibit the mother from rejecting the 'fetal graft'. The fetus is in effect a transplant of foreign tissue with its own genetic material, into the mother b. Infertility - Causes |
a. Mechanisms which inhibit the mother from rejecting the 'fetal graft'
1. Placental trophoblast excress HLA-G, a nonpolymorphic gene. (Instead of class I and II MHC genes which is polymorphic) 2. There is a Fas ligand on the surface of the placenta which cause apoptosis in T cells binding to it b. Infertility I. Male - 30% II. Female - 45% III. Both - 20% IV. Idiopathic - 5% (Ganong) |
|
|
Pregnancy
a. Hormones produced by corpus luteum of pregnancy b. Human chorionic gonadotropin (hCG) c. Human chorionic somatomammotropin (hCS) - Produced by, function |
a. Corpus luteum of pregnancy
I. Estrogens II. Progesterone III. Relaxin (Relaxin helps maintain pregnancy by inhibiting myometrial contractions, removal of the ovaries before 6 weeks of pregnancy cause abortion) b. hCG I. Produced by syncytiotrophoblast II. Detectable as early as 6 days after conception - basis for pregnancy tests (Can be detected in the urine as early as 14 days after conception) III. Structural homologism to LH, FSH, and TSH - Glycoprotein made up of alpha and beta subunits IV. Mostly LH-like activity c. Human chorionic somatomammotropin (hCS)\Human placental lactogen (hPL) I. Produced by syncytiotrophoblast II. Similar structure to GH (Appears that hCS, GH, and PRL have evolved from common gene) III. Large amount in maternal blood, low in fetal blood IV. Actions 1. ↑Anabolism as documented by nitrogen retention 2. ↑Lipolysis 3. ↓Glucose utilization (2,3 divert energy to the fetus) 4. Suppress maternal GH |
|
|
Pregnancy
a. Placental hormones b. The fetoplacental unit c. Duration |
a. Placental hormones
1. hCG 2. hCS 3. Progesterone 4. Estrogens 5. POMC -> CRH, beta-endorphin, alpha-MSH, dynorphin A 6. GnRH and inhibin (Thought to act in a paracrine fashion to regulate hCG) 7. Leptin (Trophoblast and amnion cells) 8. Prolactin b. The fetoplacental unit I. Interaction of the placenta and the fetal adrenal gland in the formation of steroid hormones II. 3 steps 1. Placenta - Cholesterol -> Pregnenolone -> Progesterone 2a. Fetal adrenal gland - Progesterone -> Cortisol, Corticosterone 2b. Fetal adrenal gland - Pregnenolone -> Dehydroepiandrosterone sulfate (DHEAS) and 16-hydroxy-DHEAS\16-OHDHEAS (The fetal liver provide some pregnenolone and does some of the 16-hydroxylation) 3. Liver - 16-OHDHEAS -> Estriol, DHEAS -> Estradiol (Estriol is the main estrogen formed) c. Duration I. 270 days from fertilization II. 284 days (40 weeks\10 months) from the first day of the last menstrual period |
|
|
Parturition
a. Mechanism of onset of labor b. How can premature labor be postponed pharmacologically |
a. Mechanism of onset of labor
I. ↑Circulating estrogens -> Uterus 1. ↑More excitable 2. ↑Number of gap junctions between myometrial cells 3. ↑Prostaglandins (-> uterine contractions) 4. ↑Number of oxytocin receptors (Increase more than 100-fold during pregnancy, peak during early labor, uterine distention itself may increase the number of receptors) I. The circulating oxytocin responds to the increase in oxytocin receptors by initiating a positive-feedback cycle 1. ↑Uterine contractions - Directly and indirectly via ↑prostaglandin synthesis -> 2. Distention of cervix and vagina -> 3. Afferent stimuli from cervix and vagina -> 4. Increased secretion of oxytocin -> 1. (Voluntary contraction and spinal reflexes also aids) (↑ACTH in the fetus is somehow involved in triggering the onset of labor. By increasing glucocorticoids it also matures the fetus' lungs) b. How can premature labor be postponed pharmacologically I. Administration of 17-alpha-hydroxyprogesterone (Relax uterine smooth muscle inhibit the action of oxytocin on the smooth muscle, and reduce the formation of gap junctions between muscle fibers) |
|
|
Lactation
a. Development of the breasts - Involved hormones b. Role of prolactin and oxytocin c. Initiation of lactation after delivery d. Effect on menstrual cycles |
a. Development of the breasts
1. Estrogens - Proliferation of the mammary ducts 2. Progesterone - development of the lobules (+ Vague anabolic role of prolactin) b. Role of prolactin and oxytocin I. Prolactin - ↑Production and secretion II. Oxytocin - Contraction of the myoepithelial cells lining the duct walls -> ejection of milk c. Initiation of lactation after delivery I. 1-3 days after delivery II. Mechanism 1. Parturition -> Loss of placenta -> ↓Circulating estrogens -> Milk production (Estrogen antagonize the milk-producing effect of prolactin, estrogen can be given to stop lactation) (Suckling also evoke prolactin secretion in addition to oxytocin release) d. Effect on menstrual cycles I. Prolactin inhibits GnRH secretion, GnRH action on the pituitary, and antagonizes gonadotropins (Women who nurse regularly have amenorrhea for 25-30 weeks) (Chiari-Frommel syndrome - persistence of lactation (galactorrhea) and amenorrhea in women who do not urse after delivery. Genital atrophy? Persistent prolactin secretion) (Ganong) |
|
|
Gynecomastia
a. Gynecomastia b. Physiological causes c. Pathological causes |
a. Gynecomastia
I. Breast development in the male I. More commonly bilateral b. Physiological causes 1. Newborns - 75% I. Transplacental passage of matenral estrogens 2. Puberty - 70% I. Mild form 3. Many men > 50 years c. Pathological causes 1. Androgen resistance 2. Estrogen-secreting tumors 3. Eunuchoidism 4. Hyperthyroidism 5. Liver cirrhosis 6. Digitalis (Cardiac glycosides are weakly estrogenic) (Characterized by increased estrogen-androgen ratio -> from ↑estrogens or ↓androgens) (Ganong) |

