![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
What are fats (mostly triglycerides) broken down into
|
monoglycerides and free fatty acids (FFAs)
|
|
|
4 accessory organs of the GI tract
|
salivary glands
pancreas liver gallbladder |
|
|
role and difference of endo and exocrine pancreas functions
|
EXOcrine (acinar cells): secrete dig juices & enzymes important in hormonal secretion...coordinate digestion....via DUCTS
ENDOcrine (islets of Langerhan's): secrete hormones directly into BLOOD (endo-no ducts!) |
|
|
which 2 enteric plexuses lie within the GI tract
in which layers of the GI tract wall |
SUBMUCOSAL plexus
MYENTERIC plexus- between walls of muscularis externa (mediates shortening) |
|
|
whats the myenteric & digastric reflexes
|
mastication stiulates salive, taste buds --> increases gastric, pancreatic & bile secretions
|
|
|
3 main salivary glands, which responsible for most of the salivary secretions
|
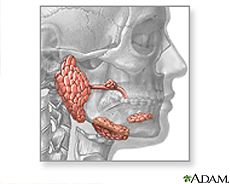
★SUBMANDIBULAR 70%★
Sublingual parotid |
|
|
primary & secondary secretions by salivary glands are via which cells
|
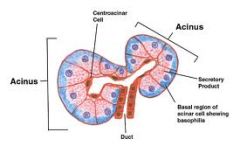
primary secretions- ACINUS
secondary- DUCT cels |
|
|
how is the saliva from acinus cells modified by duct cells
is saliva or plasma more diluted |
ACINUS secretes Na, K, Cl, HCO3 fluid
DUCT cells remove Na & Cl= dulited, ↓ NaCl than plasma |
|
|
6 functions of saliva
|
lubrication
solvent (taste) antibacterial digestion (amylase - carbs) neutralisation (HCO3) sucking |
|
|
what substrate is digested my saliva
by what enzyme |
carbohydrates
amylase |
|
|
control of saliva secretions can be due to simple unconditioned and acquired conditioned reflexes
differentiate the 2 & their signalling pathways |
SIMPLE: chemo/ pressure RECEPTORSin mouth --> afferents --> medulla (salivary centre)
ACQUIRED: think/ smell/ see/ hear--> cerebral CORTEX --> medulla ---> both impulses via extrinsic autonomic nerves (symp & parasym) |
|
|
control of saliva if due to 1)reflexes (simple & acquired) & 2) ANS
describe 2) para and symp ANS control of saliva secretions: - which nerves - receptors - type of saliva secreted |
PARA: dominant role---> facial CN VII & glossopharyngeal CN IX --> M3 - Gq - phospholiapse C ---> large watery, enzyme-rich
SYMP: stress---> superior cervical postganglionic fibres --> B1- Gs - adenylyl cyclase ---> small thick, mucus-rich |
|
|
what stimulates the upper oesophageal (cricopharyngeal) sphincter to open in swallowing
|
pressure stimulates PHARYNGEAL PERSSURE RECEPTORS ---> afferents to medulla ---> efferents
|
|
|
wheres the swallowing centre loc
|
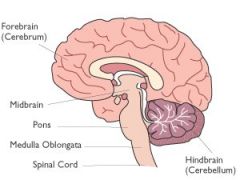
medulla oblongata
|
|
|
what does oesophagus secrete
from which layer in wall function |

MUCUS from submucosal glands
- lubrication - protect epithelium from acid & enzyme attack |
|
|
stomach is the starting point for which substrate digestion
by which substances/ enzymes |
PROTEIN
by pepsin & HCl |
|
|
areas of the stomach
|

|
|
|
what substance does stomach produce
how much gastric juice secreted per day, where from |

CHYME
~2L/day from gastric PITs & GLANDs |
|
|
how does the stomach contraction come about
|
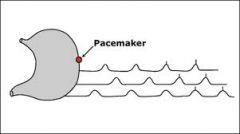
PACEMAKER cells of CAJAL in FUNDUS establish basal electrical rhythm (BER)
ALL or nothing spreads continuous 3/min |
|
|
stomach emptying controlled by 1) gastric & 2) duodenal factors
what factors are these |
1) GASTRIC: distension ----thick consistency
2) DUODENAL: neuronal---hormonal |
|
|
duodenal factors control gastric emptying via hormonal and neuronal control. Which stimuli within the duodenum drive these responses?
|
- FAT - delay requried
- ACID- delay for neutralising - HYPERTONICITY- osmotically active chyme reduces plasma vol in intestine - DISTENSION |
|
|
how do the gastric glands differ in the oxnytic mucosa (fundus & body) compared with the pyloric gland area (antrum)- i.e which cells present
|
1) oxnytic mucosa (fundus & body): parietal & enterochromaffin-like (ELC) cells
2) pyloric gland area (antrum): G & D cells NB: both contain Cheif cells |
|
|
what do these cells secrete:
- cheif cells - parietal cells - enterochromaffin-like cells - G cells - D cell |
chief- dig enzymes (pepsinogen)
parietal- HCl & intrinsic factor ECL- histamine G- gastrin D- somatostatin |
|
|
what are the functions of chief cell secretions
|
pepsinogen digests protein (when activated by HCl from parietal cells)
|
|
|
whats the function of parietal cell secretions (oxnytic mucosa - fundus & body)
|
HCl- activates pepsinogen (from chief cells)
intrinsic factor- binds vitB12 (allows absorption in the terminal ileum) |
|
|
whats the function of the ECL cell secretions (oxyntic mucosa- fundus & body)
via which receptor |
HISTAMINE- stimulates HCl secretions
via H2 receptors on parietal cells |
|
|
whats the function of gastrin secretions (pyloric gland area- antrum)
via which receptors & where |
GASTRIN- stimulates HCl secretion from parietal & histamine from ECL cells
via Gastrin receptors on ECL and parietal cells |
|
|
whats the function of D cell secretions (from pyloric gland area of antrum)
|
SOMATOSTATIN: INHIBITS HCl secretion from parietal & histamine from ECL cells
via Gastrin receptors on both cells- BETWEEN meals |
|
|
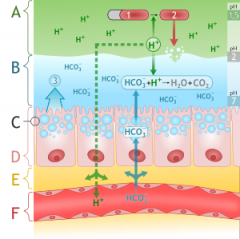
which 5 pumps are present in parietal cells for HCl secretion (& production)
|

|
|
|
which enzyme present in parietal cells makes hydrogen bicarbonate
how does it exit paritel cells |
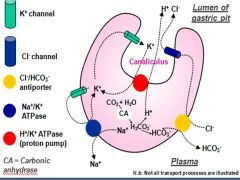
carbonic anhydrase --> HCO3- --> Cl-/HCO3- antiporter
|
|
|
which direction does the Na/K ATPase pump ions at the basal side of parietal cells
|
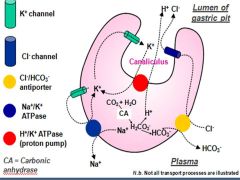
Na+ --> OUT to basal side
K+ --> IN (then --> lumenal side via K + channels--> back in via H/K ATPase) |
|
|
which ion is recycled by parietal cells, the gradient of which is used to power H/K ATPase
|
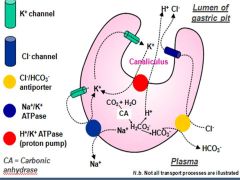
K+
|
|
|
which receptors are present on parietal cells- for what substrates (oxyntic mucosa- fundus & body)
|
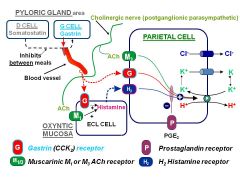
M3- Ach; G- gastrin/ somatostatin; H2- histamine; P- PGE2
|
|
|
what receptors are on ECL cells (oxyntic mucosa- fundus & body)
|
M1- Ach; G-gastrin
|
|
|
what produces PDE2 & what effect does it have
|
loacally by COX --> PGE2 receptor parietal cell--> INHIBITs acid ................powerful!
|
|
|
what does it mean by trafficking of H/K ATPase in parietal cells of oxyntic mucosa (fundus & body)
|
resting parietal cells:
- H/K ATPase largely within cell stimulated parietal cell: - H/K ATPase trafficks to apical membrane - extends microvilli |
|
|
what are the 3 phases of gastric secretion
|
1) cephalic
2) gastric 3) intestinal |
|
|
how is gastric secretion stimulated in the 1) CEPHALIC phase of gastric secretion
|

|
|
|
in the 2) GASTRIC phase of gastric secretions (instead of conditioned reflexes activating vagal stimulation in cephalic phase,) what sitmuli activate secretions?
where do they act to cause secretion |
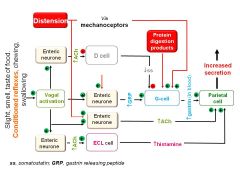
DISTENTION --> mechanoreceptors--> G cells
PROTEIN---> G cells |
|
|
what role does the 3) INTESTINAL phase have on gastric secretions
|
switch OFF secretions
stomach empties--> ↓G cell activation SOMATOSTATIN prod continues (low pH between meals- proteins act as buffer) |
|
|
what role does PROTEIN have on (pH &) gastric secretions
|
protein = buffer of stomach acid
↑gastric pH = turn off somatostatin (inhibitory) |
|
|
how do mucosal protecting mechanisms prevent against ulcers
|
hydrophobic monolayer repels H+
HCO3- in surface mucus gel layer high mucosal blood flow to clear H+ |
|
|
what role do NSAIDs have in predisposing to peptic ulcers
|
reduce PGE2 formation by INHIBITing COX
(PGE2 is powerful inhibitor of acid secretion) damage mucus layer & HCO3- prod |
|
|
how are peptic ulcers prevented in long-term NSAID use (e.g aspirin)
|
stable PGE1 analogue (e.g misoprostol)
acts like PGE2 to inhibit acid secretion maintains mucus & HCO3- |
|
|
what role does H.pylori have in causing ulcers
|
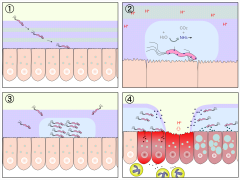
CHRONIC infection : lies in mucus layer
secretes inflammatory agents weaken mucosal barrier --> breakdown --> HCl & pepsin attack |
|
|
3 ways drug treatment aims to promote ulcer healing
|
- reduce acid
- promote mucosal resistance - eradicate H.pylori |
|
|
3 types of drugs used in treating peptic ulcers
|
PPIs
H2-antagonists muscarinic antagonists (M1 on ECL & M3 on parietal) |
|
|
how do PPIs work to reduce acid secretion in treating peptic ulcers
eg |
OMEPRAZOLE:
- covalently modifies ACTIVE H/K ATPase - irreversible - prodrug - active in acid |
|
|
how to H2-antagonists work in treating peptic ulcers
eg |
RANITIDINE:
- comp inhib H2 receptor on ECL cells (competes with Ach & gastrin) - ↓histamine - indirectly ↓H/K ATPase activity (acid prod) |
|
|
how do muscarinic antagonists work in treatment of peptic ulcers
eg NB: now obselete |
PIRENZEPINE:
- competes with ACh - blocks M1 = ↓histamine - blocks M3= ↓proton pump activation (H/K ATPase) |
|
|
what's SUCRALFATE & how does it act to strengthen mucosal barriers
administration |
mucosal strengthener (Al hydroxide & sulphated sucrose)
- acid-activated - Al- binds to ulcer base & gels with mucus - ↑mucosal blood flow ORAL |
|
|
how does bismuth chealate work in treating peptic ulcers
administration |
MUCOSAL STRENGTHENER:
- acid-activated - ↑mucosal blood flow - eradiates H.PYLORI (+ ranitidine) ORAL |
|
|
what are PPIs used to treat (e.g. omeprazole)
|
peptic ulcers
GORD 1st line Zollinger-Elison syndrome |
|
|
what's Zollinger-Ellison syndrome
|
acid HYPERSECRETION due to GASTRIN-producing tumour
|
|
|
what are H2-antagonists (ranitidine) used to treat
|
peptic ulcers
GORD |
|
|
what are antacids used for
|
symptomatic relief of peptic ulcers & dyspepsia
|
|
|
3 types of antacids and complexes they form in the stomach
|
MgOH --> MgCl
Mg trisilicate --> MgCl AlOH --> AlCl (causes diarrhoea) |
|
|
2 sets of PPI & abx combinations used in treatment of peptic ulcers
|
1) omeprazole + clarythromycin + amox
2) omeprazole + clarythromycin + metranidazole |
|
|
2 drugs used to increase gastric MOTILITY
clinical indications for: - GORD - disorders of gastric emptying |
DOMPERIDONE
METPROCLAMIDE |
|
|
what are the effects of domperidone
clinical uses |
↑gastric MOTILITY: ↑tone LOS, gastric emptying & peristalsis
GORD gastric emptying disorders |
|
|
what are the effects of metoproclamide
clinical uses |
↑gastric emptying
- GORD - disorders of gastric emptying |

