![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
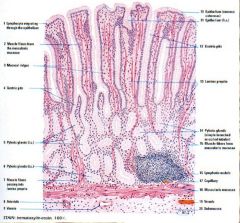
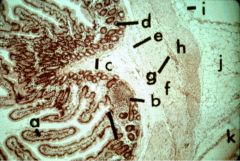
|
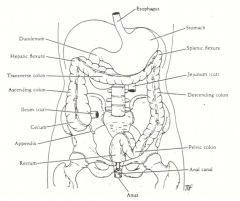
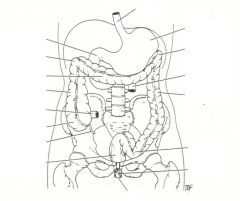
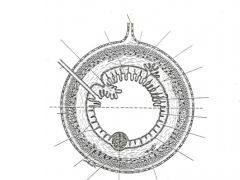
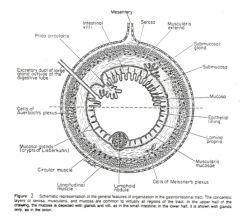
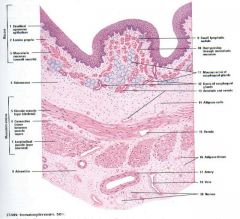
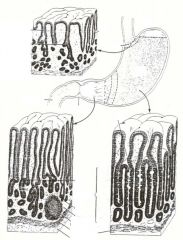
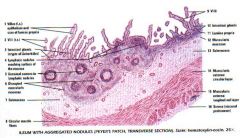
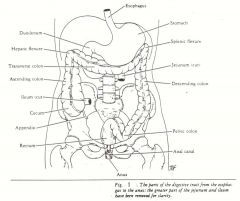
The gastrointestinal tract (GI) can be considered as a hollow tube extending from one end of the body to the other. The GI tract starts with the oral cavity (discussed in separate lecture) and continues with the esophagus, the stomach, the small intestine, and the large intestine (Figure 1). Although these organs have different functions, they have the same general histological plan (Figure 2). We will first review this general histological plan and then describe how these organs vary from one another.
|
|
|
|
|

|
|
|
|

|
|
|
|
|

|

|
|
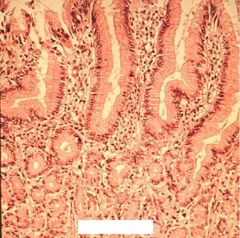
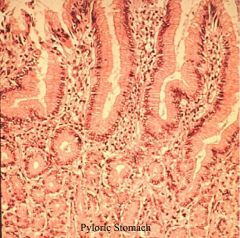
What are the anatomical regions of the stomach?
What are the folds inside the stomach called? |
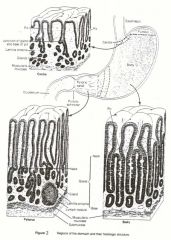
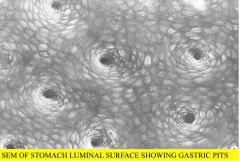
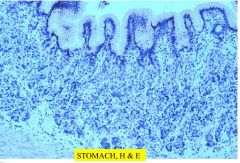
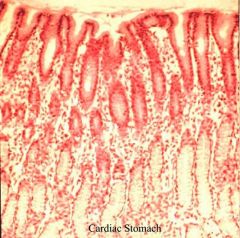
Anatomically, the stomach is divided into four regions: the cardiac portion, the fundus, the body, and the pyloric portion. If one were to cut into the stomach and observe the lining, it will appear grayish-pink. One would also see very large folds along the surface of the stomach that run in a longitudinal direction. These large folds, which involve both the lining mucosa and the submucosa, are known as Rugae.
|
|
|
|
|

|
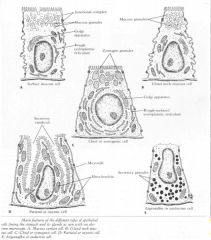
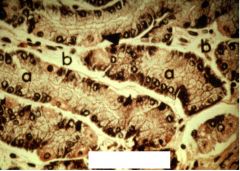
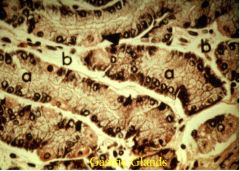
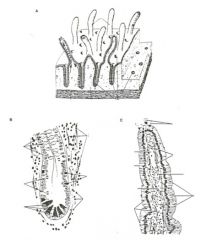
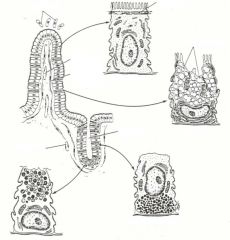
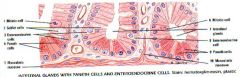
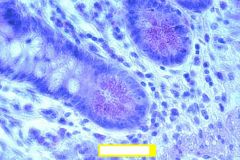
Main features of the different types of epithelial cells lining the stomach and its glands as seen with an electron microscope.
(A) Mucous surface cell. (B) Gland neck mucous cell. (C) Chief or zymogenic cell. (D) Parietal or axyntic cell. (E) Argentaffin or enteroendocrine cell. Diagram of a parietal cell, showing the main steps in the synthesis of hydrochloric acid. Blood CO2 under the action of carbonic anhydrase produces carbonic acid. This dissociates into a bicarbonate ion and a proton, H+, which reacts with the chloride ion to produce hydrochloric acid. The bicarbonate ion returns to the blood and is responsible for a measurable increase in blood pH during digestion. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

|
|
|

|
|
|

|
|
|
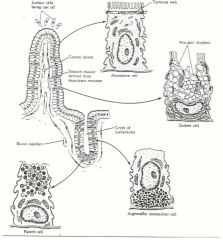
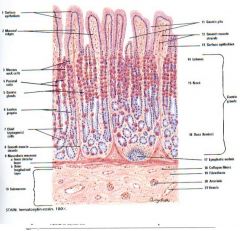
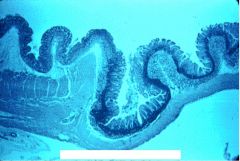
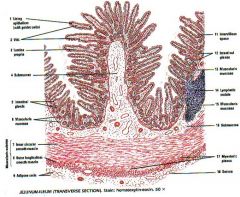
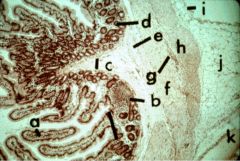
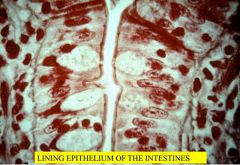
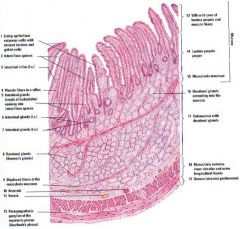
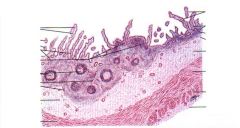
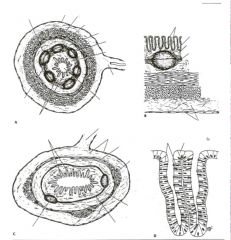
Fig. 7: Structure of a villus and a crypt of Lieberkühn; the electron microscopic structure of the surface epithelial cells is also shown.
|
|
|
|
|
|
|
|

|
|
|

|
|
|
|

|
|
|
|
|
|
|
|

|

|
|
|
|
|
|
|
|
|
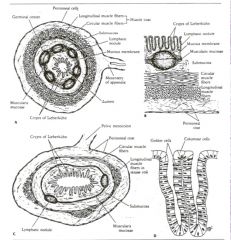
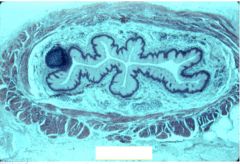
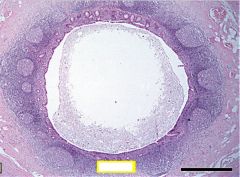
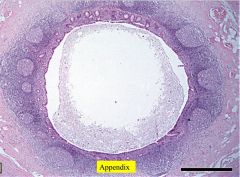
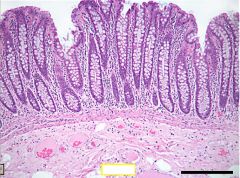
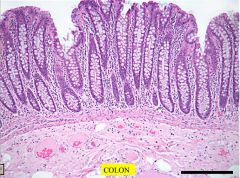
Fig. 8:
(A) General structure of the appendix as seen in cross section. (B) Enlarged view of the mucous membrane and submucosa of the appendix as seen in cross section. (C) General structure of the pelvic colon as seen in cross section. (D) Structure of two crypts of Lieberkühn of the colon. |
|
|

|
|
|
|
|
|
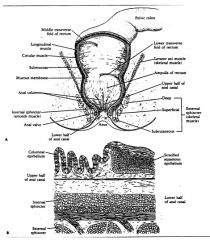
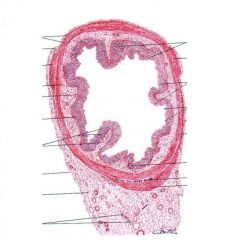
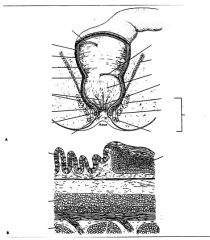
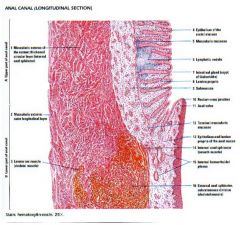
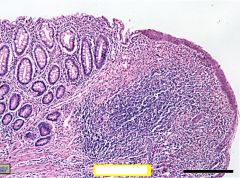
Fig. 9: (A) General structure of the rectum, anal canal, and sphincters of the anal canal. (B) Structure of the junction of the upper and lower halves of the anal canal as seen on longitudinal section.
|
|
|
|
|
|

|
|
|
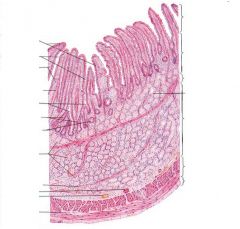
Mucosa
|
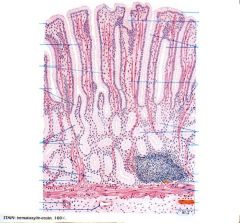
Mucosa: All the regions of the GI Tract possess a lining epithelium that lines the lumen of each region. This lining epithelium may be protective (esophagus), secretory (stomach), and/or absorptive (small intestine) in function. Under the lining epithelium is a region of connective tissue that is called the lamina propria (a general term given to any connective tissue under a lining epithelium). Under the lamina propria, there is a region of muscle called the muscularis mucosa. Together, these three regions - the lining epithelium, the lamina propria and the muscularis mucosa - make up the lining mucus membrane.
|
|
|
Submucosa
|
Submucosa: Under the muscularis mucosa is a region of connective tissue called the submucosa.
|
|
|
Muscularis externa
|
Muscularis externa: Outside of the submucosa is a thick layer of muscle. Usually, there is an inner layer of muscle that is circularly arranged and an outer layer of muscle that is longitudinally arranged. Together, these layers of muscle are known as the muscularis externa. The muscularis externa is responsible for the peristaltic waves that move the food through the length of the GI Tract.
|
|
|
Adventitia and serosa
|
Adventitia and Serosa: Outside any region of the GI Tract, one will find one of two things - Connective tissue that is continuous with connective tissue of the surrounding organs (adventitia). More commonly, however, a thin slippery membrane known as the serosa surrounds the GI Tract. The serosa consists of a single layer of squamous or cuboidal cells called the mesothelium under which there is a variable amount of connective tissue. The slippery serosa allows organs in the abdominal cavity to slide over one another without damaging each other. The serosa may be connected to the body wall by an extension termed the mesentery.
|
|
|
What are the nerves of the GI tract?
|
Nerves of the GI Tract: In addition to the above-mentioned layers, there are two prominent nerve plexuses along the length of the GI tract. The first, Meissner's Plexus, is located in the submucosa. The second, Auerbach's Plexus (also termed the Myenteric Plexus), is found between the layers of muscle making up the muscularis externa (i.e., between the inner circular and the outer longitudinal layers of the muscularis externa). Among other things, these nerve plexuses coordinate muscular contractions.
|
|
|
Give examples of some of the glands of the GI tract.
|
Glands of the GI Tract: There are glands outside of the GI Tract which send their ducts through the walls of the GI Tract and empty their content into the lumen. Two such ducts are the bile duct (bile from liver empties into the duodenum) and the pancreatic duct (from the pancreas into the duodenum). Also, glands may sometimes be found in the lamina propria or in the submucosa. Again, these glands empty their contents into the lumen of the GI Tract.
|
|
|
Describe the modifications of the lining mucosa. How is this helpful?
|
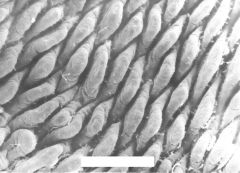
Modifications of the Lining Mucosa: The lining epithelium may have modifications to increase the luminal surface area. These may be large folds that involve both the lining mucosa and submucosa (e.g., plicae, rugae) or, smaller projections extending into the lumen (e.g., intestinal villi).
|
|
|
How long is the esophagus?
How fast is food propelled? How is it propelled? What lines the esophagus? What are the layers of the esophageal tube? |
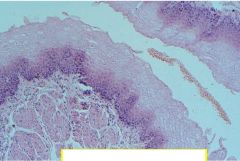
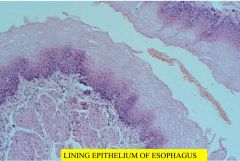
A. The esophagus is a tube (approximately 25 cm long) running from the pharynx to the stomach. Food is propelled along the esophagus (at a rate of about 5 cm/sec) by voluntary muscular action in the oral cavity followed by involuntary waves of muscle contraction (i.e., peristalsis) in the walls of the esophagus.
B. The esophagus is lined by a protective, non-keratinized stratified squamous epithelium that protects the esophagus from abrasive damage. Under the non-keratinized squamous epithelium one finds the lamina propria. Under the lamina propria are the muscularis mucosa, the submucosa, and the muscularis externa. Most of the esophagus is surrounded by an adventitia. |
|
|
Are the layers of the esophagus the same for the entire length ?
|
The upper third of the esophagus:
The muscularis externa is unique in the esophagus. In the upper third of the esophagus, the muscularis externa is composed of skeletal muscle rather than smooth muscle. However, this skeletal muscle is not under voluntary control. The middle third of the esophagus: There is a transition from skeletal to smooth muscle in the middle third of the esophagus (i.e., one will find both smooth and skeletal muscle in this region). The lower third of the esophagus: The muscularis externa is composed exclusively of smooth muscle. The smooth muscle will continue throughout most of the rest of the GI Tract. |
|
|
What types of glands are found in the esophagus?Where are they found? What do they do?
|
Glands of the Esophagus:
There are two types of glands in the esophagus. 1. The first type, termed the Submucosal Glands, is found in the submucosa throughout the length of the esophagus. These glands lubricate the esophagus by secreting a protective mucin. 2. The second populations of glands of the esophagus are called Cardiac Glands. These are located in the lamina propria of the lining mucosa at two different sites: at the junction of the esophagus and the stomach (these glands are similar to glands found in the cardiac portion of the stomach, hence, the name) and between the cricoid cartilage and the fifth tracheal ring. The cardiac glands also secrete a protective mucin. |
|
|
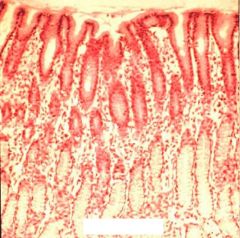
What happens when food enters the stomach?
How long does it stay in the stomach? What is absorbed in the stomach? |
When food enters the stomach, it is churned and mixed with the digestive enzymes and after 3-4 hours it is transformed into a semi-fluid known as chyme. Very little absorption occurs in the stomach; some water, alcohol and drugs are absorbed in the stomach, but mainly the function of the stomach is digestion (breaking down of the food products).
|

