![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
Antimuscarinics - members
|
Inhibits Parasympathetic And Sweat: Ipratropium Pirenzepine, Atropine, Scopolamine
|
|
|
Direct sympathomimetic catecholamines
|
DINED: Dopamine, Isoproterenol, Norepinephrine, Epinephrine, Dobutamine
|
|
|
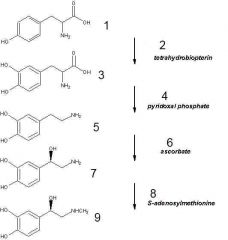
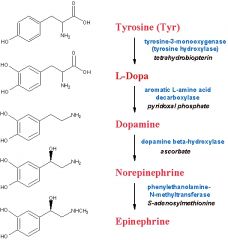
The rate-limiting step in the synthesis of norepinephrine is?
|
The formation of 3,4-dihydroxyphenylalanine (DOPA) by tyrosine beta-hydroxylase
(Stringer) |
|
|
The major pathway for termination of the action of NE is?
|
Reuptake.
(Stringer) |
|
|
What type of receptor does the acetylcholine from the preganglionic autonomous neurons bind to?
|
Nicotinic.
(Stringer) |
|
|
Does the parasympathetic or the sympathetic nervous system have short postganglionic fibers?
|
The parasympathetic system.
(Stringer) |
|
|
What is the neurotransmitter of postganglionic sympathetic neurons?
|
Mostly NE, two exceptions
1. Ach is found in sweat glands 2. 80% of adrenal medulla secretions is Epinephrine (Stringer) |
|
|
Structure of a basic catecholamine - draw dopamine
|
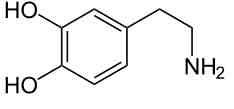
Basically a benzene ring with two hydroxyl groups (3,4), ethyl, and an amine group
(Catechol is the benzene group with two hydroxyl groups situated next to each other) (Stringer\Wikipedia) |
|
|
Degradation of catecholamines
|
1. Mostly by reuptake by presynaptic neuron
2. Enzymatically - in the liver and a little in the brain a. COMT (catechol-O-methyl-transferase) (Plays a major role in the metabolism of endogenous and exogenous circulating EPI and NE) b. MAO (monoamine oxidase) A, B (Stringer) |
|
|
|
|
|
Five main subtypes of receptors for norepinephrine
|
Alpha -
1 2 Beta - 1 (mainly heart) 2 (skeletal muscle vessels, bronchial smooth muscle) 3 (adipose tissue) (Stringer) |
|
|
Activation of alpha-adrenergic receptors cause (4)
|
1. Vasoconstriction (ie GI tract)
2. Contract radial muscle of eye -> dilation\mydriasis 3. Contracts sphincters in various places 4. Mediate ejaculation (Stringer) |
|
|
Which adrenergic receptor subtype cause renin release?
|
Beta1
(Stringer) |
|
|
Alpha2-adrenergic receptors
a. Function and location b. Effect of blocking c. Example of antagonist |
a. Activation of presynaptic alpha2 receptors results in feedback inhibition of the release of NE, thus decreases the release of NE
b. Inhibition of presynaptic alpha2 receptors will increase the release of NE c. Clonidine (Stringer) |
|
|
Organization of cholinomimetics
a. Direct-acting - mechanism, which receptors do they work in? b. Indirect-acting - mechanism, which receptors do they work on? |
a. Have a direct action on the nicotinic or muscarinic receptor for acetylcholine
b. The indirect-acting cholinomimetics act by inhibiting acetylcholinesterase. Work at all cholinergic synapses. (Stringer) |
|
|
Direct cholinergic agonists
a. Esters - structure, metabolized by cholinesterase, examples (4)? b. Alkaloids - structure, metabolized by cholinesterase, examples (4)? c. Most effect on the muscarinic or the nicotinic receptors? d. Which is used to treat urinary retention e. Which is used therapeutically to help patients stop smoking? f. Side effects - related to nicotinic or muscarinic receptors - examples (4) |
a. Esters of choline, metabolized by acetylcholinesterase (similar to Ach)
1. Bethanechol 2. Carbachol 3. Cevimeline 4. Methacholine b. Alkaloids - alkaloids that are not related to acetylcholine and are generally plant derived, since their not strucurally related to Ach, they're not metabolized by cholinesterases 1. Arecoline 2. Muscarine 3. Pilocarpine 4. Nicotine c. Almost exclusively on muscarinic in the therapeutic doses d. Bethanechol (Postoperative period, patients with neurogenic bladder (dysfunction of micturition due to CNS or PNS pathology) e. Nicotine f. Muscarinic Increased sweating (increased secretion), salivation, GI distress, cramps (increased motility) (Stringer) |
|
|
Cholinesterase inhibitors
a. Groups b. Which are not used therapeutically? c. Which are lipid soluble? d. To which group does the carbamates and quatarnary amines belong? e. To which group does the organophosphates belong? |
Reversible inhibitors (water-soluble) (quaternary amines, carbamates)
Irreversible inhibitors (organophosphates, lipid soluble, not used therapeutically) (Stringer) |
|
|
Reversible cholinesterase inhibitors (carbamates and quaternary amines)
a. Endings b. Mechanism c. Drugs used for Myasthenia gravis (6) d. Drugs used for Alzheimer's disease? |
a. Many end in -stigmine and -nium.
b. Competitive inhibitor c. Myasthenia gravis 1. Edrophonium 2. Neostigmine 3. Pyridostigmine 4. Ambenonium 5. Demecarium 6. Physostigmine d. Alzheimer's disease 1. Donepezil 2. Galantamine 3. Rivastigmine 4. Tacrine (Stringer) |
|
|
Irreversible cholinesterase inhibitors
a. Synonym b. Mechanism c. Uses (2) d. Examples (7) e. Side effects |
a. Organophosphates
b. Inhibit the enzyme by phosphorylating it. c. Insecticides, "nerve gases" (Since they are lipid-soluble they rapidly cross all membranes - including skin and BBB) d. (-phate, -thion) 1. Diisopropyl fluorophosphate 2. Echothiophate 3. Isoflurophate 4. Malathion 5. Parathion 6. Sarin (Released by a terrorist group into three different subway lines in Tokyo in 1995, injuring more than 5500 people) 7. Soman e. Muscarinic effects (salivation, sweating, cramping, GI distress) and nicotinic effects -> fasciculations, CNS effects: tremor, anxiety, coma (Stringer) |
|
|
Reversible cholinesterase inhibitors
a. Which is used in the diagnosis of myasthenia gravis? b. Which are used in the treatment of myasthenia gravis (3)? c. Which are used in the treatment of Alzheimer's disease? d. Other therapeutic uses (2) |
a. Edrophonium
(Short-acting, administered IV, if they have myasthenia gravis, the drug will dramatically improve muscle strength) b. Neostigmine, pyridostigmine, and ambenonium (Longer-acting) c. 1. Donepezil 2. Galantamine 3. Rivastigmine 4. Tacrine (Studies have shown a deficiency of cholinergic neurons in patients with Alzheimer's disease.) (These agents are preferred due to their higher efficacy in the brain than in the periphery) d. Treatment of open-angle glaucoma, reversal of non-depolarizing neuromuscular blockade after surgery (Stringer) |
|
|
Irreversible cholinesterases\Organophosphates
a. Which agents are used to treat poisoning of irreversible cholinesterases\organophosphates (2) b. Mechanism |
a. Pralidoxime and atropine
b. Pralidoxime phosphorylate the phosphate added by the organophosphate to the cholinesterase (Works if the enzyme-phosphate complex has not aged, don't cross BBB <- can't relieve CNS symptoms) Atropine is a cholinergic antagonist (stringer) |
|
|
Muscarinic antagonists
a. Mechanism of action b. Members (7) c. Which are used to prevent motion sickness? d. Which are used in the treatment of COPD? e. Which are used for urinary frequency, urgency, and urge incontinence caused by detrusor overactivity? |
a. Competitive antagonists to the muscarinic receptor
b. 1. Atropine 2. Ipratropium 3. Scopolamine 4. Tiotropium 5. Tolterodine 6. Trospium 7. Oxybutinin c. Scopolamine (CNS-mediated effected, by transdermal patch) d. Ipratropium, tiotropium (To choice of whether to use a beta-agonist or muscarinic antagonist depend mostly on the side effect profile) e. Tolterodine, Trospium, Oxybutynin (Stringer) |
|
|
Effects and side effects of muscarinic antagonists
a. Eye (3) b. Skin (2) c. GI (2) d. CVS (1) e. Respiratory (2) f. Genitourinary (1) g. CNS (3) |
a. Mydriasis, Cycloplegia (blurred vision from loss of power of ciliary muscle), dry eyes
b. Flushing, reduced sweating c. Reduced motility (constipation) and secretions d. Increased heart rate (at high doses) e. Bronchial dilation and decreased secretion f. Urinary retention g. Drowsiness, hallucinations, coma (Stringer) |
|
|
Muscarinic antagonists - use (7)
|
1. Preoperatively to reduce secretions
2. To prevent motion sickness (Scopolamine) 3. To treat COPD (Ipratropium) 4. To inhibit detrusor overactivity causing urinary frequency, urgency and urge incontinence (Tolterodine, Trospium, Oxybutynin) 5. To produce mydriasis for eye surgery 6. For Parkinson's 7. Adjuncts to treatment of irritable bowel syndrome (Stringer) |
|
|
Neuromuscular blockers
a. Mechanism b. Can the effect be inhibited? c. Which drug is often given concurrently? d. Use |
a. Relatively selective antagonists to nicotinic receptor. Depolarizing blockers open ion channel while nondepolarizing don't
b. Yes, by administration of cholinesterase inhibitor c. Muscarinic antagonist d. To produce skeletal muscle relaxation. (Stringer) |
|
|
Neuromuscular blockers
a. Members of depolarizing blockers b. Most members of nondepolarizing neuromuscular blockers contains which letters c. Members of nondepolarizing neuromuscular blockers (5) |
a. Succinylcholine
(Brief action) b. -cur- c. 1. d-Tubocurarine 2. Pancuronium 3. Vecuronium 4. Atracurium 5. Rocuronium |
|
|
Succinylcholine
a. Properties b. Severe associated side-effect c. Treatment of this side-effect |
a. Rapid acting, depolarize the junction
b. Malignant hyperthermia c. Dantrolene (Interfere with release of Ca from the sarcoplasmic reticulum) (Stringer) |
|
|
Adrenergic agonists - distinction into direct- and indirect-acting
|
The indirect-acting do not bind to specific receptors (not specific action), but act by releasing stored NE
The direct-acting on the other hand bind to receptors, so specificity is possible. (Stringer) |
|
|
Significance of differentiation of adrenergic agonists into catecholamines and non-catecholamines
|
Only the catecholamines are metabolized by catechol-O-methyl-transferase (COMT) and monoamine oxidase (MAO).
(Catecholamines: epinephrine, norepinephrine, dopamine) (Non-catecholamines: albuterol, bitolterol, ephedrine, formoterol, isoetharine hydrochloride, isoproterenol, levalbuterol, metaproterenol, pirbuterol, salmeterol, and terbutaline) (Stringer) |
|
|
Adrenergic agonists
a. What are the only two direct-acting agonists that activate both alpha and beta receptors? b. alpha-1 agonist members (2) c. alpha-1 agonist use (2) |
a.
1. Epinephrine (Almost equal effect on alpha and beta, and on beta1 and beta2) 2. Norepinephrine (Lower affinity for beta2) b. Phenylephrine, midodrine c. 1. Nasal decongestant (decrease blood flow and decrease secretions) (phenylephrine) 2. Increase blood pressure (midodrine) (Stringer) |
|
|
Alpha-2 adrenergic agonists
a. Member (1) b. Mechanism (2) c. Use |
a. Clonidine
b. 1. Activate alpha-2 receptors in CNS -> decrease sympathetic stimulation (ie heart) 2. Activate presynaptic alpha-2 receptors on peripheral nerve endings -> inhibit release of NE c. Antihypertensive (Stringer) |
|
|
Beta-adrenergic agonists
a. Mostly beta-1-agonist b. Mixed c. Mostly beta-2-agonist |
a. Dobutamine
(Increase heart rate and cardiac output) b. Isoproterenol c. 1. Albuterol 2. Terbutaline 3. Metaproterenol (Stringer) |
|
|
Dopamine
a. Structure b. Effect |
a. Catecholamine
(Precursor to norepinephrine) b. 1. High doses - much like epinephrine 2. Lower doses - cause renal and coronary vasodilation while alsovating activating beta-1-receptors in the heart (increase CO) (Thus increase CO in treatment of shock while preserving renal blood flow) (Dopamine receptors are located throughout the body and in the CNS) (Stringer) |
|
|
Indirect-acting sympathomimetics
a. Mechanism b. Members (5) |
a. Act by releasing previously stored norepinephrine and is thus non-selective.
b. 1. Ephedrine, phenylpropanolamine -> nasal decongestants 2. Amphetamine, dexmethylphenidate, methylpenidate -> CNS stimulants used to treat ADHD and narcolepsy (Modafinil is now used to treat narcolepsy, uncertain mechanism) (Stringer) |
|
|
Norepinephrine - effect on
a. Heart rate and cardiac b. Mean arterial pressure c. Peripheral resistance |
a. Decreased
(Reflex via parasympathetic activation due to increased mean arterial pressure) b. Increased (alpha-adrenergic-mediated vasoconstriction) c. Increased (Alpha-adrenergic stimulation) (Stringer) |
|
|
Epinephrine - effect on
a. Heart rate and cardiac output b. Peripheral resistance c. Mean arterial pressure |
a. Increased
(Beta-1) b. Low doses - decrease (beta-2), middle - no change (alpha-beta equilibrium), high - increase (alpha) c. Same as peripheral resistance (Stringer) |
|
|
Isoproterenol - effect on
a. Heart rate and cardiac output b. Peripheral resistance |
a. Increased
(Mixed beta agonist) b. Decreased (Stringer) |
|
|
Central sympathetic blockers
a. Mechanism b. Members (4) |
a. Alpha-2-agonists. Alpha-2 receptor activation inhibits both sympathetic output from the brain and release of norepinephrine from nerve terminals.
b. 1. Clonidine, guanabenz, guanfacine -> antihypertensives 2. Tizanidine -> antispastic agent (Stringer) |
|
|
Alpha-adrenergic antagonists
a. Members (7) b. Side-effects c. Name of alpha-1A antagonist that is used to treat benign prostatic hypertrophy |
a.
1. Alpha-1 selective: prazosin, terazosin, doxazosin, trimazosin, phenoxybenzamine (only irreversible inhibitor) -> all -azosin are used as antihypertensives 2. Mixed alpha-1 and alpha-2: phentolamine, tolalozine (3. alpha-2: yohimbine. No therapeutic use) b. 1. Postural hypotension (Sympathetic activity is greater when a person is standing) 2. Reflex tachycardia c. Tamsulosin (Alpha-1A is specific to genitourinary tract - constrict the smooth muscle in the bladder neck and prostate) (Stringer) |
|
|
Beta-adrenergic antagonists
a. Nonselective beta antagonists (5) b. Selective (Cardioselective) beta antagonists (5) c. Beta-antagonists should be used with caution in patients with which condition c. |
a.
1. Propranolol 2. Carteolol 3. Levobunol 4. Timolol 5. Pindolol b. 1. Acebutolol 2. Atenolol 3. Metoprolol 4. Esmolol 5. Bisoprolol c. Diabetes (Metabolic effects of symapthetic stimulation (glycogenolysis, gluconeogenesis, lipolysis) are mediated by beta receptors. Thus in response to hypoglycemia, the sympathetic nervous system can't respond. The reflex tachycardia in response to hypoglycemia which is an early warning sign to the diabetic patient is also removed) (Some beta antagonists have partial agonist activity) (Stringer) |
|
|
Mixed alpha and beta adrenergic antagonists
a. Members (2) b. Relative effect on the different subreceptors |
a.
1. Labetalol 2. Carvedilol (Both don't end in the usual -olol) b. Both are nonselective at the beta receptor and specific for the alpha-1 receptor (Stringer) |

