![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
64 Cards in this Set
- Front
- Back
|
What is Pharmacology |
The study of drugs: Pharmacology is not to be confused with Pharmacy which concerns It's d |
|
|
Pharmacodynamics |
what drugs do to the body D + R ⇒ DR Biological Effect is proportionate to the amount of DR |
|
|
Pharmacokinetics |
what the body does to drugs |
|
|
What is a Receptor? |
The beneficial therapeutic effects and many of the unwanted |
|
|
How do drugs work? |
Drugs elicit their desirable and many of their undesirable effects by mimicking or blocking the actions of hormones and neurotransmitters! |
|
|
What are ligands? |
Ligands include drugs as well as endogenous signaling molecules such as hormones and neurotransmitters!
|
|
|
How do ligands work? |
Upon recognition and binding an appropriate molecule (ligand), receptor proteins transmit this chemical signal into a biological change in the target cell! |
|
|
Major Classes of Receptors |
• Ligand-Gated Ion Channels • Ligand-Activated Transcription Factors |
|
|
What do the different pathways for receptors look like? |
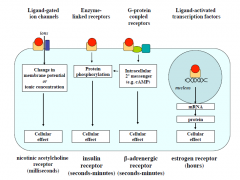
|
|
|
The Lock and Key Model of Ligand-Receptor Interaction |
Normal hormone = key in lock Agonists are like bobby pins that pick locks Antagonists bind to receptors but do not produce a response
|
|
|
Chemistry of Drug-Receptor Interactions |
Most drug-receptor interactions - strong chemical bonds (covalent) - difficult reversal of effects/toxicity |
|
|
Relationship of Drug Concentration and Receptor Binding |
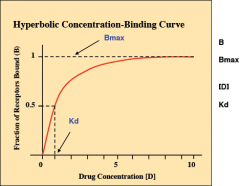
|
|
|
Relationship of Drug Concentration and Receptor Binding |
B = Bmax × [D]/ |
|
|
Sigmoidal Receptor Binding Curves |
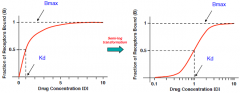
- Semi-logarithmic transformation - Common representation of pharmacological data |
|
|
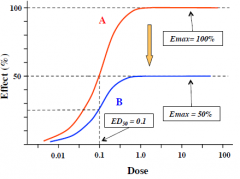
Graded-dose dependent curves |
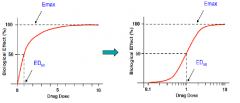
Emax -the maximum response achieved by an agonist |
|
|
Affinity |
ability of the ligand to bind to the receptor |
|
|
Efficacy |
|
|
|
Potency |
where 50% of the maximum response is achieved |
|
|
Quantal Dose-Response Curves |
Graded Phenomena: - infinite number of intermediate states - vessel dilation, blood pressure change, heart rate change! Quantal Phenomena: - “all-or-none” - death, pregnancy, cure, pain relief, effect of given magnitude -ex. you can't be "sort of" pregnant |
|
|
Quantal Dose-Response Curves |
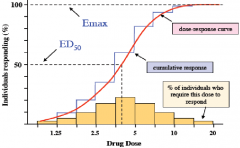
Quantal Dose-Response Curves |
|
|
Potency |
• related to the amount of drug needed -if something is more potent, |
|
|
Efficacy |
Efficacy • the maximum effect that can be |
|
|
Potency v.s. Efficacy |
On the graph, more potency = not a delayed curve and more efficacy = a taller response |
|
|
Agonist Types: Its All Relative |
A: full agonist (“gold standard”) B: partial agonist C: full agonist D: partial agonist reduced potency, reduced efficacy
|
|
|
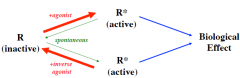
A Model for Constitutive Receptor Activation! |
|
|
|
A Model for Constitutive Receptor Activation |
• agonist (e.g. drug, hormone, neurotransmitter) binding induces a conformational change in the receptor from the inactive (R) to active (R*) state |
|
|
Inverse Agonists |
get rid of the normal affect instead of bringing in a new effect
|
|
|
An Experimental Apparatus to Measure Constitutive Receptor Activity |
• Isolated blood vessel preparation Add agonist • Agonist dilates blood vessel |
|
|
Effect of inverse agonist |
-has an independent impact upon -Inverse agonists reveal constitutive receptor activity |
|
|
Chemical Antagonism |
- Direct interaction of two drugs in solution such that the effect of one or -e.g. protamine (acidic anticoagulant) and heparin (basic |
|
|
Physiological Antagonism |
- Indirect interaction of two drugs with opposing physiological actions |
|
|
Pharmacological Antagonism |
- Blockage of interaction of one drug with receptor by another drug! |
|
|
Types of pharmacological antagonists |
Competitive and Non-Competitive Antagonists |
|
|
Competitive Antagonists |
-bind reversibly to the receptor |
|
|
Non-Competitive Antagonists |
-bind irreversibly (e.g. covalently) to the receptor or to a site on the -primarily affect efficacy |
|
|
How does competitive antagonism work? |
Effect = 100% when both receptors (blue) are bound by agonist (green), the maximum Effect = 50% when a competitive antagonist (red) is present, it can displace the agonist from the receptor and the biological effect is reduced Effect = 100% increasing the amount of agonist can displace the competitive antagonist and |
|
|
Competitive Antagonists - Effect on Dose Response Curves |
A: -agonist with NO antagonist -agonist has maximum B: -agonist with competitive |
|
|
Non-Competitive Antagonism |
Effect = 100% when both receptors (blue) are bound by agonist (green), the maximum Effect = 50%! when a non-competitive Effect = 50% Increasing the amount of agonist cannot displace the non-competitive antagonist |
|
|
Non-Competitive Antagonists - Effect on Dose Response Curves |
A: • agonist with NO antagonist B: • agonist with non-competitive |
|
|
Drug Desensitization |
• effect of a drug often diminishes when given |
|
|
Receptor Mediated Drug Desensitization |
- loss of receptor function |
|
|
Non-Receptor Mediated Drug Desensitization |
- reduction of receptor-coupled signaling components |
|
|
Simplified Model for Desensitization of G Protein-Coupled Receptor (GPCR) Signaling |

Receptor Mediated Non-Receptor Mediated |
|
|
Non-Receptor Mediated Desensitization: Reduction of Receptor-Coupled Signaling Components |
-depletion of signaling molecules required for biological response |
|
|
Non-Receptor Mediated Desensitization: Increased Metabolic Degradation |
-increase in the rate of metabolism and/or elimination of drug |
|
|
Non-Receptor Mediated Desensitization: Physiological Adaptation |
-reduction or amelioration of drug effects due to opposing homeostatic response |
|
|
Adverse drug effects: Side effect |
• Dose-dependent |
|
|
Adverse drug effects: Toxic reaction |
• Dose-dependent |
|
|
Adverse Reaction: Allergic Reaction |
• Not dose-dependent |
|
|
Example: Beneficial versus Adverse Effects of Cyclosporine: Desirable Beneficial Therapeutic Effect |
– Promotes survival of transplanted organs |
|
|
Example: Beneficial versus Adverse Effects of Cyclosporine: Adverse effects |
– Increased susceptibility to infection and increased risk for some cancers • Magnitude of effect is dose-dependent |
|
|
Therapeutic Index |
• A measure of drug safety Therapeutic Index (T.I.) = • In general, a larger T.I. indicates a clinically safer drug |
|
|
Therapeutic Window – Relationship to Blood Levels |
A measure of drug safety that considers the range of blood concentrations of a drug that are A larger therapeutic window makes a safer drug. |
|
|
Pharmacokinetic Differences are a Major |
Same drug, same diagnosis, same dose can have different effects for the different people because their bodies may respond to drugs differently. |
|
|
Pharmacokinetics |
Drug absorption, administration, metabolism and excretion etc |
|
|
Pharmacodynamics |
Clinical response, adverse effect, therapeutic benefit |
|
|
Enteral drug administration |
-desired effect is systemic(non-local), substance is given via the digestive tract Oral is the most convenient route, but not ideal if the drug has a quick first pass metabolism as the bioavailability can be reduced Other methods include gastric feeding tube and rectal |
|
|
Parenteral drug administration |
desired effect is systemic (non-local), drug is given by route other than digestive tract This method has 100% bioavailability Bypass first pass effect But may be more expensive and require professional assistance • Transdermal (nicotine patches) |
|
|
Topic Drug Administration |
local effect, substance is applied directly where its action is desired |
|
|
Oral Drug Absorption |
• The process by which a drug moves from the |
|
|
Physiochemical Factors that Affect Oral Drug Absorption |
– Concentration difference across membrane – Size – Polarity! Ionization • Dependent upon environmental pH |
|
|
Passive Drug Absorption in the Small Intestine |
• The majority of absorption for |
|
|
Physiological Factors That Affect Oral Drug Absorption |
1) Gastrointestinal Motility – Many drugs are metabolized by enzymes in enterocytes |
|
|
First pass effect |
The first-pass effect (also known as first-pass metabolism or presystemic metabolism) is a phenomenon of drug metabolism whereby the concentration of a drug is greatly reduced before it reaches the systemic circulation. It is the fraction of lost drug during the process of absorption which is generally related to the liver and gut wall. Notable drugs that experience a significant first-pass effect are imipramine, morphine, propranolol, buprenorphine, diazepam, midazolam, demerol, cimetidine, and lidocaine. |

