![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
2 Herbicides that when ingested in high doses can produce signs of Neuromuscular involvement
|
2,4-dichlorophenoxyacetic acid (2,4-D) & 2,4,5-trichlorophenoxyacetic acid (2,4,5-T)
|
|
|
Chlorphenoxy Herbicides are often contaminated with what? What effects may it have on humans?
|
TCDD = Agent Orange
Large amounts for long periods of time = Reproductive & Carcinogenic effects Chloracne = almost always |
|
|
What 2 Herbicides uncouple oxidative phosphorylation & thus increase the Metabolic Rate & temperature? What is the treatment?
|
Dinitrophenols + Pentachlorophenol
Cool the patient down |
|
|
This Herbicide under goes redox cycling & causes free radical mediated injury to lungs
|
Paraquat
|
|
|
What is Paraquat's mechanism of action in causing Lung damage?
|
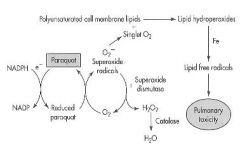
1. Reduced by NADPH
2. Reduced Paraquat reacts with molecular Oxygen to produce Superoxide radicals 3. Superoxide radicals form Singlet Oxygen 4. Singlet oxygen reacts with Polyunsaturated cell membrane lipids to produce Lipid Peroxides 5. Lipid free radical = Pulmonary Toxicity |
|
|
How does one die from ingesting Paraquat orally? Inhalation?
|
Orally = liver, kidney -> Lung (fatal)
Inhalation = Lung (fatal) -faster |
|
|
List the Halogenated Hydrocarbons
What are they most often used as? |
Carbon Tetrachloride
Chloroform Methylene Chloride Chloroethylene Trichloroethylene Tetrachlorethylene Solvents for cleaning |
|
|
What is the mechanism of toxicity for Carbon Tetrachloride?
|
Hepatotoxicity
1. metabolized by a P450 to Trichlormethyl free radical (*CCl3) 2. free radical-induced lipid peroxidation causes an increase in Intracellular Ca++ leading to cell death |
|
|
What are the symptoms of Halogenated Hydrocarbon (-chlor-) poisoning? (4)
|
1. CNS depressants
2. Cardiac arrhythmias at high doses by sensitizing myocardium to catecholamine stimulation 3. Liver & Kidney damage 4. Carcinogenicity |
|
|
What is the treatment for Halogenated Hydrocarbon toxicity?
|
Remove contaminated clothing to stop further absorption
Treat symptoms & support vital signs |
|
|
What do all Alcohols & Glycols cause at high doses?
|
CNS depression
|
|
|
What alcohol is Neurotoxic?
|
Methanol
|
|
|
What are the properties of Isopropyl Alcohol (rubbing alcohol)?
|
1. CNS depression
2. Metabolized to Acetone 3. Renal damage 4. Gastric lavage 5. treat symptoms |
|
|
What alcohol/glycol is Nephrotoxic?
|
Ethylene glycol & diethylene glycol
|
|
|
What Alcohol/glycol is used as a vehicle for drugs?
|
Propylene glycol
|
|
|
Describe the metabolism of Ethanol
|
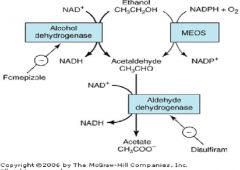
Ethanol -1-> Acetaldehyde -2-> Acetate
1. Alcohol Dehydrogenase 2. Aldehyde Dehydrogenase |
|
|
What drug inhibits Alcohol Dehydrogenase & is used to treat Ethanol & Ethylene Glycol poisoning?
|
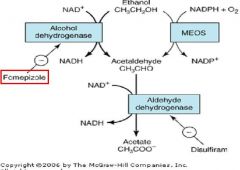
Fomepizole
|
|
|
What drugs may cause a Disulfarim effect? (4)
|
1. 3rd generation Cephalosporins
-Cefemandole -Cefoperazone 2. Metronidazole 3. Trimethoprim 4. Chlorpropamide |
|
|
What are the CNS effects of Ethanol due to?
|
Stimulation due to inhibition of CNS inhibitory GABA pathways = Disinhibition
Followed by anesthetic-like CNS depression at higher doses = visual impairment, muscular incoordination, slowing of reaction time, euphoria, respiratory depression & coma |
|
|
What is Ethanol's effect on the kidney?
|
Diuresis by Vasopressin (ADH) inhibition & temporary positive fluid balance
|
|
|
What would be a reason for telling old people to drink a glass of wine (ethanol) before meals?
|
causes increased SALIVATION & GASTRIC SECRETION to stimulate appetite
|
|
|
Why does Ethanol predispose to Hypothermia in cold environments?
|
causes Peripheral vasodilation which results in warm, flushed skin, interfering with normal homeostatic mechanisms responsible for maintaining constant core body temperature
|
|
|
What are the blood alcohol levels of Acute Mild, Moderate, Severe, & Coma poisoning? What symptoms accompany each?
|
Mild = 50-150 mg% = decreased inhibitions; visual impairment; muscular incoordination; slowing of reaction time
Moderate = 150-300 mg% = major visual impairment; symptoms of mild intoxication are more pronounced; slurring of speech Severe = 300-500 mg& = approaching stupor; severe hypoglycemia; convulsions; fatalities Coma = 500 mg% = slowed respiration; complete loss of sensations; deaths are frequent at this blood level |
|
|
What is the treatment strategy for Acute Ethanol poisoning?
|
1. Support vital signs
2. avoid depressant drugs 3. Hemodialysis if blood levels are greater than 500 mg% |
|
|
What are the treatments for Chronic Ethanol poisoning?
|
Diazepam IV = for seizures associated with withdrawal
Chlordiazepoxide = to prevent withdrawal during treatment program |
|
|
What is Disulfiram's mechanism of action?
|
inhibits Acetaldehyde Dehydrogenase causing accumulation of Acetaldehyde in blood resulting in nausea & vomiting
|
|
|
Oral Opioid Antagonist that has shown some promise in treating alcohol addiction
|
Naltrexone
|
|
|
What does acute toxicity from Methanol result from?
|
its rapid metabolic conversion to Formaldehyde & Formic Acid
|
|
|
Describe the metabolism of MEthanol
|
Methanol -1-> Formaldehyde -2-> Formic Acid -3-> Formate
1. Alcohol Dehydrogenase 2. Acetaldehyde Dehydrogenase 3. pH dependent |
|
|
What are the symptoms of Methanol poisoning?
|
1. Visual disturbances -> BLINDNESS
2. CNS toxicity 3. Metabolic Acidosis 4. Death is usually due to Acidosis & Respiratory failure |
|
|
What is the treatment for Methanol poisoning?
|
1. Emesis or Gastric Lavage
2. Antidote = 50% Ethanol IV = competes for Alcohol Dehydrogenase -or Fomepizole = synthetic Alcohol Dehydrogenase inhibitor 3. Treat acidosis with Sodium Bicarbonate |
|
|
What are the symptoms of Ethylene Glycol & Diethylene Glycol poisoning?
|
1. CNS depression
2. KIDNEY DAMAGE DUE TO CALCIUM OXALATE CRYSTALS |
|
|
What poisoning causes Kidney damage due to Calcium Oxalate Crystals?
|
Ethylene Glycol
|
|
|
What is the treatment for Ethylene Glycol & Diethylene Glycol poisoning?
|
1. Gastric lavage
2. Ethanol IV = Antidote = prevents conversion of Glycols -> Oxalic Acid by competing for Alcohol Dehydrogenase -or Fomepizole 3. treat symptoms & support vital signs |
|
|
List some Petroleum distillates
|
1. Kerosene
2. Diesel fuel 3. Gasoline 4. White spirit 5. Polishes & other household products |
|
|
What are the symptoms of Petroleum distillates (gasoline, kerosine)?
|
1. Pulmonary irritation by high concentration of vapor
2. CNS depression 3. SEVERE PNEUMONITIS after aspiration of liquid "Drink some gasoline from the lawn-mower: lung irritation, pass out due to CNS depression, & pneumonitis from aspirating vomitted gasoline |
|
|
What is the treatment for Petroleum poisoning?
|
Treat symptoms & support vital signs
Emesis & Gastric Lavage without Tracheal Intubation are Contraindicated |
|
|
What causes Severe Pneumonitis after aspiration of fluid?
|
Petroleum distillates
-kerosine -gasoline |
|
|
List the Aromatic Hydrocarbons
|
1. Benzene
2. Toluene* 3. Xylene* *found in alot of glues |
|
|
What are the symptoms of Benzene, Toluene, or Xylene toxicity?
|
"Glue Sniffers"
1. CNS stimulation at low doses or early in high doses followed by CNS depression in more serious poisonings 2. Kidney & Liver damage may occur after high acute doses or prolonged exposure 3. Cardiac Arrhythmias caused by Catecholamine release can be enhanced by high exposure |
|
|
What 2 things can long-term exposure to Benzene cause? What drug can cause these same things?
|
Aplastic Anemia
Leukemia *so can Chloramphenicol |
|
|
What is the treatment for Benzene, Toluene, or Xylene poisoning?
|
1. remove ingested hydrocarbon by gastric lavage only if aspiration can be prevented; DO NOT induce emesis
2. control excitement or convulsions with IV Diazepam |
|
|
What substance do the corrosives such as bleaches, metal cleaners, & rust removers contain?
|
Oxalic Acid & Oxalates
|
|
|
What are the symptoms of Oxalic Acid & Oxalate poisoning (corrosive = bleaches, metal cleaners, rust removers)?
|
1. Local irritation & corrosion of the GI tract
2. Muscle weakness, Convulsions & Collapse due to Calcium Chelation 3. Renal Tubular damage due to Calcium Oxalate precipitation |
|
|
What is the specific antidote for the Corrosives (bleaches, metal cleaners, rust removers) that contain Oxalic Acid & Oxalates?
|
Calcium Gluconate IV
|
|
|
What is the treatment strategy for Oxalic Acid & Oxalate poisoning?
|
1. precipitate Oxalate in GI by giving Calcium in any form (milk, calcium antacids)
2. Monitor Renal fxn & force fluids to prevent Oxalate crystals from depositing in kidney tubules 3. Antidote = Calcium Gluconate IV 4. DO NOT use Gastric Lavage or Emetic Compounds |
|
|
What are the symptoms of the mineral acid corrosives (Hydrochloric, Sulfuric, Acetic, Nitric, Perchloric acids)?
|
1. Irritation inflammation &/or necrosis to all parts of the GI tract exposed to corrosive
2. Death is usually due to unresolved Hypovolemic Shock after massive Hemorrhage |
|
|
What is death usually due to in Hydrochloric, Sulfuric, Acetic, Nitric, & Perchloric acid ingestion?
|
Unresolved Hypovolemic Shock after Massive Hemorrhage
|
|
|
What is the treatment for ingestion of Mineral Acid Corrosives (Hydrochloric, Sulfuric, etc)?
|
1. DO NOT use Gastric Lavage or Emesis after ingestion of acids
2. Dilute the acid with water 3. Give Analgesics to reduce pain 4. Non-specific antidote = MILK OF MAGNESIA 5. Treat symptomatically & support vital signs |
|
|
List some Strong Alkali Corrosives
|
Hydroxides in:
1. Soaps 2. Cleansers 3. Drain cleaners |
|
|
What are the symptoms of Stron Alkali Corrosives (hydroxides in soaps, cleansers, drain cleaners)?
|
1. irritation, inflammation, & tissue damage
2. Alkali are more penetrating than Strong Acids |
|
|
Which agents are more penetrating, Strong Alkali or Strong Acids?
|
Strong Alkali
|
|
|
What is the treatment for Strong Alkali Corrosives (hydroxides in soaps, cleansers, drain cleaners)?
|
1. DO NOT use Gastric Lavage or Emetics
2. Dilute the alkali with Water 3. Treat symptomatically & support vital signs |
|
|
Generally, how do Arsenic & Arsine cause toxicity?
|
By binding to Sulfhydryl groups on enzymes & interfering with cellular metabolism
|
|
|
What are the symptoms of Acute poisoning with Arsenic & Arsine?
|
1. HEMOLYSIS & HEMOGLOBINUREA
2. GI disturbances 3. CNS effects where convulsions & coma are terminal signs 4. Ventricular Arrhythmias 5. Vasodilation & increased capillary permeability 6. Hyperpigmentation of skin = Rose color complexion 7. Kidney Tubular damage |
|
|
What chemical causes Hemolysis & Hemoglobinurea along with a Rose color complexion?
|
Arsenic & Arsine
|
|
|
What are the symptoms of Chronic toxicity to Arsenic & Arsine? (6)
|
1. Polyneuritis
2. Nephritis 3. DERMATITIS = MEES' LINES -> best indicator 4. Cardiac failure 5. Cirrhosis of the liver 6. Personality changes **often sprinkled onto food to slowly kill people |
|
|
Arsenic & Arsine
|

What are Mees' lines an indicator of poisoning with?
|
|
|
What is the levels of toxicity of the differenet Arsenics from least toxic to most toxic?
|
Organic < As(5+) < As(3+) < Arsine (AsH3)
|
|
|
What is the mechanism of As(5+) toxicity?
|
Substitutes for inorganic phosphate in production of ATP
|
|
|
What is the mechanism of As(3+) toxicity?
|
binds to Sulfhydryls especially in Lipoic Acid, thus interferes with energy production
|
|
|
What is the treatment strategy for Arsenic/Arsine poisoning?
|
1. remove ingested Arsenic by lavage or emesis
2. Dimercaprol or Penicillamine can be use to chelate 3. treat symptomatically |
|
|
One of the most toxic metals because it accumulates in the body; the greatest degree of intoxication occurs in children
|
Lead
|
|
|
Where is Lead primarily stored in the body?
|
Bones but the symptoms are in soft tissues like Bone Marrow & Nervous system tissue
|
|
|
What are the symptoms of Acute INORGANIC Lead toxicity?
|
1. GI irritation
2. Kidney damage |
|
|
What are the symptoms of Acute ORGANIC lead poisoning?
|
Much more likely to get into the CNS & can even cause CNS problems in adults
|
|
|
What is Chronic Inorganic Lead poisoning referred to as?
|
Plumbism
|
|
|
What do children usually present with in Chronic Lead poisoning?
|
Lead Colic
-anorexia -constipation -Abdominal pain |
|
|
A child presents with Basophilic Erythrocyte Stippling & Microcytic Anemia. What poisoning could this be due to?
|
Lead
|
|
|
What precursor accumulates in Lead poisoning?
|
Aminolevulinic Acid = hemoglobin precursor due to inhibition of Heme synthesis -> Microcytic Anemia
|
|
|
What CNS effects are prominent in Lead-poisoned children?
|
1. Hyperirritability
2. Behavior disturbances & intellectual deficits 3. Loss of recently developed skills 4. Finally Coma & intractable convulsions |
|
|
What Neuromuscular effects can Lead poisoning cause?
|
1. Weakness
2. Paralysis 3. Incoordination 4. Arthralgia 5. "WRIST DROP" & "ANKLE DROP" due to degeneration of peripheral nerves |
|
|
What is the treatment strategy for Lead poisoning?
|
1. Remove unabsorbed lead
2. Chelation produces an organis form of lead which is more likely to cross the BBB; however, in the case of severe CNS toxicity, chelation must be used 3. Treat symptomatically 4. Calcium Gluconate for GI effects 5. Chelate kids above 10 ug/dL -Calcium DiSodium EDTA = Most effective -BAL = Dimercaprol -Penicillamine (Oral) -Succimer (oral) |
|
|
What do Mercury compounds have a very high affinity for?
|
Sulfur groups in enzymes & proteins
|
|
|
What symptoms does Metallic Mercury cause?
|
1. Acute Chemical Pneumonitis
2. Noncardiogenic Pulmonary Edema **due to Inhalation of vapors |
|
|
What are the Acute, Secondary, & Delayed effects of ACUTE INORGANIC MERCURY poisoning?
|
Acute
1. Irritation & superficial corrosion of GI 2. Abdominal pain 3. Vomiting which may be bloody Secondary 1. Diarrhea 2. Acute renal tubular necrosis 3. Shock Delayed 1. Severe kidney damage leading to Anuria 2. Severe GI damage & hemorrhage |
|
|
What are the Early , Late, & Continued Exposure symptoms of CHRONIC INORGANIC MERCURY poisoning?
|
Early
-salivation -Stomatitis = swollen, bleeding gums -rarely: "mercury line" Late -Erethism = uncontrollable blushing; emothional instability; tremor -may lose teeth Continued Exposure: -course, jerky movements -drowsiness, depression -loss of memory -hallucinations, delusions -mania |
|
|
What are the effects of Chronic Organic Mercury (Methyl & Tetraethyl Mercury) exposure?
|
-Paresthesia
-Muscle twitching -Ataxia -Gross constriction of visual fields |
|
|
Where does Organic Mercury accumulate in nature?
|
plants eaten by fish (that we may eat, but probably doesn't cause much affect on us in the long run)
|
|
|
What is the treatment strategy for Acute Exposure to Inorganic Mercury?
|
1. Lavage or induce emesis
2. give Milk, raw eggs, or Charcoal 3. IM Dimercaprol (for more severe) or Oral Succimer (for less severe) |
|
|
What should not be used for Chronic elemental or organic mercury exposure b/c it redistributes mercury to the brain? What may you give then?
|
Dimercaprol
Succimer may help for inorganic mercury |

