![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
What are 85-90% of Hypertension cases due to?
|
Unknown = Essential HTN
|
|
|
How is Hypertension usually manifested initially?
|
usually a SILENT DISEASE that is asymptomatic as most hypertensives usually feel well & progressive cardiovascular damage develops very gradually
Generally remains asymptomatic for 15-20 years until vital organs (Heart, brain, kidneys) become damaged |
|
|
What is the 1st step in the treatment of Hypertension?
|
Life-stype modifications
1. exercise 2. weight reduction 3. moderatation of dietary salt, fats, & alcohol 4. avoid or reduce smoking 5. before, or together with, drug therapy |
|
|
What is the most common cause of treatment failure in treating HTN?
|
Non-compliance
|
|
|
List the 3 main goals of Anti-HTN drug treatment
|
1. lower BP & keep it normal
2. reduce CV risks 3. produce minimal side-effects without decreasing quality of life |
|
-
|
-
|
|
|
Aside from mechanism of action, how do most Anti-HTN drugs differ?
|
Adverse or side effects
|
|
|
At what diastolic pressure is there inadequate Coronary perfusion & increased CV morbidity & mortality?
|
lower than 90 mm Hg
|
|
|
How do drugs lower BP?
1. Reduce blood volume = ? 2. Interrupt Sympathetic tone = ? 3. Vasodilation = ? |
1. Diuretics
2. Sympatholytics 3. Direct Vasodilators; CCA's; ACE inhibitors & AT-II Antagonists |
|
|
What are the 2 mechanisms in which Diuretics lower BP?
|
1. initially deplete body Na+ stores -> reduce blood volume
2. Later activate K+ channels -> reduce vascular resistance |
|
|
Diuretic that is recommended for Mild to Moderate HTN & when used:
-alone will lower BP in 40-60% of patients, and -in drug combinations will enhance efficacy of other Anti-HTN drugs |
Thiazide
-Chlorthalidone -Indapamide -Metolazone -Quinethazone |
|
|
Which doses of Diuretics are higher, those used for Anti-HTN purposes or those used for Diuresis?
|
Diuresis = 100-200 mg
Anti-HTN = 6-12 mg |
|
|
Which diuretic is primarily used for HTN?
|
Thiazide
-Chlothalidone -Indapamide -Metolazone -Quinethazone |
|
|
Which diuretic is primarily used for CHF?
|
Loop
-Furosemide -Torsemide -Bumetanide -Ethacrynic acid |
|
|
What 2 general types of Sympatholytic Drugs are used to lower BP?
|
1. Central agonists = stimulate medullary receptors
2. Peripheral Antagonists = block receptors at nerve endings |
|
|
Why are Sympatholytics generally not recommended for monotherapy?
|
produce Side-effects of:
1. Postural Hypotension 2. Sodium retention |
|
|
List the 4 Centrally Acting Sympatholytics
|
1. Clonidine
2. Methyldopa 3. Guanabenz 4. Guanfacine |
|
|
This is a prodrug Centrally Acting Sympatholytic
|
Methyldopa = converted to alpha-methylnorepinephrine
|
|
|
What is the mechanism of action of the Centrally Acting Sympatholytics?
|
Act as AGONISTS that stimulate Medullary Alpha-2 adrenergic receptors to reduce peripheral Sympathetic tone & lower BP by:
1. decreasing Vasoconstrictor tone = Vasodilation 2. Decrease Renal Renin Secretion |
|
|
How are the Centrally Acting Sympatholytics usually administered?
Which one can be used as a Transdermal or Skin Patch? |
Orally
Clonidine |
|
|
What are the side effects of the Centrally Acting Sympatholytics?
|
CNS effects = Sedation, Nausea, dizziness, nightmaires, depression, Postural Hypotension
Dry mouth |
|
|
Sudden withdrawal of this Centrally Acting Sympatholytic may cause of Hypertensive Crisis
|
Clonidine
|
|
|
Centrally acting Sympatholytic that may produce Hemolytic Anemia with a Positive Coombs test
|
Methyldopa
|
|
|
What are the possible side effects of Methyldopa use?
|
1. Hemolytic anemia with + Coombs test
2. Hepatotoxicity 3. Gynecomastia 4. Lactation |
|
|
What 3 drugs act by binding to Secretory Vesicles that normally store & release NE in peripheral endings?
|
1. Guanadrel
2. Guanethidine 3. Reserpine *reduce sympathetic activity by preventing NE release to reduce sympathetic activity, cause vasodilation, & lower BP |
|
|
Sudden release of endogenous NE when _______ is given IV may elevate BP
|
Guanethidine
|
|
|
What are the common ADR's of Guanethidine?
|
1. Postural Hypotension
2. Fluid retention 3. Diarrhea 4. Retrograde ejactulation |
|
|
What are the common ADR's of Reserpine?
|
1. Sedation
2. Psychic depression 3. Nasal stuffiness 4. Dry mouth 5. GI disturbances |
|
|
List the Non-selective Beta Antagonists
|
1. Propranolol
2. Cartelol 3. Nadolol 4. Sotalol 5. Timolol |
|
|
List the Cardioselective Beta-1 blockers
|
BEAM
1. Betaxolol & Bisoprolol 2. Esmolol 3. Acebutolol 4. Atenolol 5. Metoprolol |
|
|
List the 3 Intrinsic Sympathomimetic Activity Beta blockers that manufacturers claim produce less Cardiac Depression & are preferred for Hypertensive pts with CHF
|
PAP
1. Penbutolol 2. Acebutolol 3. Pindolol |
|
|
List the 3 ways in which Beta blockers lower BP
|
by blocking Beta receptors in:
1. Heart to reduce CO = Beta-1 2. Kidneys to reduce Renin secretion = Beta-1 3. CNS to reduce sympathetic vasomotor tone |
|
|
In what group of people are the Beta blockers most efficacious in?
|
Caucasians & younger people
|
|
|
In what patients are Beta blockers recommended for monotherapy?
|
Young White Males
|
|
|
What are Beta blockers combined with other Anti-HTN drugs to counteract? (2)
|
1. Reflex Tachycardia caused by Vasodilators
2. Increased Renin secretion caused by Thiazide & Loops Diuretics |
|
|
What may Beta blockade worsen the symptoms of?
|
1. Pts with reduced Myocardial reserve = Beta-1 blockade
2. Asthma = Beta-2 blockade 3. Peripheral Vascular Insufficiency 4. Diabetes = Beta-2 blockade of Insulin release |
|
|
When may Beta blockers increase exercise tolerance?
When may they decrease exercise tolerance? |
In patients being treated for Angina
In patients with CHF -> reduces CO -> earlier onset of fatigue |
|
|
How may Beta blockers predispose to Atherogenesis?
|
1. increasing plasma Triglycerides
2. decreasing HDL-cholesterol |
|
|
What does Beta blockade delay the recovery of>
|
Normoglycemia b/c it inhibits hyperglycemic responses mediated by Epinephrine on pancreatic Beta-2 receptors to release Insulin
|
|
|
What are minor side effects of Beta blockers?
|
GI = NVD, constipation
CNS = insomnia, lassitude, nightmares, depression Skeletal muscle tremors |
|
|
List the common ending for the Alpha-1 antagonists
|
-AZOSIN
1. Prazosin 2. Terazosin 3. Doxazosin |
|
|
How do the "-ZOSIN's" reduce blood pressure?
|
Alpha-1 blockade reduces NE-induced vasoconstriction to dilate both arteries & veins
|
|
|
What are the common ADR's of the -AZOSIN's?
|
1. Postural Hypotension (usually with 1st dose)
2. Dizziness, headache, drowsiness, palpitations, heachache, easy fatigability |
|
|
What 2 drugs have combined Alpha & Beta blockade?
|
1. Labetalol
2. Carvedilol *lower BP by non-selective blockade of both Alpha- & Beta receptors |
|
|
What is the Beta:Alpha block ration after ORAL LABETALOL is given?
|
Beta:Alpha = 3:1
|
|
|
What are the ADR's of Labetalol & Carvedilol?
|
1. Orthostatic Hypotension
2. Bronchospasm 3. Hepatotoxicity |
|
|
What are Labetalol & Carvedilol used mainly for the treatment of?
|
1. Hypertensive emergencies
2. Pheochromocytoma = tumor of the Adrenal Medulla that secretes Epi & NE |
|
|
Vasodilators given orally for Chronic Anti-HTN treatment
|
Hydralazine or Minoxidil
|
|
|
Vasodilators given IV for Hypertensive emergencies (5)
|
1. Sodium Nitroprusside
2. Diazoxide 3. Fenoldopam 4. Enalaprilat 5. Nicardipine *FENDS |
|
|
These 3 vasodilators dilate ARTERIES selectively without affecting venous smooth muscles
|
1. Hydralazine
2. Minoxidil 3. Diazoxide |
|
|
Dilates arteries by acting as a Dopamine D1-agonist
|
Fenoldopam
|
|
|
Non-selective or balanced vasodilator that dilates both arteries & veins
|
Sodium Nitroprusside
|
|
|
Are Vasodilators used for Monotherapy? Why?
|
No
Anti-hypertensive effects tend to diminish with time b/c of Reflex Tachycardia & increased Renin secretion |
|
|
When are Vasodilator drugs most effective?
|
When combined with other drugs to prevent undesirable side-effects
|
|
|
What are Hydralazine & Minoxidil combined with?
|
1. Diuretics = to avoid fluid retention
2. Beta blockers = to diminish Renin secretion & Reflex Tachycardia -Renin secretion blockage = Beta-1 blockage -Reflex Tachycardia blockage = Beta-1 blockage |
|
|
Hypotension produced by any Vasodilator drug will be accompanied by these things
|
1. Reflex Tachycardia, increased Myocardial contractions
2. Increased Renin secretion 3. Fluid retention, headaches, flushing, palpitations, or dizziness |
|
|
What 2 drugs may induce Anginal attacks & Myocardial Ischemia through reflex increases in Cardiac Output in Elderly patients with coronary artery disease?
|
Hydralazine
Minoxidil |
|
|
Vasodilator that may cause a Lupus-like syndrome consisting of fever, skin rashes, arthralgia, & myalgia
|
Hydralazine
|
|
|
Vasodilator that causes Hyperthrichosis (excess hair growth); topical ointment "Rogaine"
|

Minoxidil
|
|
|
List the drugs contained within the Calcium Channel Blockers class
|
1. Verapamil
2. Diltiazem 3. Dihydropyridines = "-DIPINES" -Nifedipine |
|
|
What is the mechanism of action of the CCA's in lowering BP?
|
1. reduce IC Ca++
2. relax Arteriolar smooth muscles 3. vasodilation & lower BP |
|
|
Drugs that are equally effective for monotherapy in mild to moderate HTN especially in the Elderly & African-Americans
|
Calcium Channel Blockers
Thiazides |
|
|
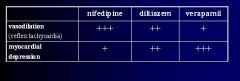
CCA that is the strongest Vasodilator and most likely to produce Reflex Tachycardia
|
Nifedipine
*also has smallest inhibition of AV conduction |
|
|
Why do Verapamil & Diltiazem not cause Reflex Tachycardia?
|
b/c they depress SA & AV node conduction directly
|
|
|
When are Verapamil & Diltiazem contraindicated?
|
in patients with SA or AV node abnormalities
CHF *may cause Bradycardia in the presence of SA node dysfunction |
|
|
MC side effect of Verapamil
|
Constipation
|
|

-
|
-
|
|
|
CCA's that are most likely to cause headache, flushing, dizziness, & peripheral edema
|
Dihydropyridines = '-DIPINE's' = Nifedipine
Greatest effect is Vasodilation |
|
|
What is the common ending for ACE inhibitors?
|
-PRIL
|
|
|
Only active ACE inhibitor, all others are prodrugs that have to be converted to the corresponding di-acid
|
Captopril
|
|
|
How do ACE inhibitors lower BP?
|
Inhibit ACE = inhibit conversion of Antiogentin I -> Angiotensin II
-Inhibit AT-II vasoconstriction -also inhibit ACE destruction of Bradykinin |
|
|
What are the side effects of the ACE inhibitors?
|
CAPTOPRIL + Hyperkalemia
1. Cough (due to Bradykinin) 2. Angioedema & Anaphylaxis(due to Bradykinin) 3. Proteinuria 4. Taste changes 5. hypOtension 6. Pregnancy proglems (fetal renal damage) 7. Rash 8. Increased renin 9. Lower angiotensin-II |
|
|
List the advantages of ACE Inhibitors
|
1. lower BP without compromising blood supply to the heart, brain, or kidneys
2. side-effects are mild, fewer, & without lipid changes 3. do not cause reflex tachycardia b/c of concurrent baroreceptor resetting or vagal activation 4. are effective orally for monotherapy & will lower BP in 50% of pts with mild to moderate HTN |
|
|
What groups of people are ACE inhibitors most effective in?
|
Young & Middle-aged Caucasians
*less effective in Elderly AA's |
|
|
What 3 things are ACE inhibitors the 1st choice of treatment for HTN in pts?
|
1. Diabetes
2. Chronic Renal disease 3. Left Ventricle Hypertrophy |
|
|
What is the common ending for Angiotensin Receptor Antagonists?
|
-SARTAN
|
|
|
Which receptor do the -SARTAN's bind to? Where is this receptor located?
|
AT1 receptor in vascular smooth muscle
|
|
|
What are the 2 important differences between Angiotensin receptor antagonists & ACE inhibitors?
|
1. -SARTAN's are more specific than ACE inhibitors b/c AT-II antagonists do not affect Bradykinin metabolism = no coughing or Angioedema
2. -SARTAN's have more complete inhibition of Angiotensin action b/c enzymes other than ACE can generate Angiotensin-II |
|
|
What are some adverse effects of the -SARTAN's?
|
Hyperkalemia
Fetal Renal toxicity |
|
|
What Anti-hypertensive drugs can be used as monotherapy?
|
1. Diuretics
2. Beta blockers 3. ACE inhibitors 4. CCA's |
|
|
With what anti-HTN drugs do Elderly males often complain of Impotence?
|
Thiazides or Sympatholytics
|

