![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
|
What is Coronary Artery Disease mainly due to?
|
Obstruction of the coronaries by Atheromatous plaques
|
|
|
When does Coronary Artery Disease start?
|
silently in childhood
**everyone develops Coronary Artery Disease |
|
|
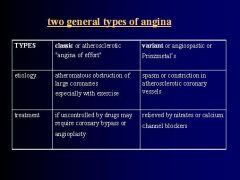
The primary symptom of heart disease; refers to chest pain caused by Myocardial Ischemia
|
Angina Pectoris
|
|
|
What characterizes Angina Pectoris?
|
Chest discomfort occurring when the amount of blood delivered to the heart by the coronary arteries cannot supply enough oxygen to satisfy the Myocardial requirement so that OXYGEN NEED EXCEEDS OXYGEN SUPPLY
|
|
|
How is Angina Pectoris typically relieved?
|
within minutes by REST or use of NITROGLYCERIN
|
|
|
Describe the chest pain associated with Angina Pectoris
|
Strangling
Vise-like Constricting Suffocating Crushing Heavy Squeezing |
|
|
Where is the site of chest discomfort in Angina Pectoris?
|
Retrosternal often radiating down the Ulnar surface of the left arm or may also involve the right or both arms
|
|
-
|
-
|
|
|
What does Oxygen supply to the heart depend on?
|
Oxygen delivery
Extraction |
|
|
What does oxygen demand of the heart depend on?
|
Cardiac workload
1. contractility 2. heart rate 3. ventricular wall tension 4. oxygen extraction is already maximal even at rest |
|
|
How can additional Oxygen be supplied to the heart?
|
By increasing Oxygen delivery through coronary blood flow
1. directly proportional to Aortic Diastolic Pressure & duration of Diastole 2. inversely proportional to coronary vascular resistence determined by: metabolic products, autonomic activity, & various drugs |
|
|
Describe the "Coronary Steal Phenomenon"
|
diseased atherosclerotic branch is unable to dilate as well as the normal branch in response to the vasodilator drug, the amount of blood supplied by the diseased branch is actually reduced because blood flow is diverted into the normal branch that is vasodilated
|
|
|
Increasing Oxygen supply through coronary vasodilation releives only acute anginal attacks but is ineffective for chronic treatment because of _____________
|
Coronary Steal
|
|

-
|

-
|
|
|
What is the mechanism of action of Nitrates
|

Decrease Preload
|
|
|
All vascular smooth muscle cells are relaxed by Nitrates, but explain how the ensuing vasodilation is uneven
|
Large veins are markedly dilated
Arterioles & Precapillary sphincters are dilated less |
|
|
What are the other effects of Nitrates aside from vasodilation? (2)
|
1. Decrease platelet aggregation
2. produce Methemoglobin |
|
|
What are the beneficial effects of the Nitrates due to in anginal relief?
|
1. Pronounced dilation of large veins = reduces Preload, myocardial oxygen demand, & cardia work
2. Redistribution of regional coronary blood flow from normal to ischemic areas due to preferential dilation of large epicardial arteries 3. Mild arteriolar dilation = reduces Afterload & myocardial oxygen demand |
|
|
What is the harmful effect of the Nitrates on angina?
|
1. Reflex increases in HR & Contractility and therefore increases myocardial oxygen demand
2. Reflex tachycardia = reduced perfusion due to shorter diastole |
|

-
|

-
|
|
|
What are other uses of Nitrates (other than for angina)
|
1. Treatment of Cyanide poisoning = sodium nitrite is used to induce formation of Methemoglobin which has very high affinity for Cyanide ion
2. Sex-enhancing drugs -inhaled amyl nitrite to heighten climax by increasing coronary flow -nitroglycerin patches or ointment for impotence |
|
|
What is the mechanism of action of Sildenafil?
|
Inhibits cGMP Phosphodiesterase = increases cGMP -> vasodilation in the Corpus Cavernosum -> enhanced erection in 9 of 10 male patients
|
|
|
What are common side-effects of Sildenafil? (5)
|
1. Headache
2. Dyspepsia = indigestion 3. Nasal congestion 4. Visual disturbances = blue-green color vision 5. Priapism "a guy taking Sildenafil has so much sex he sees Green & his dick hurts (priapism). So much sex gives him a headache & indigestion (b/c he just ate within 20 minutes). He also snots all over the girl" |
|
|
When is Sildenafil contraindicated?
|
Elderly males with CV disease especially if they are receiving Nitrate Therapy for Angina or CAD
|
|
|
Why are Sildenafil & Nitrates contraindicated?
|
b/c nitrates increase cGMP systematically, Sildenafil can potentiate nitrate effects to cause extreme HYPOTENSION that is sometimes fatal
|
|
|
What are the alternative uses of Sildenafil? (2)
|
Postmenopausal women for Sexual dysfunction
Babies with Pulmonary HTN |
|
|
What are the 2 newer drugs related to Sildenafil?
|
1. Vardenafil
2. Tadalafil = erection from single dose lasts 24-36 hours |
|
|
Which nitrates are metabolized rapidly & how?
|
Oral nitrates
Hepatic reductase |
|
|
What are the routes of administration for nitrates in chronic treatment?
|
1. Inhalation
2. Sublingual 3. Oral 4. Transdermal (skin patch or ointment) |
|
|
What is the preferred routed for Nitroglycerin & Isosorbide Dinitrate?
|
Sublingual for rapid absorption & to avoid hepatic destruction
|
|
|
What are the fast acting preparations fo Nitrates?
|
1. inhaled Amyl nitrite
2. IV Sodium Nitroprusside = dilates arteries & veins equally |
|
|
What is Sublingual Nitroglycerin used for?
|
Immediate anginal relief b/c its action is rapid (onset 1-3 min) & short (10-30 min)
**not suitable for maintenance of chronic therapy |
|
|
What is done to minimize tolerance of Nitrates during chronic treatment?
|
Use lowest effective doses with nitrate-free intervals of 10-12 hours daily
|
|
|
What are the Acute Toxicity symptoms of the Nitrates?
|
Pronounced vasodilation resulting in Orthostatic Hypotension, Tachycardia, & throbbing Headaches
|
|
|
What does frequent repeated exposure to Nitrates result in?
|
Tolerance or a marked reduction in magnitude of most effects
|
|
|
Describe "Monday Disease"
|
Industrial exposure to Nitrates
-headache & dizziness on Mondays as tolerance diminishes on weekends; symptoms gradually disappear during weekdays when tolerance develops again with continuous exposure |
|
|
What are 2 important cardiovascular actions of intracellular calcium?
|
1. triggers contraction in both the Myocardium & vascular smooth muscles
2. required for pacemaker activity of the SA node & for conduction thru the AV node |
|
|
What are the 2 major types of Cardiovascular Calcium channels?
|
1. L-channel = long-lasting
2. T-channel = transient **Calcium ions flow thru open pores in the calcium channels |
|
|
What are Calcium Channel Antagonists (CCA's)?
|
Orally active drugs that bind to L-type Channels in the Myocardium & vascular smooth muscles
|
|
|
What opens Calcium channels in the Heart & vascular smooth muscle?
|
Beta-adrenergic stimulation enhances calcium entry
|
|
|
What are the most sensitive smooth muscles to CCA's?
|
Vascular but also bronchiolar, GI, & uterine muscles are relaxed
|
|
|
Among the blood vessels, which are more sensitive to CCA's?
|
Arterioles > Veins
|
|
|
CCA:
-Chemical class = Dihydropyridine -Binding site = 1A -Tissue selectivity = Vascular |
Nifedipine
|
|
|
CCA:
-Chemical Class = Benzothiazepine -Binding site = 1B -Tissue selectivity = in-between |
Diltiazem
|
|
|
CCA:
-Chemical class = Phenylalkylamine -Binding site = 1C -Tissue selectivity = Myocardial |
Verapamil
|
|
|
What are the major cardiac effects of the CCA's?
|
1. Decreased contractility
2. reduced SA node impulse generation 2. slowed AV node conduction |
|
|
CCA that has the strongest Vasodilation effect
|
Nifedipine
|
|
|
CCA that has the strongest Cardiac Effects
|
Verapamil
|
|
|
CCA that has "in-between" effects on Vasodilation & Myocardial depression
|
Diltiazem
|
|
|
Which CCA is most likely to produce Reflex Tachycardia? Why?
|
Nifedipine = causes most pronounced hypotension for reflex tachycardia, with little or no inhibition of SA or AV nodal function
|
|
|
Why are Verapamil & Diltiazem not as likely to elicit Reflex Tachycardia?
|
They are weaker Vasodilators & slow the heart by depressing SA & AV node function directly
|
|
|
What are the beneficial effects of Nifedipine due to in the treatment of Angina?
|
1. Coronary Vasodilation = increased myocardial oxygen supply
2. vasodilation of systemic arteries = decreased Afterload ***#1 is most significant |
|
|
What is the potential harmful effect of Nifedipine?
|
Increased risk of MI resulting from:
-Pronounced hypotension -> reflex tachycardia -> increased cardiac workload *especially applicable to Hypertensive patients with or without diabetes |
|
|
What are the beneficial effects of Verapamil & Diltiazem due to for the treatment of Angina?
|
1. Reduced SA automaticity & AV conduction
2. decreased myocardial contractility & bradycardia 3. REDUCED CARDIAC WORKLOAD |
|
|
What are the potential harmful effects of Verapamil & Diltiazem?
|
Serious cardiac depression that could result in:
1. cardiac arrest 2. AV block 3. CHF |
|
|
What are the "other" actions of CCA's? (2)
|
1. inhibition of Insulin secretion
2. interference with Platelet aggregation |
|
|
What are the general side effects of the CCA's?
|
1. flushing
2. edema 3. dizziness 4. nausea 5. constipation CCA = Constipation, Color (red = flushing), Aversion (nausea) |
|
|
What may Verapamil & Diltiazem reduce the renal clearance of?
|
Digoxin = could enhance its toxicity
|
|
|
In what patients should Verapamil & Diltiazem not be used?
|
pts with Ventricular dysfunction or SA-AV node disturbances
|
|
|
What Beta blockers are commonly used for Angina treatment?
|
Atenolol
Metoprolol Propranolol Nadolol |
|
|
What type of Angina are the Beta blockers extremely useful for the management of? Why?
|
Angina associated with effort
B/c they reduce myocardial oxygen requirements at rest & during exercise |
|
|
T or F: Beta blockers produce better outcome & symptomatic treatment than CCA's
|
True
|
|
|
Aside from Angina, what else are the Beta blockers valuable for treating?
|
Silent or Ambulatory ischemia which does not cause pain but is detected by appearance of ECG signs of ischemia
Long-term Beta-adrenergic blockade reduces the total amount of "ischemic time" per day |
|
|
What have studies on Beta-adrenergic Antagonist been shown to do?
|
1. reduce mortality in patients with MI
2. improve survival & prevent stroke in hypertensive patients |
|
|
Beta blockers act by ____________________
Beta blockers do not _________________ |
decreasing sympathetic tone to decrease Cardiac Output
dilate coronary arteries |
|
|
What does Anginal relief result from when using Beta blockers?
|
Decrease sympathetic activity -> decreased contractility, HR, & vasoconstriction -> DECREASED CARDIAC WORKLOAD -> DECREASED OXYGEN DEMAND
Bradycardia also prolongs Diastole & increases Myocardial perfusion time |
|
|
What is the harmful effect of Beta blockade?
|
may induce or worsen CHF whenever sympathetic activity prodives critical support for cardiac performance as in pts with Acute MI or Decompensated Heart Failure
|
|
|
What do Beta blockers usually increase the tolerance to?
|
Exercise when used for treatment of angina
BUT in patients with CHF exercise tolerance may be decreased by the reduction in CO |
|
|
In what type of patients should Beta blockers be used in caution when treating Angina? (4)
|
1. Reduced Myocardial reserve
2. Asthma 3. Peripheral vascular insufficiency 4. Diabetes |
|
|
Why are Beta blockers potentially harmful in Variant Angina?
|
Slow heart rate & prolong ejection time -> Left Ventricular End-Diastolic Volume increases -> increased Myocardial oxygen requirement
|
|
|
Beta blockers:
1. may predispose to ______ 2. Delays the recovery of _____ |
1. Atherogenesis by increasing plasma triglycerides & decreasing HDL-cholesterol
2. Normoglycemia b/c it inhibits hyperglycemic responses mediated by Epinephrine = Beta-2 receptors in Pancreas |
|
|
What are the minor side-effects of Beta blockers? (2)
|
GI = diarrhea, constipation, nausea, vomiting
CNS = insomnia, lassitude, nightmares, depression |
|
|
What effect will effective Antianginal therapy do?
|
1. increase exercise tolerance
2. decrease frequency & duration of MI |
|
|
Which drugs are better for Variant/Angiospastic Angina?
|
Nitrates & CCA's = dilate Coronary BV's
|
|
|
What are the most effective drug combinations for Antianginal therapy?
|
1. Beta blockers + CCA's
2. 2 CCA's (eg Nifedipine + Verapamil) |
|
|
How can the potentially harmful effects of the CCA's or Beta blockers be prevented?
|
by combined treatment with Nitrates or vice versa
|
|
|
How can Reflex Tachycardia be minimized when using Antianginal drugs?
|
Combining Nitrates with CCA's or Beta blockers
|
|

-
|

-
|

