![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
What are the clinical features of Parkinson's Disease? (4)
|
1. Tremor (at rest)
2. Rigidity 3. Bradykinesia = extreme slowness in movement 4. Mask-like expression |
|
|
What can Parkinson's Disease be a complication of?
|
1. Influenza epidemic of 1918
2. certain medications 3. MPTP toxicity 4. other neurologic disorders -Progressive Supranuclear Palsy -Shy-Drager Syndrome -Creutzfeld-Jacob Disease |
|
|
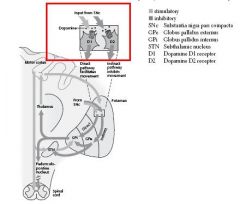
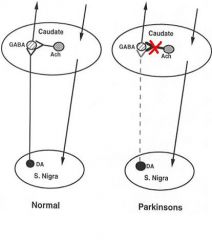
What is the pathophysiology of Parkinson's Disease?
|

Loss of Nigrostriatal Dopamine neurons = pale Substantia Nigra
Loss of Dopaminergic innervation of the Basal Ganglia |
|
|
What are the 2 families of Dopamine receptors?
|
D1-like = D1 & D5
D2-like = D2, D3, & D4 |
|
|
What is important for the greatest efficacy in therapeutic strategy for Parkinson's treatment?
|
balance between D1 & D2
|
|
|
What is the Primary Strategy in Parkinson's treatment? Secondary?
|
Primary = replace Dopamine
Secondary -Dopamine agonists -block Dopamine catabolism -Anticholinergics -Antivirals |
|
|
Since Dopamine does not cross the BBB, what is given to replace it?
|
L-DOPA
"The Lazy Dog Naps Easily" |
|
|
What are the pharmacological effects of L-DOPA?
|
Motor = reversal of rigidity, tremor, & bradykinesia
Psychic -improved mental function -sense of well-being |
|
|
What are the Early Side Effects of Levodopa (L-DOPA)?
|
GI = N/V = due to stimulation of the Chemoreceptor Trigger Zone (CTZ) (very common)
Cardiovascular -Postural Hypotension (very common) = due to stimulation of D1 Dopamine receptors in Kidney & Vasculature -HTN, esp. w/ Sympathomimetics -Arrhythmia -Tachycardia Neuroendocrine -decreased Prolactin secretion = due to stimulation of D2 receptors in Pituitary |
|
|
What are the long-term Motor side effects of L-DOPA?
|
1. fluctuations in efficacy
2. "on-off" - symptoms reappear periodically 3. "wearing off" - effects don't last as long |
|
|
What are the long-term Neurological side effects of L-DOPA?
|
Abnormal movements
-Dystonia -Dyskinesias -Chorea **this is very common |
|
|
What are the long-term Psychic effects of L-DOPA?
|
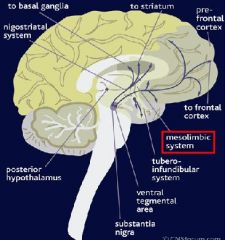
Hallucinations, Paranoia, Mania, Anxiety, Depression
-due to stimulation of dopamine receptors in targers of the Mesolimbic & Mesocortical pathways -can lower dose or treat with newer Antipsychotics that do not tend to produce EPS |
|
|
What are the long-term Neuroendocrine side effects of Levodopa?
|
Renewed Sexual interest & behavior
Hypersexuality |
|
|
L-DOPA Pharmacokinetics:
1. Route of Administration 2. Absorption 3. Peak Levels 4. t1/2 5. Metabolism & excretion |
1. Oral
2. dependent on GI transit time 3. 1/2 to 2 hrs after administration 4. 1-3 hours 5. >95% decarboxylated in periphery & excreted in urine |
|
|
What is L-DOPA virtually always administered with? Why?
|
Carbidopa
-Increases Levodopa to the brain -can used decreased doses -decrease side effects, esp. GI |
|
|
Non-ergot D2/D3 Dopamine agonists
|
1. Pramipexole
2. Ropinerole "Ropin some Prami's" with D2/D3 |
|
|
2 Ergot Dopamine Agonists
|
Bromocriptine
Pergolide |
|
|
D1/D2 Dopamine agonist
|
Apomorphine
|
|
|
What is the mechanism of action of the Dopamine agonists?
|
Agonist at D2 & other Dopamine receptors
Activity at D3 receptor may confer greater efficacy & may mediate neuroprotective effects |
|
|
Which Dopamine agonists may be used as Monotherapy or with L-DOPA?
|
D2/D3 agonists = Pramipexole & Ropinerole
**others are used with L-DOPA in pts with "on-off" or whose symptoms are not controlled by L-DOPA |
|
|
What are the side effects of the Dopamine Agonists?
|
N/V
Postural Hypotension Hallucinations |
|
|
Selective MAO-B inhibitor that blocks that catabolism of Dopamine
|
Selegeline
"Select a Gel Line" that inhibits sweating "My Ass Off" (MAO-B) |
|
|
What is the use of Selegeline?
|
Adjunct to L-DOPA
-increases efficacy -decrease L-DOPA dose -decreases "on-off" effect |
|
|
2 COMT inhibitors that block catabolism of Dopamine
|
Tol-capone
Enta-capone "Al CAPONE watched the COuntry Music Television Inhibitor" |
|
|
What are the uses of COMT inhibitors?
|
Adjunct to L-DOPA
-increases efficacy -decrease L-DOPA dose -decreases "on-off" effect |
|
|
What side effect can MAO inhibitors cause?
|
Hypertensive Crisis
-esp. MAO-A inhibitors |
|
|
What drugs can decrease GI motility and result in decreased absorption of L-DOPA?
|
Anticholinergics
|
|
|
What drug can increase L-DOPA metabolism?
|
Pyridoxine = vitamin B6
|
|
|
What are 2 Anticholinergics used to treat Parkinson's Disease? Why are they used?
|
TRIHEXYPHENYDYL & BENZTROPINE
Block the actions of Striatal Interneurons = curb the excess Cholinergic activity |
|
|
What are the side effects of Trihexyphenydyl & Benztropine?
|
1. Constipation
2. Urinary Hesitance, retention 3. Mental confusion 4. Hallucinations |
|
|
What antiviral is used to treat Parkinson's disease? What is a proposed mechanism?
|
Amantidine
May release Dopamine and/or have anticholinergic properties **used as adjunt to L-DOPA |
|
|
What are the side effects of Amantidine?
|
Similar to Dopamine agonists
May produce Livedo reticularis, Peripheral Edema, & Headache |
|
|
What is the cause of Drug-induced Parkinsonism?
|

Blockade of Striatal Dopamine receptors
|
|
|
What drugs most commonly produces Drug-induced Parkinsonism? What is the treatment?
|
Antidopaminergic, antipsychotic drugs such as HALOPERIDOL
Tx = Trihexyphenidyl & Bentropine |
|
|
What are the clinical features of Huntington's Disease?
|
1. Progressive Chorea = abnormal involuntary movements
2. Progressive Dementia |
|
|
What is the pathology of Huntington's Disease?
|
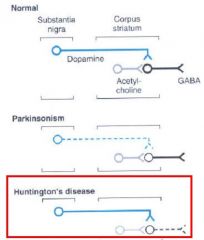
Functional overactivity of Dopaminergic Nigrostriatal pathways due to loss of Striatal GABAergic neurons projecting to the Globus Pallidus
|
|
|
What is the treatment for Huntington's Disease?
|
Haloperidol
|
|
|
What are the clinical features of Tourrette's Syndrome?
|
Tics
Involuntary movements or outbursts |
|
|
What is the pathology of Tourette's Syndrome?
|
Unknown, but involves increased activity of Striatal neurons
|
|
|
What is the treatment of Tourrette's Syndrome?
|
Haloperidol
|
|
|
What are Physiologic Postural Tremors? What receptors does it involve?
|
Normal phenomenon enhanced by anxiety, fatigue, thyrotoxicosis, or administration of Sympathomimetics
Beta-1 & Beta-2 receptors |
|
|
What are Essential Tremors? What receptors are primarily involved?
|
Essential Tremor = neurological disorder characterized by shaking of hands (and sometimes other parts of the body including the head), evoked by intentional movements
Beta-1 receptors |
|
|
What is the treatment for Tremors?
|
Physiologic & Essential = Propranolol (Beta-1 & 2 blocker)
Essential = Metoprolol (Beta-1 selective) |
|
|
What is "Spasticity"?
|

Violent, painful, involuntary muscle contractions resulting from dysfunction or descending motor input
|
|
|
What can cause Spasticity?
|
Trauma, inflammation, or diseases such as Multiple Sclerosis & Cerebral Palsy
|
|
|
What is the site of action of Diazepam as an Antispastic drug? What is its mechanism?
|
Spinal & Supraspinal
Enhances GABAergic transmission at GABA-A receptors |
|
|
What are the principal uses of Diazepam as an Antispastic drug?
|
All types of Spasticity associated with Spinal Cord lesions
Cerebral Palsy |
|
|
Diazepam as an Antispastic:
1. Administration 2. Duration of action |
1. Oral or IM
2. >24 hrs due to active metabolites |
|
|
What is the site of action of Baclofen as an Antispastic drug? What is the mechanism?
|
Gamma motor neurons in the Spinal Cord
GABA-B agonist = inhibits release of excitatory transmitters & increases threshold for excitation thus decreasing mono- & polysynaptic spinal reflexes |
|
|
What are the side effects of Baclofen?
|
1. Drowsiness
2. Insomnia 3. Weakness 4. Dizziness 5. Confusion **side effects can be decreased with Intrathecal administration |
|
|
What are the principal uses of Baclofen?
|
Spinal Cord injuries & Multiple Sclerosis
|
|
|
Baclofen pharmacokinetics:
1. Administration 2. Half-life 3. Excretion? |
1. rapidly absorbed after oral administration
2. 3-4 hours 3. unchanged in urine |
|
|
What is Dantrolene's site of action? What is its mechanism?
|
Muscle
reduces muscle contraction by decreasing Ca++ release from Sarcoplasmic Reticulum |
|
|
What are Dantrolene's side effects?
|
Generalized Muscle Weakness
Hepatotoxicity *"Dan the Lean" man has muscle weakness & Liver problems |
|
|
What are the principal uses of Dantrolene? What is another use?
|
Paralysis & Hemiparalysis
Cerebral Palsy Multiple Sclerosis Malignant Hyperthermia = hereditary condition in which certain anesthetics (e.g., halothane) cause high body temperatures and muscle rigidity |
|
|
Dantrolene pharmacokinetics:
1. Administration 2. Plasma half-life 3. Metabolism & excretion |
1. Orally
2. 9 hours 3. Hepatic metabolism & urine excretion "Dan the Lean" man gets oral for 9 hours |
|
|
What is Botox's site of action as an Antispastic drug? What is it's mechanism?
|
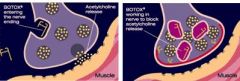
Muscle
Acts on Cholinergic vesicles to inhibit ACh release |
|
|
What are the principal uses of Botox?
|
Local muscle spasm & more generalized spastic disorders such as Cerebral Palsy
|
|
|
Botox pharmacokinetics:
1. Administration 2. Duration of action? |
1. injected into muscle
2. weeks-months after a single injection |
|
|
What 2 drugs are used for the treatment of acute muscle spasm cause by acute trauma or strain? What is their mechanism of action?
|
Cyclobenzaprine & Carisoprodol
Act as either a sedative &/or at the level of the brain stem or spinal cord "Clarissa-Pro-Doll drives her Circle-Benz-aprine so much she gets sleepy (sedatives) & doesn't have muscle spasms" |
|
|
What is Cyclobenzaprine structurally relted to? What is it not effective against?
|
Tricyclic Antidepressants
Spasms due to Cerebral Palsy or Spinal Cord injury |
|
|
What is Carisoprodol metabolized into? What is the significance of this?
|
Meprobamate = sedative-hypnotic with abuse potential
"Clarissa the Pro Doll" has a daughter named "Me Probe a Mate" who is sedated all the time, with whom she is addicted to |

