![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
68 Cards in this Set
- Front
- Back
|
Defintion: Drug that decreases anxiety without sedation
|
Anxiolytic
|
|
|
Definition: Decrease in motor activity, coordination, & mental acuity
|
Sedation
|
|
|
Definition: Increased tendency to sleep, but easily awakened
|
Hypnosis
|
|
|
Definition: Sleep induction, not easily awakened
|
Anesthesia
|
|
|
The general principle of current CNS depressants is that they generally do what?
|
enhance inhibitory neurotransmission
|
|
|
What is the difference between Complete depressants & Incomplete depressants?
|
Complete depressants produce Anesthesia
Incomplete depressants do not produce Anesthesia |
|
|
What is the mechanism of action of the Barbiturates?
|
1. Bind to the Barbiturate binding site on the GABA-A receptor
2. increase Chloride ion channel flux by increasing channel open time = Duration 3. Decrease neuron firing |
|
|
List some Complete CNS depressants Anxiolytics
|
1. Barbiturates
2. Ethanol 3. Chloral Hydrate 4. Paraldehyde **produce Anesthesia |
|
|
List some Incomplete CNS depressant Anxiolytics
|
1. Benzodiazepines
2. Non-benzodiazepine BZ/omega receptor agonists -Zolpidem -Zaleplon -Eszopiclone |
|
|
List some Non-depressant Anxiolytics/Hypnotics
|
1. Buspirone
2. SSRI's 3. Melatonin agonist = Ramelteon 4. Antihistamines = Diphenhydramine 5. Beta-blockers = Propranolol |
|
|
What is the common ending for Barbiturates?
|
"-barbital" + Thiopental
|
|
|
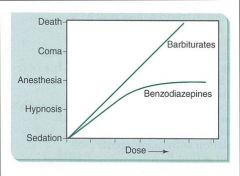
What effects do Barbiturates have on the CNS?
|
1. Complete CNS depressants
-Sedation, Hypnosis, Anesthesia, Coma, Death 2. Paradoxical excitement & euphoria |
|
|
What effects do Barbiturates have on the CNS?
|
NO EFFECT UP TO ANESTHETIC DOSES
At Anesthetic doses: 1. decreases Respiration 2. decreases Blood Pressure due to Medullary depression |
|
|
What effects do Barbiturates have on the Liver?
|
Chronic use increases Microsomal enzyme activity
-pharmacokinetic tolerance & can decrease plasma levels of other drugs |
|
|
Barbiturates can increase the synthesis of a certain product & are therefore contraindicated in this disease
|

Porphyria
**increase the synthesis of Porphyrin **Barbiturate causes increased Heme metabolism; Heme usually has negative feedback on ALA synthase (which produes Porphyrin) |
|
|
What are the clinical uses of Barbiturates?
|
1. Hypnotics
-have been largely replaced by Benzodiazepines & Non-Benzodiazepine BZ/Omega receptor agonists 2. Anticonvulsants 3. Anesthetics |
|
|
Long-acting Barbiturate that is used for its Sedative & Anticonvulsant properties
|
Phenobarbital
|
|
|
2 Intermediate-acting Barbiturate that are used for their Hypnotic effects
|
Pentobarbital
Secobarbital "Sleep Producing" Barbs |
|
|
Ultra-short acting Barbiturate that is used for Anesthesia
|
Thiopental
|
|
|
Acute Barbiturate Toxicity:
1. Causes? 2. Signs/Symptoms? 3. Treatment? |
1. Overdose or interaction with other CNS depressants
2. Decrease in respiration & Blood Pressure; loss of consciousness 3. Maintain Respiration & BP; removal of drug |
|
|
What are the Chronic Toxicities associated with Barbiturates?
|
1. ADDICTION = more common than opiate addiction
2. Tolerance develops over time 3. Withdrawal includes anxiety, tremor, nausea, vomiting, seizures, weight loss, psychiatric rxns **treatment includes measured reduction over time (2-3 wks) |
|
|
Barbiturate Pharmacokinetics:
1. What does it diffuse across? 2. What does distribution depend on? 3. What accounts for differences in duration of action? 4. What can cause drug interactions? 5. Where metabolized? 6. Where excreted? |
1. All membranes
2. Lipophilicity of body part 3. Redistribution 4. Highly binds to Plasma proteins 5. Liver 6. Urine |
|
|
-Complete CNS depressant that is used as a Hypnotic with its active product being Trichloroethanol
-Irritating to G.I. -Rapid onset, short duration of action -Acute & chronic toxicity are same as barbiturates |
Chloral Hydrate
|
|
|
-Complete CNS depressant used as an Anxiolytic
-Irritating to the G.I. -Rapid onset & short duration of action -Acute & chronic toxicity are the same as Barbiturates |
Paraldehyde
|
|
|
What the is mechanism of action of the Benzodiazepines?
|
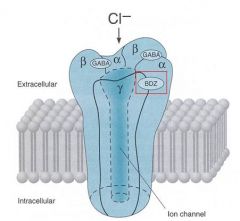
1. Bind to the Benzodiazepine binding sites (BZ/omega) on the GABA-A receptor
2. increases affinity of GABA-A receptors for GABA 3. increase the FREQUENCY of Cl- channel opening |
|
|
Give a possible reason as to why Benzodiazepines are probably Incomplete CNS Depressants
|
they act at a smaller subset of GABA-A receptors than the Barbiturates
-there are atleast 3 BZ binding site subtypes: BZ1-BZ3 |
|
|
What are the CNS effects of the Benzodiazepines?
|
1. INCOMPLETE depressant
2. Skeletal muscle relaxant = Anti-spastic (via Central effect) 3. Anticonvulsant (status epilepticus) 4. Hypnotic 5. Paradoxical excitement & euphoria |
|
|
What Benzodiazepine effects does tolerance develop to? (3)
|
1. Sedative
2. Hypnotic 3. Anticonvulsant |
|
|
Which one has more risk of Respiratory depression, Coma, & decreased Blood Pressure...Barbiturates or Benzodiazepines?
|
Barbiturates
|
|
|
What is the common ending for most Benzodiazepines?
|
"-azepam"
|
|
|
What are the 4 clinical uses of Benzodiazepines?
|
1. Anxiolytics
2. Sedative/Hypnotics = night terrors, sleepwalking 3. Muscle relaxants / Antispastic 4. Pre-anesthetic / Anesthetic |
|
|
Short acting (t1/2 = 2-4 hrs) that is the most rapidly inactivated Benzodiazepine
-Produces Anesthesia I.V. -Primarily used as Anesthetic/Pre-anesthetic in surgical settings |
Mid-azolam
|
|
|
Short acting (T1/2 = 2-4 hrs) Benzodiazepine used as a Hypnotic = short-term treatment of insomnia w/out producing morning drowsiness
|
Tri-azolam
|
|
|
Moderate acting (T1/2 = 10-14 hrs) that is an Anxiolytic/Hypnotic often used for Panic Attacks
-has rapid Oral absorption/onset |
Alpr-azolam
|
|
|
Moderate acting (t1/2 = 10-14 hrs) Benzodiazepine that is Anxiolytic, Pre-anesthetic. Generally used in Alcohol Detox & Pre-surgery anxiety
|
Chlordiazepoxide
|
|
|
Moderate acting (t1/2 = 10-14 hrs) Benzodiazepine that is Anxiolytic/Hypnotic, Pre-anesthetic
-generally used for Status Epilepticus |
Lorazepam
|
|
|
Long acting Benzodiazepine (t1/2 = 24 hrs) used as an Anti-convulsant
|
Clonazepam
|
|
|
Very long acting Benzodiazepine (t1/2 = 43 hrs) that has active metabolites
|
Diazepam
|
|
|
What are the clinical uses of Diazepam?
|
1. Anxiolytic
2. Anticonvulsants 3. Muscle relaxant 4. Antispastic 5. Pre-anesthetic |
|
|
Very long acting Benzodiazepine that has a half-life of 74 hours & has active metabolites
|
Flurazepam
|
|
|
Benzodiazepine that is fast-acting & causes amnesia = used as a "date rape" drug
|
Flunitrazepam
|
|
|
What would you treat an overdose of Benzodiazepines with?
|
Flumazenil = competitive antagonist at GABA receptor
**short t1/2 requires repeated doses |
|
|
What are the side effects & toxicities of the Benzodiazepines?
|
1. Sedation & ataxia (loss of muscle coordination)
2. Amnesia 3. Idiosyncratic responses: nightmares, irritability, anxiety, seizures 4. Abuse liability 5. Withdrawal, especially with shorter-acting compounds |
|
|
Most Benzodiazepines are administered orally, but which ones can be administered via IV & IM?
|
1. Chlordiazepoxide
2. Diazepam 3. Lorazepam 4. Midazolam |
|
|
Which Benzodiazepine can be given rectally?
|
Diazepam
|
|
|
List the 2 BZ1 agonists that are not actually Benzodiazepines
|
1. Zolpidem
2. Zaleplon **used as Hypnotics for Insomnia in those who have trouble falling asleep "Help you get your ZZZ's" |
|
|
Non-selective BZ receptor agonist that is not actually a Benzodiazepine
|
Eszopiclone
|
|
|
What is the clinical use of Eszopiclone? What are its general properties?
|
Hypnotic = for insomnia
-minimal muscle relaxant or anticonvulsant activity -less amnestic than Benzodiazepines = less memory loss -Tolerance develops to Hypnotic effects "EaSy Z's" |
|
|
Anxiolytic that is not a CNS depressant but is a partial agonist at the 5-HT(1A) site
|
Buspirone
**"1 pirate on a bus (Buspirone) takes Exit 1A to get off the stressful highway (Anxiolytic)" |
|
|
What is the onset of action of Buspirone? What does it cause at high doses?
|
Onset of action = 1-2 weeks = not useful for initial panic attacks
High doses = Dysphoric = unpleasant or uncomfortable mood = less addiction/abuse |
|
|
Anxiolytics that increase the synaptic availability of 5-HT (Serotonin)? What are they used for?
|
SSRI's & other Antidepressants
Generalized anxiety & as prophylaxis for Panic disorder |
|
|
Melatonin agonist indicated for Insomnia with prolonged sleep onset (takes a long time to fall asleep)
-MT1 & MT2 melatonin receptor agonist |
Ramelteon
|
|
|
Common OTC sedative that is a Histamine-1 (H1) blocker
|
Antihistamines = Diphenhydramine
|
|
|
Why would Beta-blockers such as Propranolol be used for Anxiety?
|
Blocks peripheral symptoms of anxiety such as Heart Rate & Tremor
|
|
|
Is Ethanol a Complete or Incomplete CNS depressant?
|
Complete
|
|
|
What is Ethanol's mechanism in being a Complete CNS depressant?
|
-affects a variety of receptors & ion channels but no specific receptor interactions have been identified
-Affects membrane fluidity at high doses |
|
|
What CNS effects does Ethanol possess?
|
1. impairs vision & muscular coordination
2. lengthens reaction time 3. decreases anxiety, removes inhibitions -> Euphoria |
|
|
What GI effects does Ethanol possess?
|
1. increases salivation & gastric secretion
2. decreases intestinal motility 3. directly irritating to mucosa -> nausea & vomiting |
|
|
What Respiratory effect does Ethanol possess?
|
little effect at low to moderate doses
Respiratory decrease at Anesthetic doses |
|
|
What Cardiovascular effects does Ethanol possess?
|
1. Vasodilation -> sensation of warmth
2. Anesthetic doses -> decrease in Blood Pressure |
|
|
What Hepatic/Renal effects does Ethanol possess?
|
1. Cirrhosis
2. increases Microsomal enzyme activity 3. increase in Urine Flow & Volume due to increase in fluid intake & inhibition of ADH |
|
|
List the metabolic pathway of Ethanol
|

-
|
|
|
What are the contraindications of Ethanol?
|
1. Hepatic disease
2. Renal disease 3. Ulcers 4. Epilepsy 5. Other CNS depressants = additive or syergistic CNS depression 6. Pregnancy |
|
|
What are the Acute Toxicity symptoms of Ethanol?
|
1. Coma
2. Hypothermia 3. Decreased Respiration 4. Vomiting |
|
|
What are the symptoms of Chronic Toxicity of Ethanol?
|
1. Withdrawal = restlessness, tremor, fear, hallucinations, convulsions
-potentially life-threatening 2. Cirrhosis of the Liver |
|
|
What is the treatment for Withdrawal symptoms of Ethanol?
|
Slowly reduce dose over time
Benzodiazepines for acute symptoms |
|
|
What is the mechanism of action of Disulfarim? What are the side effects?
|

Inhibits Acetaldehyde Dehydrogenase = Aldehyde increases
-increase in HR -dizziness -vomiting -unconsciousness -can be fatal |
|
|
What should you warn patients about when using Disulfarim?
|
usage of Alcohol-containing consumer products such as mouthwash, cough syrups, etc.
|

