![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
97 Cards in this Set
- Front
- Back
|
How are the Cholinoceptor Agonists classified pharmacologically?
How are they further classified? |
By receptor action
1. Muscarinic 2. Nicotinic Direct-acting & Indirect-acting |
|
|
How do Direct-acting cholinomimetic agents act?
How do Indirect-acting agents act? |
directly bind & activate Muscarinic or Nicotinic agents
Inhibit Acetylcholinesterase -reduce hydrolysis of ACh -increase Endogenous ACh conc. in synaptic clefts |
|
|
List the 2 groups of Cholinoceptors and the type of receptor they are
|
Muscarinic = G protein-linked
Nicotinic = Ion channel **activated by ACh |
|
|
Muscarinic receptors are G protein-linked receptors:
1. How many domains are there 2. How is it coupled to G proteins? |
1. 7 Transmembrane domains
2. Third cytoplasmic loop is coupled to G proteins |
|
|
Where are the Muscarinic receptors located? (3)
|
1. CNS
2. tissues targeted by PSNS 2. vascular Endothelium (BUT not innervated by PSNS!!!) |
|
|
Describe the structure of Nicotinic receptors
Where are they located? |
4 subunits form cation-selective ion channels
1. All ANS Postganglionic cells ("neuronal" type) 2. Muscles innervated by Somatic Motor fibers (NMJ type) 3. some CNS neurons ("neuronal type) **there is a difference in the proteins that make up the "neuronal" type and "NMJ" type = allows for selective use of drugs |
|
|
How are the Direct-acting Cholinoceptor Agonists classified?
|
1. Esters of Choline
2. Alkaloids (Muscarine & Nicotine) |
|
|
Prototypical drug agent & endogenous transmitter that has effects on both Nicotinic and Muscarinic receptors
|
Acetylcholine
|
|
|
What renders Choline Esters relatively insoluble in LIPIDS?
|
Quaternary Ammonium group
|
|
|
Choline esters:
1. acetic acid ester of choline 2. Acetic acid ester of Methylcholine 3. Carbamic acid esters of the same alcohols |
1. Acetylcholine
2. Methacholine 3. Carbachol & Bethanechol |
|
|
T or F: Choline esters are well absorbed and are distributed good to the CNS
|
False
-poor absorption -poor distribution to CNS |
|
|
1. Choline Ester that is very rapidly hydrolyzed by AChE
2. Choline Ester that is more resistant to hydrolysis 3. Choline Esters that are very resistant to hydrolysis |
1. Acetylcholine
2. Methacholine 3. Carbachol & Bethanechol |
|
|
What 2 Choline esters that have NO potency at Nicotinic receptors? Why?
|
Methacholine & Bethanechol
due to their methyl group |
|
|
Choline Ester (other than ACh) that is more penetrant into the CNS than others. Why?
|
Carbachol
b/c it has an Amine group instead of Methyl |
|
|
List the 3 Tertiary natural Cholinomimetic alkaloids
List 2 properties relative to Choline Esters |
1. Pilo-car-pine
2. Nicotine 3. Lobe-line 1. not susceptible to degradtion by AChE 2. better at penetrating CNS |
|
|
What type of compound is Muscarine? What is it's source? Does it have CNS activity?
|
Quaternary amine
Amantia muscaria mushroom CNS activity = YES!!! |
|
|
2 agonists that are chiefly Nicotinic agonists
|
Nicotine
Lobe-line |
|
|
2 agonists that are chiefly Muscarinic agonists
|
Muscarine
Pilo-carpine |
|
|
List the activation pathway when Muscarinic receptors are activated
|
1. G-protein coupled
2. activates IP3, DAG cascade = increase in IC Calcium (in some tissues i.e. smooth muscle & glands) 3. activates Gi = inhibits Adenylyl Cyclase = opens K+ channels (occurs in other tissues i.e. heart = decreases HR) |
|
|
What is the mechanism of action of the Nicotinic receptors?
|
1. ACh binds to alpha subunits
2. results in electrical & ionic changes 3. depolarization of the nerve cell or neuromuscular end plate membrane |
|
|
What happens if you have "prolonged agonist occupancy" at Nicotinic receptors?
|
1. abolishes the effector response
2. "depolarizing blockade" = lose the electrochemical gradient across the cell membrane = cell unable to fire 3. can produe MUSCLE PARALYSIS |
|
|
What are the Muscarinic cholinoceptor effects predicted from? (2)
|
1. effects of PARASYMPATHETIC nerve stimulation
2. distribution of Muscarinic receptors |
|
|
What are the Nicotinic Agonist effects predictable from?
|
Physiology of the Autonomic ganglia & Skeletal Muscle Motor End Plate
|
|
|
What do Muscarinic Agonists produce in the Eye?
|

1. contraction of the Iris sphincter = Miosis
2. Contraction of Ciliary Muscle = Accommodation = for close-up vision 3. facilitates Aqueous Humor outflow = relief of Glaucoma |
|
|
What are the Muscarinic Agonist effects on the Cardiovascular system?
|
1. reduce Peripheral Vascular resistance (by IV infusions of ACh)
2. DIRECT EFFECT = Slow Heart Rate |
|
|
What will Intravenous Infusions of ACh cause?
|
Vasodilation and reduce blood pressure by binding to Muscarinic receptors on Endothelial Cells -> NO release -> Smooth Muscle relaxation
|
|
|
What is the DIRECT EFFECT of ACh on Muscarinic receptors on Vascular Smooth Muscle? What is this masked by? When can this effect be seen?
|
Vascular Smooth Muscle contraction
masked by effects of NO released by ENDOTHELIAL CELLS In vasculature stripped of Endothelium |
|
|
What does Muscarinic Vasodilation evoke? What can mask this?
|
SNS reflex = increase in Heart Rate
Give large doses of ACh to mask the reflex = Direct Bradycardia (Muscarinic receptors in Heart contain Gi receptors = inhibit AC -> opens K+ channels -> slows HR) |
|
|
Muscarinic Effects:
1. Respiratory system 2. GI tract 3. GU tract 4. Secretory glands |
1. Constricts Bronchiolar Smooth Muscle & glands of Mucosa are stimulated to secrete (often exacerbates symptoms of Asthma)
2. Increases secretions (salivary, gastric, pancreatic, intestinal) & increases Peristaltic activity (contraction of Longitudinal muscle; relaxation of sphincters) 3. Contracts Detrusor muscle; relaxes Trigone & Sphincter muscles 4. stimulation of secretion by Thermoregulatory sweat glands (**UNDER SYMPATHETIC CONTROL**) |
|
|
What is the major site of action of Nicotinic agonists?
|
Autonomic ganglia
|
|
|
What predominant tone are present in the following:
1. Vasculature 2. Most other tissues |
1. SNS
2. PSNS |
|
|
Does Nicotine have a greater affinity for neuronal or skeletal muscle nicotinic receptors?
|
Neuronal
|
|
|
What effects do Nicotinic agonists have on NMJ's?
|
1. produces Muscle Fasciculations
2. subsequent development of Depolarization blockade = Flaccid Paralysis **Nicotinic overdose could lead to lack of respiration b/c of paralysis |
|
|
Explain "Low" dose Acetycholine
|
Only activates VASCULAR ENDOTHELIAL MUSCARINIC receptors
-NO release = Vasodilation -produces REFLEX TACHYCARDIA |
|
|
How would you block the effects of "Low" dose Acetylcholine
|
Atropine = muscarine antagonist
|
|
|
What could happen if you administered "Low" dose Acetylcholine along with a Ganglionic Blockade?
|
decrease both BLOOD PRESSURE & HEART RATE
**Ganglionic blockers would inhibit the REFLEX TACHYCARDIA provided by SNS **only DIRECT effects are observed with Ganglionic Blockade - Endothelial Muscarinic receptors are not affected |
|
|
Explain "High" Dose Acetycholine
|
1. Muscarinic receptors on Endothelial cells activated = NO = Vasodilation
2. Cardiac Muscarinic receptors are activated = direct BRADYCARDIA -slows rate of diastolic depolarization of SA node -slow AV conduction -reduces force of Myocardial contractions -shortened Atrial refractory period which can lead to atrial flutter **Vasodilation + Bradycardia = bad combination **some Sympathetic responses can be evoked by high dose ACh & may be readily apparent in the presence of Muscarinic Antagonists |
|
|
Name of a Cholinesterase inhibitor that is a simple alcohol bearing a Quaternary Ammonium group
|
Edro-phonium
|
|
|
List 3 Cholinesterase Inhibitors that are Carbamic Acid Esters of Alcohols bearing Quaternary or Tertiary Ammonium groups (Carbamates)
|
1. Neostigmine (Quaternary)
2. Physostigmine (Tertiary) 3. Carbaryl (high lipid solubility = rapid CNS effects) |
|
|
Carbamate Cholinsterase Inhibitor that has high lipid solubility and therefore has rapid CNS effects
|
Car-baryl
|
|
|
List the 9 Organophosphate Cholinesterase Inhibitors
|
1. Echo-thio-phate
2. Soman 3. Sarin 4. Mala-thion 5. Para-thion 6. Isoflurophate 7. Di-isoflurophate 8. Donepezil 9. Tacrine *"I'D PEST MD'S **2&3 are nerve agents |
|
|
2 Organophosphate Cholinesterase Inhibitors that have to be converted into active Organophosphates; are insecticides b/c insects convert them more readily
|
Mala-thion
Para-thion |
|
|
Cholinesterase Inhibitors that have poor absorption and poor CNS distribution
|
Quaternary Carbamates = Neostigmine & Pyridostigmine
*permanent charge renders them relatively insoluble in lipids |
|
|
Cholinesterase Inhibitors that are well absorbed, distribute into the CNS, and the duration of their effect is determined by stability of Inhibitor-Enzyme complex
|
Tertiary Amines = Physostigmine
|
|
|
All Organophosphate Cholinesterase Inhibitors are well absorbed topically and are distributed to all parts of the body, including the CNS...exept which one?
|
Echo-thio-phate
|
|
|
What is the primary target of the Cholinesterase Inhibitors?
|
Acetylcholinesterase
**Butyrylcholinesterase is also inhibited |
|
|
Cholinesterase Inhibitors that reversibly bind to the ACTIVE site; inhibition is short-lived (2-10 minutes)
|
Quaternary Alcohols
-Edro-phonium **there are 2 sites on AChE: Binding & Active |
|
|
AChEI that is a great diagnostic agent in Myasthenia Gravis
|
Edrophonium
|
|
|
Explain the mechanism of action of the Carbamate Ester AChEI's
|
Undergo a 2-step hydrolysis
-Covalently bind to ACTIVE site of AChE = Covalent bond of the Carbamoylated enzyme is resistant to hydration -inhibition is 30 minutes - 6 hours |
|
|
Explain the mechanism of action of the Organophosphate AChEI's
|
1. results in a phosphorylated AChE ACTIVE SITE
2. covalent phosphorous-enzyme bond is extremey stable = inhibition lasts hundreds of hours = outlast the lifetime of the enzyme protein -"Aging" strengthens phosphorus-enzyme bond |
|
|
Before aging of the Organophosphate-AChE bond, what can restore enzyme function?
|
Prali-doxime (2-PAM)
|
|
|
List the Symptoms of Cholinesterase Inhibitors
What is not affected? |
DUMBBELSS
1. Diarrhea 2. Urination 3. Miosis = constricted pupil 4. Bronchospasm 5. Bradycardia 6. Excitation of skeletal muscle 7. Lacrimation 8. Sweating 9. Salivation Not affected = Vascular Smooth Muscle = no effect on Blood Pressure |
|
|
What happens at the NMJ when low doses of AChEI are given?
High doses? |
Low = increase force of contraction
High = depolarizing neuromuscular blockade = flaccid paralysis |
|
|
What are Cholinesterase Inhibitors used for to treat in the Eye? Explain mechanism
|
Closed-angle Glaucoma
-ACh binds to Muscarinic receptor ➡ reduce intraocular pressure by causing contraction of the Ciliary Body (accommodation) ➡ facilitates outflow of Aqueous Humor |
|
|
What clinical disorders are AChEI's used for in the GI and Urinary tracts?
|
Inactivity of Smooth Muscle disorders
1. Postoperative Ileus 2. Congenital megacolon 3. Urinary retention 4. Neurogenic bladder 5. Reflux Esophagitis 6. Insufficient salivary secretion |
|
|
Drug class used to treat Myasthenia Gravis...why?
|
Cholinesterase Inhibitors
-Pyridostigmine Will allow for more ACh in the synapse of NMJ's where Nicotinic receptors are insufficient or decreased |
|
|
What drug would Cholinesterase Inhibitors be used to reverse their intoxication?
|
Atropine = Muscarinic Antagonist
|
|
|
When would Cholinesterase Inhibitors be used for treatment in the CNS?
What drug has both Anticholinesterase and Cholinomimetic actions that is used? |
mild to moderate Alzheimer's disease
Tacrine |
|
|
Mnemonic given in class for Cholinesterase Inhibitor toxicity
|
SLUDGE
Salivation Lacrimation Urinary incontinence Diarrhea GI cramps Emesis = vomiting |
|
|
What is the treatment for Cholinesterase Inhibitor Toxicity?
|
1. Atropine = Muscarinic Antagonist
2. Maintenance of vital signs (respiration) 3. Decontamination to prevent further absorption 4. Atropine parenterally in large doses **therapy may also include Pralidoxime to "rescue" un-aged inhibited enzyme |
|
|
Nicotinic Toxicity:
1. what is it usually produced by? 2. what is fatal dose? |
1. Nicotine
2. 40 mg = amount in 2 cigarettes -BUT most destroyed by burning -ingestion usually followed by vomiting = limits absorbed dose |
|
|
What are the effects of Nicotinic Toxicity?
|
1. CNS stimulation = convulsions, coma, respiratory arrest
2. Skeletal muscle end plate depolarization = RESPIRATORY ARREST 3. HTN & Cardiac Arrhythmias (SNS effects) |
|
|
What is the treatment for Nicotinic Toxicity?
|
Symptom-directed
-Muscarinic antagonists -mechanical respiration |
|
|
What is the most significant toxicity that Nicotinic toxicity is due to?
|
Chronic smoking
|
|
|
List the 2 groups and corresponding agonists of DIRECT MUSCARINIC AGONISTS
|
Choline Esters
-Acetycholine -Bethanechol -Carbachol Alkaloids -Muscarine -Pilocarpine |
|
|
List the 2 Direct Nicotinic Agonists
|
1. Nicotine
2. Lobe-line |
|
|
List the 7 Carbamate Cholinesterase Inhibitors
|
Neo-stigmine
Physo-stigmine Pyrido-stigmine Riva-stigmine Ambenon-ium Demecar-ium Carbaryl "Stigmine CAD's" |
|
|
List the 9 Organophosphate Cholinesterase Inhibitors
|
Echo-thio-phate
Soman Sarin Parathion Malathion Isoflurophate Diisopropylfluorophosphate (DFP) Donepezil Tacrine "I'D PEST MD'S" |
|
|
What 2 groups are the Nicotinic Antagonists divided into?
|
1. Ganglion blockers
2. Neuromuscular junction blockers = paralytics |
|
|
What are the Tertiary compound Antimuscarinic drugs used for?
What are the Quaternary Amine Antimuscarinic used for? |
EYE or CNS
Peripheral effects |
|
|
Prototypical Antimuscarinic that causes REVERSIBLE, COMPETITIVE blockade
|
Atropine
**not selective between M1, M2, & M3 subtypes |
|
|
What are the Cholinoceptor-Blocking drug effects on the CNS?
What do toxic doses cause? With what other drug & what disease are they used to treat? |
1. Minimal stimulant effects on CNS
2. Agitation, Hallucinations, & coma 3. Dopamine precursor in Parkinson's disease |
|
|
What effects would Atropine or any other Muscarinic Antagonist have on the EYE?
|
1. Mydriasis = dilated pupil
2. Paralysis of the Ciliary Muscle = Cycloplegia (loss of accommodation) = precipitates Acute Glaucoma in patients with Narrow Anterior Chamber Angle |
|
|
What effects does Atropine have on the on the Cardiovascular System?
|
Tachycardia
-SA node is under PSNS tone, which is sensitive to Muscarinic blockade Antimuscarinics can cause Cutaneous Vasodilation (mechanism of unknown) |
|
|
What are the effects of Atropine on the Respiratory System?
|
Bronchodilation and reduction of secretion
**anti-muscarinic drugs are not as useful as Beta-adrenoceptor stimulants in the treatment of Asthma |
|
|
What effect does Atropine have on the GI tract?
What could it be used for? |
Reduces motility & secretion in GI tract
Preoperative adjuvant before abdominal surgery |
|
|
What effect does Atropine have on the GU tract?
|
can produce Urinary retention, especially with BPH
|
|
|
What effect does Atropine have on Sweat Glands?
|
suppresses Thermoregulatory sweating (which is under SNS control!!!, but still Muscarinic receptor)
Body Temperature can be elevated = "Atropine Fever" |
|
|
What are the therapeutic applications Muscarinic Antagonists?
|
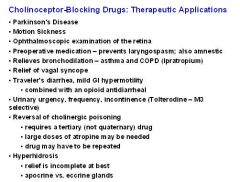
-
|
|
|
What are the symptoms of Atropine poisoning?
|
Dry mouth, Mydriasis (dilated pupil), Tachycardia, Flushed skin, Delirium
"Dry as a bone, blind as a bat, red as a beet, mad as a hatter" |
|
|
What is the mnemonic for the effects that Atropine blocks?
|
Blocks SLUD
-Salivation -Lacrimation -Urination -Defecation |
|
|
What would Atropine poisoning be treated with?
|
Physostigmine (Acetylcholinesterase inhibitor)
-penetrates CNS |
|
|
What are the contraindications for giving Atropine?
|
1. Glaucoma (especially angle-closure glaucoma)
2. Prostatic Hyperplasia = will cause Urinary Retention 3. May increase Gastric Ulcer Symptoms |
|
|
Define Ganglion-Blocking Drugs
|
block actions of ACh & other agonists at NICOTINIC receptors
-receptors located on both PSNS & SNS Autonomic ganglia |
|
|
What type of compound are all Gangion-blocking drugs?
What was the 1st developed Gangion-blocker called? |
Synthetic Amines
Tetra-ethyl-ammonium = short duration of action & used for HTN |
|
|
What Ganglion-blockers lack CNS effects?
|
Quaternary Amines & Trimethaphan
|
|
|
Ganglion-blocker that readily enters CNS
What are the side effects? |
Meca-myl-amine
Sedation, tremor, choreiform movements, mental aberrations |
|
|
What are the effects of Ganglion-blockers on the EYE?
|
1. Ciliary muscle ➡ mostly PNS tone ➡ Cycloplegia = loss of accommodation
2. Pupil = under both PNS & SNS, but PNS dominates slightly = if PNS blocked = moderate DILATION |
|
|
What effect do Ganglion-blockers have on Blood Vessels?
|
Vessels are under SNS tone
-vasoconstriction is blocked = DECREASE IN ARTERIOLAR AND VENOMOTOR TONE -reduced Blood Pressure -Orthostatic HTN = get out of bed & faint due to lack of SNS reflex |
|
|
What effect do Ganglion-blockers have on the Heart?
|
removal of PNS tone at SA node = moderate TACHYCARDIA
|
|
|
What effect would Ganglion-blockers have on the GI tract?
|
Tone is PNS = reduced secretion and motility = CONSTIPATION
|
|
|
What effect do Ganglion-blockers have on the GU system?
|
1. Hesitancy or urinary retention (especially with Prostatic Hyperplasia)
2. Sexual function is impaired b/c requires both SNS and PNS |
|
|
What effects do Ganglion-blockers have on Sweat glands?
|
blocks Thermoregulatory Sweating
|
|
|
Give an example of how Ganglion blockers inhibit Homeostatic reflexes (use NE as example)
|
Normal:NE is given ➡ Blood Pressure would increase ➡ reflex PSNS causes decreased HR to decrease CO & minimize BP
Ganglion-blockers: give NE ➡ Blood pressure rises ➡ reflex PSNS is inhibited = Heart Rate does not decrease |
|
|
List the 6 Tertiary Amine Muscarinic Antagonists
|
Atropine
Scopolamine = motion sickness Homatropine Pirenzepine (M1 selective) Tropic-amide Tolterodine "Tri-STAPH" |
|
|
List the 5 Quaternary Amine Muscarinic Antagonists
|
Atropine Methyl Nitrate
Meth-scopolamine Ipra-tropium Propan-theline Glyco-pyrrolate |
|
|
List the 3 Ganlgionic-blockers
|
Hexa-methonium
Tri-metha-phan Meca-myl-amine |

