![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
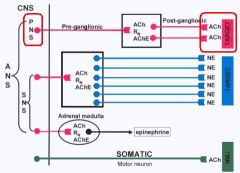
Where are the outputs for the SNS?
PNS? |
SNS = Thoracolumbar = T1-L3
PSNS = Craniosacral = CN & S2-S4 |
|
|
Where do the Preganglionic fibers of the SNS terminate? What do the Postganglionic fibers innervate?
|
Paravertebral chain ganglia
Peripheral tissues |
|
|
Adrenal Medlla
-is a modified __1__ ganglion -receives __2__ fibers and releases __3__ into the blood from __4__ cells |
1. Sympathetic
2. Preganglionic sympathetic 3. Epinephrine (80%) & NE (20%) 4. Chromaffin cells |
|
|
Where do the Preganglionic fibers of the PNS terminate?
|
in Parasympathetic ganglia located near or in the effector organ
|
|
|
What is the 3rd division of the ANS? What does it contain?
|
Enteric nervous system
Myenteric plexus (Auerbach) Submucous plexus (Meissner) |
|
|
What 2 inputs does the Enteric nervous system receive?
|
1. Preganglionic PSNS input
2. Postganglionic SNS input |
|
|
ANS division that has diffuse innervation, meaning 1 Preganglionic neuron synapses with 100s-1000s of Postganglionic neurons
|
SNS
|
|
|
ANS division that has a 1:1 ratio of Preganglionic:Postganglionic neurons
|
PSNS
|
|
|
At what places is Acetycholine used?
|

1. all Preganglionic efferent autonomic fibers
2. Somatic motor fibrers to skeletal muscle 3. Most Parasympathetic Postganglionic & a few Sympathetic Postganglionic fibers |
|
|
There are significant numbers of PSNS Postganglionic neurons that do not use ACh...what are they called & what do they use?
|
Non-adrenic, non-cholinergic autonomic fibers
Nitric Oxide & Neuropeptide Y |
|
|
What type of receptor does Norepinephrine stimulate?
|
Adrenergic (Alpha & Beta receptors)
|
|
|
Where is Norepinephrine used in the ANS?
|
Most Postganglionic Sympathetic fibers (that bind to Adrenergic receptor on target organ)
|
|
|
What is Dopamine released by in the ANS?
|
some peripheral Sympathetic fibers
|
|
|
What are the Adrenal Medullary cells analogous to?
What do they release? |
Postganglionic sympathetic fibers
Epi & NE (also ATP & Enkephalin) |
|
|
What co-transmitter is release along with ACh?
What co-transmitter is released along with NE? What do the co-transmitters do? |
Vasointestinal Peptide (VIP)
Neuropeptide Y provide long lasting, slowly developing activation of Postsynaptic target tissue |
|
|
1. What enzyme synthesizes ACh?
2. What component of ACh is synthesized in the Mitochondria? 3. What ACh component is transported into the neuron? 4. After ACh is synthesized where is it transported? |
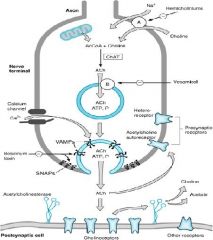
1. Choline Acetytransferase (ChAT)
2. Acetyl-CoA 3. Choline 4. Small clear vesicles |
|
|
Drug that blocks the transport of Choline into the presynaptic neuron to inhibit ACh synthesis?
|

Hemicholinium
|
|
|
Drug that blocks the transport of ACh into the vesicles in the Presynaptic neuron? (blocks the transporter)
|

Vesamicol
|
|
|
What is the release of ACh dependent on?
What triggers it? |
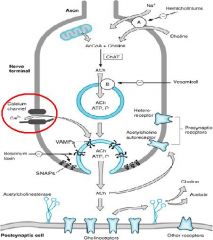
Calcium-dependent
Action Potentials |
|
|
This blocks the release of ACh from Presynaptic neurons
|
Botulinum toxin
|
|
|
What catabolizes ACh?
What does it break ACh into? |
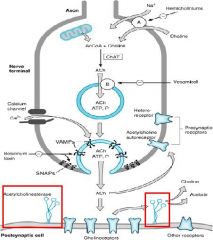
Acetycholinesterase (AChE)
Choline + Acetate |
|
|
Where are True AChE's found?
|
Postsynaptic neurons & RBC's
|
|
|
Where is Butyrylcholinesterase (pseudo) found? (3)
|
1. Blood plasma
2. Liver 3. Glial cells |
|
|
What is the neurotransmitter released at Adrenergic synapses?
|
Neuroepinephrine (mostly found in SNS)
|
|
|
Where is NE converted to Epi?
|
Adrenal Medulla
|
|
|
What is the rate-limiting step in the Adrenergic transmission pathway?
|
Conversion of Tyrosine -> L-DOPA = Tyrosine Hydroxylase
|
|
|
List the sequence of the production of NE and Epi
|
Tyrosine -> L-Dopa -> Dopa -> NE -> Epi
The Lazy Dog Naps Easily |
|
|
What converted L-Dopa to Dopamine?
|
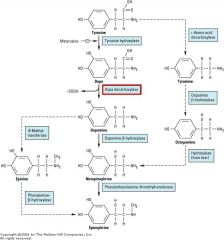
Dopa Decarboxylase
|
|
|
Tyrosine analog that inhibits Tyrosine Hydroxylase convesion of Tyrosine to L-DOPA
|

Me-tyrosine
|
|
|
What enzyme converts Dopamine to NE?
|
Dopamine-beta-hyrdoxylase
|
|
|
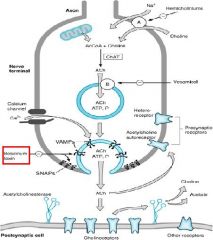
What inhibits the storage of NE in vesicles by inhibiting VAMP?
What blocks the release of NE from the Presynaptic neuron? What could these be used for clinically? |

Re-serpine
Guan-ethidine & Bretyl-ium HTN |
|
|
What is Uptake 1 in the Adrenergic pathway?
What is Uptake 2 in the Adrenergic pathway? |
transports catecholamines into the Presynaptic neuron
uptake of catecholamines in the Postsynaptic neuron |
|
|
What blocks the Uptake 1 mechanism in Adrenergic transmission? What is the effect?
|
Cocaine & other Tricyclic Antidepressants (TCA's)
increases transmitter activity |
|
|
What 2 drugs enter via Uptake 1 mechanism and displace NE from vesicles (action does not require exocytosis)?
|
Tyramine
Amphetamines |
|
|
What is the name of the transporter that sequesters NE into vesicles in the Adrenergic pathway?
|
VAMP
|
|
|
What is the major secretory product of the Adrenal Medulla?
What enzyme is responsible for this? |
Epinephrine
Phenyl-ethanol-amine-N-methyltransferase (PNMT) = converts NE -> Epi |
|
|
Enzyme in the Mitochondria of the nerve terminals of the Presynaptic neurons that metabolize NE & Epi
|
Monoamine Oxidase (MAO)
**metabolism is not primary mechanism for termination of action -- Uptake 1 is!! |
|
|
Enzyme in the cytoplasm of the Postsynaptic cells that metabolize NE and Epi
|
Catechol-O-MethyTransferase (COMT)
**metabolism is not primary mechanism for termination of action -- Uptake 1 is!! |
|
|
What are the subtypes of Cholinergic receptors?
|
1. Muscrarinic
2. Nicotinic |
|
|
What are the 2 types of Cholinergic receptors? What do they respond to?
|
Muscarinic & Nicotinic
ACh |
|
|
What type of receptors are Muscarinic receptors?
What type of receptors are Nicotinic receptors? |
G-protein coupled
Ligand activated Ion channels |
|
|
What are the 2 types of Adrenoceptors? What do they respond to?
|
Alpha- & Beta-adrenoceptors
Catecholamines (NE, Epi, dopamine) |
|
|
Where are Muscarinic receptors found?
|
on the target organs of the PSNS
-heart -smooth muscle **also found in Sweat Glands but is a Sympathetic neuron |
|
|
Where are Nicotinic Receptors found?
|
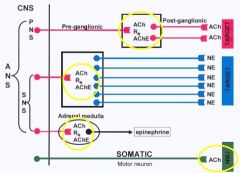
1. autonomic ganglia of SNS & PSNS
2. Neuromuscular jxn (Somatic) 3. Adrenal Medulla |
|
|
What transmitters do the "Nonadrenergic, Noncholinergic" neurons use?
Where are these neurons very important? |
Peptides, NO, & purine
GI and GU systems |
|
|
What provides the central integration of the ANS?
|
Midbrain, Medulla, Hypothalamus
-provide descending drive that impinges on the Presynaptic neurons of both SNS and PSNS -they receive info from the periphery from central inputs |
|
|
What are the main functions of the PSNS?
|
Energy conservation
-major underlying tone at most end organs (except VASCULATURE!!!) -slowing of heart & stimulate digestive activity |
|
|
The PSNS provides the underlying tone at most end organs except what?
|
Vasculature = under control by the SNS
|
|
|
What are the main functions of the SNS?
|
"Fight or Flight" = stress
-Cardiac stimulation -increased blood glucose -cutaneous vasoconstriction |
|
|
What is an important organ that does not receive DUAL INNERVATION?
|
Peripheral Vasculature = no innervation by PSNS
|
|
|
Explain how the PSNS has a "pseudo" activity on the Peripheral Vasculature
|
Peripheral Vasculatre DOES NOT have PSNS innervation, BUT:
-Endothelial cells have Muscarinic cholinoceptors (receptors used by PSNS on end organs) that can be activated by ACh circulating in blood -evokes production & release of NO -> Vasodilation (Hypotension) |
|
|
What is the main variable that is controlled by the ANS in the Cardiovascular System?
|
Mean Arterial Pressure = average arterial pressure with respect to time
|
|
|
What is the major determinant of Mean Arterial Pressure? What else controls it?
|
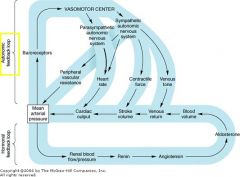
Peripheral resistance determined by SNS
Others: -PSNS controls heart rate (slows down) and CO -SNS influences contractility of heart |
|
|
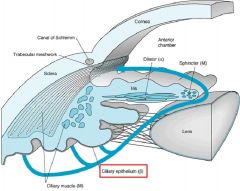
What are the 3 different muscles in the Eye? What are they controlled by?
|
1. Pupillary dilator = iris = Adrenergic receptors cause contraction (SNS) = pupil dilates
2. Pupillary Constrictor -iris- Muscarinic receptors contract (PSNS) 3. Ciliary muscle = Muscarinic receptors contract (PSNS) = contraction of the ciliary muscles reduces the size of the ciliary body, lessening the tension on the lens and allowing it to assume a more sperical shape for close vision |
|
|
What is the innervation of the Secretory Epithelium of the Ciliary Body in the eye?
How does the fluid drain? |
Adrenergic receptors = SNS = Beta
- forms aqueous humor Canal of Schlemm (in ciliary body) |
|
|
What actions would Muscarinic Agonists produce in the Eye?
|
1. contraction of the Circular Pupillary Constrictor muscle = Miosis = Small pupil
2. Contraction of the Ciliary Muscle = accommodation = close viewing 3. Outflow of Aqueous Humor due to contraction of Ciliary Muscle -> tension on trabecular meshwork -> opens pores -> outflow of aqueous humor **all due to PSNS |
|
|
What effects would Alpha adrenoceptor Agonists have on the Eye?
|
contract Radial Pupillary Dilator Muscles = Mydriasis = pupil becomes larger
**SNS |
|
|
What effects would Beta-adrenoceptor Agonists have on the Eye?
|
act on Ciliary Epithelium to secrete Aqueous Humor
**Beta-blockers reduce secretion = useful in Glaucoma |
|
|
Explain the ways in which Presynaptic neurons may be regulated
|
Autoreceptors on Presynaptic neuron terminals
-usually inhibit vesicular release -Alpha2 receptors on Preganlionic SNS neurons (presynaptic) can be inhibited by NE released from the Postsynaptic neuron |
|
|
What does it mean when we say that "Presynaptic receptors can have Heterologous action"?
|
a Presynaptic receptor could gate the release of the transmitter that binds to it
-Presynaptic receptor that responds to norepinepherine could be gating norepinepherine release in a Presynaptic sympathetic neuron |
|
|
What would a lack of activation on Postsynaptic neurons cause?
|
1. Denervation Supersensitivity
2. Up-regulation of Postsynaptic receptor number &/or affinity |
|
|
What would persistant activation of Postsynaptic neurons cause?
|
1. Desensitization or Tachyphylaxis (rapidly decreasing response to a drug following administration of the initial doses)
2. Down-regulation of receptor #, affinity, or coupling 3. Internalization or Phosphorylation of receptor proteins |

