![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
68 Cards in this Set
- Front
- Back
|
Principal androgen in men?
What secretes 95% of it? What secretes 5% of it? |
Testosterone
Leydig cells Adrenal Cortex |
|
|
What are the plasma levels of Testosterone in males after puberty?
When do they start to decline? |
0.6 mg/dL
after age 50 |
|
|
What is the level of Testosterone in females?
What 2 sites secrete Testosterone in females? |
.03 mg/dL (vs. 0.6 in males)
Adrenal Cortex & Corpus Luteum |
|
|
What are 2 weak androgens secreted along with Testosterone in men?
What is their precursor? |
Androstenedione & De-hydro-epi-androsterone (DHEA)
|
|
|
In target tissues, Testosterone is converted into active and inactive metabolites...what are the 2 ACTIVE metabolites?
Which is the major active androgen in most tissues? |
1. Dihydro-testosterone
2. Estradiol Dihydrotestosterone |
|
|
In the Liver, Testosterone is metabolized into what 2 INACTIVE METABOLITES?
|
1. Andro-sterone
2. Etio-cholan-olone |
|
|
List the changes that both Testosterone and Dihydrotestosterone cause at PUBERTY
|
1. general GROWTH-promoting properties
2. Penile & Scrotal growth 3. Thicker and oilier skin with more SEBACEOUS glands 4. appearance of pubic, axillary, and beard hair 5. Laryngeal growth, thicker vocal cords = lower-pitched voice 6. Accelerated Skeletal growth & Epiphysial closure 7. Growth of Prostate and Seminal Vesicles 8. Stimulating and maintaining Male Sexual fxn |
|
|
List the 2 changes produced by Testosterone & Dihydrotestosterone in EARLY ADULTHOOD & MIDLIFE
|
1. gradual development of MALE PATTERN BALDNESS = begins with recession of hair at temples & vertex
2. development of BENIGN PROSTATIC HYPERPLASIA or PROSTATIC CANCER |
|
|
Serum Testosterone declines gradually as men age so that by age 80 free testosterone concentration is about ____% of that at age 20
|
40%
**may be related to decreases in energy, libido, muscle mass/strength, and bone mineral density |
|
|
Why is Oral Testosterone ineffective?
|
b/c it is catabolized in the liver
|
|
|
What type of preparations of Testosterone are able to bypass hepatic catabolism and are injected IM every 2-4 wks in Hypogonadal males
|
synthetic preps as LIPOPHILIC ESTERS dissolved in OIL
|
|
|
List 3 esters that are used to prolong and have greater activity release of free testosterone at injection sites
|
Propionate
Enan-thate Cypio-nate **are not Androgens themselves but help in the slow release of Testosterone |
|
|
What are the 2 uses of Synthetic Androgens?
|
1. Anabolic effects (but increase in muscle strength is ALWAYS accompanied by adverse effects)
2. treating Testosterone deficiency |
|
|
What do large doses of Synthetic Androgens cause in Adult Males?
|
suppress Gonadotropin secretion ➡ testicular atrophy
|
|
|
What can happen if Synthetic Androgens are given to women?
|
develop Secondary Male characteristics
|
|
|
What product is reduced in the urine due to taking Synthetic Androgens? What is the cause?
|
Urinary Nitrogen
Increased protein synthesis or decreased protein breakdown |
|
|
When would Synthetic Androgens be used in boys?
|
as a growth stimulator in boys with delayed puberty
|
|
|
List 5 uses of Synthetic Androgens in treating women
|
1. Postpartum breast engorgement
2. Endometriosis 3. Endometrial bleeding (& to enhance libido) after menopause 4. Postmenopausal Osteoporosis (alone or combined with estrogens) 5. Chemotherapy of Premenopausal breast tumors |
|
|
Give 3 situations in which Synthetic Androgens would be used as a protein anabolic agent to reverse protein loss
|
1. after trauma
2. after surgery 3. prolonged immobilization |
|
|
What are the possible adverse effects of Anabolic Steroid abuse?
|
1. suppress endogenous Testosterone
2. suppress Sperm production 3. may cause Gynecomastia 4. may cause Virilization |
|
|
What are 2 possible adverse effects if Synthetic Androgens are given to elderly males to replace low androgen levels
|
1. may worsen Benign Prostatic Hyperplasia
2. increase risk of Prostate CA |
|
|
What are the adverse effects of Synthetic Androgens in Women?
|
1. Acne
2. Hirsutism 3. Amenorrhea 4. Clitoral enlargement 5. deep voice 6. ALTER SERUM LIPIDS TO INCREASE ATHEROSCLEROTIC SUSCEPTIBILITY |
|
|
What are the adverse effects of Synthetic Androgens in Men? (6)
|
1. Acne (nathan)
2. Sleep apnea 3. Erythrocytosis 4. Gynecomastia 5. Azoospermia 6. decreased testicular size = due to decreased Gonadotropin secretion (FSH/LH) |
|
|
List 2 Gonadotropin-releasing hormone (GnRH) analogs used for gonadal suppression in treatment of Prostatic Cancer
|
Gose-relin
Leu-prolide |
|
|
Antifungal imidazole used to inhibit adrenal and gonadal steroid synthesis to treat Cushing's disease (adrenal) and Prostate Cancer (gonadal)
What is it's mechanism of action? |
Ketoconazole
inhibits Desmolase |
|
|
5-alpha-reductase inhibitor that reduces conversion of Testosterone to Dihydrotestosterone
|
Fin-asteride
|
|
|
What is Finasteride used to treat?
|
Benign Prostatic Hyperplasia
**5-alpha-reductase inhibitor |
|
|
3 non-steroidal competitive inhibitors of androgens (anti-androgens) used to treat PROSTATIC CARCINOMA
|
F-lutamide
Bica-lutamide Ni-lutamide |
|
|
Aldosterone antagonist used clinically as a potassium-sparing diuretic, also lowers 5-alpha-reductase activity to lower plasma levels of Testosterone & Androstenedione
|
Spironolactone
|
|
|
Cottonseed derivative used as a male contraceptive in China
|
Gossypol
|
|
|
2 major constituents of Bone
|
Calcium & Phosphate
**bones contains 98% of total body Ca++; 85% of total body Phosphate |
|
|
Which has higher intestinal absorption, phosphate or calcium?
|
Phosphate
|
|
|
Larger amounts of ______ are present in bone and reabsorbed by the Kidneys
|
Calcium
**more calcium is present in bone; more calcium is reabsorbed in the kidney as compared to Phosphate |
|
|
Calcium enters the body only through the __1__ resulting in daily absorption of about __2__. An obligatory loss of 150 mg/day occurs in __3__ & __4__ secretions, and in sloughed __5__ cells
|
1. intestine
2. 300 mg 3. mucus 4. biliary 5. intestinal |
|
|
What accounts for a fecal loss of 650 mg/day of Calcium?
|
1. mucosal + biliary secretions & sloughed intestinal cells = 150 mg
2. redisual 500 mg remaining from the unabsorbed intake (800 mg intake; 300 is absorbed) |
|
|
What is urinary excretion of Ca++ determined by?
|
Tubular reabsorption
-highly efficient = more than 98% of the 9 g filered daily is reabsorbed |
|
|
What are the prinipal regulators of Calcium bone homeostasis?
|
1. PTH
2. Vitamin D |
|
|
What is the primary function of PTH?
|
to keep Ca++ concentration in the extracellular fluid constant
|
|
|
What is the plasma half-life of PTH?
How is it removed from the body? |
2-5 min
hepatic and renal clearance |
|
|
What influences the secretion of PTH from the parathyroid gland?
|
low Ca++ = secretion of PTH
high Ca++ = inhibition of PTH secretion |
|
|
In what 2 ways does PTH increase the plasma concentration of Ca++
|
1. increase Bone resorption = increase Ca++ mobilization
2. increase reabsorption of Ca++ in Kidneys |
|
|
List the 6 preparations of Vitamine D
|
Calci-fed-iol
Calci-triol Chole-calci-ferol **Dihydro-tachy-sterol** Doxy-calci-ferol Ergo-calci-ferol |
|
|
What are the sources of Vitamin D?
|
1. formed in skin by UV radiation
2. Plants |
|
|
Intrinsic and dietary forms of Vitamin D are inactive precursors that have to be converted to active metabolites of which _______ is the most active
|
Calci-triol
|
|
|
In what 3 ways does Vitamin D regulate Ca++ homeostasis?
|
1. increase bone resorption
2. kidneys to increase tubular reabsorption 3. small intestines to increase Ca++ absorption |
|
|
What does deficiency of Vitamin D in children cause?
In adults? |
Children = Rckets
Adults = Osteomalacia |
|
|
The only regulator affecting intestinal Ca++ absorption
|
Vitamin D
|
|
|
Hormone secreted by Parafollicular cells (C cells) in the Thyroid when serum Ca++ is high
|
Calcitonin
|
|
|
What is the action of Calcitonin? How does it achieve it?
|
Lowers serum Ca++
inhibits Osteoclastic bone resorption; reduces tubular reabsorption of Ca++ & phosphate |
|
|
What 3 diseases is Calcitonin used to treat?
|
1. Paget's disease = excessive breakdown & formation of bone tissue
2. Hypercalcemia 3. Osteoporosis |
|
|
How do Glucocorticoids affect Ca++ homeostasis? (2)
|
1. antagonize Vitamin D-stimulated intestinal Ca++ absorption
2. stimulate renal Ca++ excretion **ultimately cause decreased body Calcium |
|
|
What do Glucocorticoids block the synthesis of in bone?
|
Collagen synthesis
|
|
|
What 3 conditions are Glucocorticoids used to treat in regards to Mineral Homeostasis?
|
1. to reverse Hypercalemia in Lymphomas
2. Sarcoidosis (has hypercalcemia due to elevated conversion of vitamin D to its active form in Epithelioid macrophages) 3. Vitamin D intoxication |
|
|
How do Estrogens prevent accelerated bone loss?
|
act by decreasing PTH-induced bone resorption
|
|
|
Are Estrogens more effective in preventing or restoring bone loss?
|
PREVENTING
|
|
|
Used for treatment or prevention of Postmenopausal Osteoporosis
|
Estrogens
|
|
|
What is the ending for all Pyrophosphate analogs of Bisphosphonates?
|
-DRONATE
|
|
|
What is the mechanism of action of the -DRONATE's?
|
Bisphosphonate pyrophosphate analogs
Act by retarding formation & dissolution of hydroxyapatite crystals in the skeleton = decrease bone resorption |
|
|
What is the adverse effect of the -Dronate's?
|
Gastric irritation
**< 10% of oral doses is absorbed |
|
|
What are the -Dronate's used clinically to treat?
|
1. Hypercalcemia associated with malignancy (bone metastases)
2. Osteoporosis 3. Syndromes of ectopic calcification 4. Paget's disease = enlarged & deformed bones |
|
|
Diuretic used to treat HypercalciURIA
|
Thiazides
|
|
|
Explain why Thiazides are used to treat HypercalciURIA
|
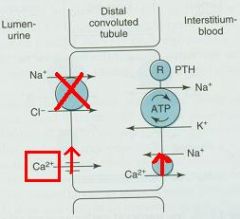
1. block sodium reabsorption in distal tubule
2. increase Calcium-sodium exchange in basolateral membrane 3. Increase Ca++ reabsorption = reduced renal excretion |
|
|
Cytotoxic antibiotic used for treatment of Paget's disease and Hypercalcemia
|
Plica-mycin (Mithramycin)
|
|
|
Define Osteoporosis
Who is it most common in? |
abnormal bone loss predisposing to fractures
Postmenopausal women (but also occurs in older men) |
|
|
Aside from Menopause and aging, what other 5 things can Osteoporosis result from?
|
1. Chronic treatment with Glucocorticoids
2. Endocrine disorders such as Thyrotoxicosis or Hyperparathyroidism 3. Malabsorption syndrome 4. Alcohol abuse 5. Idiopathic |
|
|
What is Postmenopausal Osteoporosis due to?
|
Estrogen deficiency
|
|
|
Partial Estrogen Agonist used to prevent Postmenopausal Osteoporosis BUT does NOT affect Endometrium or Breast
|
Ralox-ifene
|
|
|
What is idiopathic Osteoporosis in Elderly men usually treated with?
|
Vitamin D & dietary Calcium
|

