![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
The Thyroid gland maintains metabolic homeostasis by regulating these 3 things
|
1. Growth & development
2. Body temperature 3. Energy levels |
|
|
What hormones are involved in accomplishing the functions of the thyroid gland?
|
1. Triiodothyronine = T3
2. Tetraiodothyronine = T4 = Thyroxine |
|
|
What is the molecular composition of T3?
|
one Monoiodotyrosine (MIT) + one Diiodotyrosine (DIT)
|
|
|
What is the molecular composition of T4?
|
2 Diiodotyrosine (DIT)
|
|
|
What is the Thyroglobulin ratio of T3 and T4?
|
1 T3 molecule for every 5 T4 molecules
or T3:T4 = 1:5 |
|
|
How much Iodide (I-) does the Thyroid gland remove from the extracellular pool each day?
|
75 mg
|
|
|
Thyroid hormone synthesis:
-Iodide is taken up by Thyroid follicular cells via a membrane __1__ transporter -Iodide is coupled to __2__ residues on the __3__ molecule (=organification) -formation of __4__ &__5__ -__6__ catalyzes coupling of 2 DIT molecules to form T4 or one molecule each of MIT and DIT to form T3 -Thyroglobulin is stored as __7__ in the lumen -__8__ signals secretion to hydrolyze Thyroglobulin to free MIT, DIT, T3 & T4 |
1. Na+/I-
2. tyrosine 3. thyroglobulin 4. MIT = monoiodotyrosine 5. DIT = diiodotyrosine 6. Thyroid peroxidase 7. colloid 8. TSH |
|
|
Plasma T3 and T4 are REVERSIBLY bound to __1__
Why is most of the thyroid hormone that is released T4? |
Thyroxine-binding globulin
T4:T3 ratio in Thyroglobulin is 5:1 |
|
|
The peripheral metabolism of T4 is mainly by what mechanism?
What 2 things does it form? |
Deiodination
1. T3 = 3-4 times more potent than T4 2. rT3 = metabolically inactive |
|
|
Give 2 reasons why the total serum levels of T4 are higher than T3
|
1. more of it is released (5:1 ratio)
2. metabolic clearance of T3 is much higher |
|
-
|
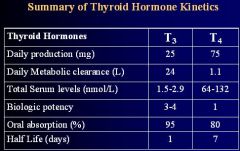
Just know which one is higher and which one is lower
|
|
|
Explain Hypothalamic-Pituitary-Thyroid Regulation
|

1. Paraventricular nuclei in the Hypothalamus secrete TRH
2. TRH stimulates the Anterior Pituitary to release TSH 3. TSH acts on Thyroid to release T3 & T4 4. T3 & T4 act by negative feedback to inhibit formation of TRH & TSH |
|
|
Describe the Autoregulation within the Thyroid gland
|
Modifies Thyroid hormone synthesis through blood iodine levels
-high iodine levels → inhibit iodide organification → reduced T3/T4 synthesis → hypothyroidism **counterintuitive b/c the same substance, iodine, has opposite effects and the effects depend on the concentration --> higher plasma Iodine = lower T3/T4 |
|
|
Explain Grave's Disease
|

Autoantibody to the TSH receptor in the Thyroid causes increased T3/T4 release
**TRH and TSH levels will be decreased due to negative feedback of T3/T4 |
|
|
Explain Hashimoto's Disease
|
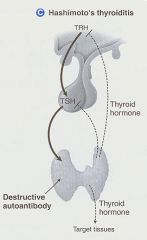
Destructive Autoantibody causing decreased T3/T4 release
**TRH and TSH will be elevated b/c T3/T4 are not present for negative feedback |
|
|
Thyroid hormone receptors located in all cells are monomers that interact with ___1____ to form heterodimers
In the absence of T3 the heterodimer associates with a __2__ complex that binds to DNA to __3__ In the presence of T3 the __4__ dissociates, while __5__ form to stimulate __6__ |
1. Retinoic Acid X Receptor (RXR)
2. co-repressor 3. inhibit gene expression 4. co-repressor 5. coactivators 6. Gene expression ** = T3 stimulates gene expression |
|
|
T3 receptors belong to a superfamily of __1__ receptors (c-erb which includes receptors for __2__ and __3__)
|
1. nuclear
2. steroid hormones 3. Vitamins A & D |
|
|
Describe the Thyroid Hormone Mechanism of action (6 steps)
|
1. T3/T4 are dissociated from thyroid-binding proteins
2. T3/T4 enter target cells by diffusion or transport 3. in cytoplasm 5'-deiodinase converts T4 to T3 4. T3 enters the nucleus to bind to T3 receptors 5. increased formation of RNA 6. increased protein synthesis |
|
|
Circulating iodine is 95% __1__ and 5% __2__
|
1. organic iodine
2. iodide = I- |
|
|
Of the circulating iodine in the Organic form 95% is __1__ while the other 5% is __2__
|
1. T4
2. T3 |
|
|
What protects circulating T3 and T4?
|
Thyroxin binding globulin (TGB)
*free or unbound hormones are minimal *only the unbound hormones have metabolic activity |
|
|
In peripheral tissues what converts T4 to T3?
What are the 3 main organs that do this? |
Iodothyronine 5'-deiodinase
Liver, Thyroid, Kidneys |
|
|
What is the active hormone in most target tissues?
|
T3
|
|
|
List the 4 main effects of Thyroid Hormone
|
1. Nervous, musculoskeletal, and reproductive issues
2. Calorigenic effect 3. Sympathetic hyperactivity 4. Metabolic effects |
|
|
List the Nervous, musculoskeletal, and reproductive effects Thyroid hormone has
|
Nervousness
Emotional lability Muscle weakness & fatigue Osteoporosis Menstrual irregularities |
|
|
Describe the Calorigenic effect thyroid hormone causes
|
increased Oxygen consumption
Sweating |
|
|
Describe the Sympathetic hyperactivity effects Thyroid Hormone causes
|
Up-regulates B1-adrenergic receptors in the heart
-tachycardia -increased stroke volume & CO -high-output heart failure -arrythmia -angina **may want to use B-adrenergic blocking agent (propranolol) as an adjunct treatment for hyperthyroidism |
|
|
Describe the Metabolic effects Thyroid Hormone causes
|
Decreased Cholesterol and TG's
Increased BMR Hyperglycemia Appetite |
|
|
Preparation of choice for Replacement and Suppression therapy for Hypothyroidism
|
Synthetic Levothyroxine (T4)
|
|
|
Why is Levothyroxine the preparation of choice for replacement therapy of Hypothyroidism?
|
1. Stable
2. Uniform content 3. Low cost 4. Long half-life (7 days) 5. conversion to produce both T3 and T4 |
|
|
Thyroid preparation though inexpensive, is not recommended for replacement therapy b/c of its antigenicity, instability, and variable hormone content
|
Dessicated Thyroid
|
|
|
Thyroid replacement that is 3-4 times more active than Levothyroxine but is not recommended for routine replacement therapy
|
Liothyronine (T3)
|
|
|
Why is Liothyronine not recommended for routine thyroid replacement therapy?
|
1. High cost
2. Shorter half-life (24 hrs vs. 7 days) 3. **Cardiotoxicity** potential |
|
|
4:1 combination of synthetic T4 and T3, is also expensive with the same disadvantages as Liothyronine
|
Liotrix
|
|
|
List the 2 Thioamides (anti-thyroid drugs)
|
Methimazole
Propylthiouracil |
|
|
Where do the 2 Thioamides accumulate readily?
|
Thyroid gland for treatment of Thyrotoxicosis
|
|
|
Thioamide that is 10X more active than the other
|
Methim-azole
|
|
|
What are the plasma half-lives for the 2 Thioamides?
|
Methim-azole = 6 hrs
Propyl-thio-uracil = 1.5 hrs |
|
|
How long does it take for the Thioamides to have an effect?
|
Slow onset!!! ➡ 3-4 weeks to deplete T4 stores
|
|
|
What are the mechanisms of action of the Thioamides? (3)
|
1. Inhibits peroxidase rxns = blocks Iodine Organification (conversion of I- to I2)
2. blocks Iodotyrosine coupling 3. Inhibit peripheral deiodination of T3 and T4 ***Mechanism 1 is the major action |
|
|
What is the most common adverse effect of the Thioamides?
|

Maculopapular pruritic rash
|
|
|
What are the rare adverse effects of the Thioamides?
|
Urticarial rash, vasculitis, arthralgia, lupus-like rxn, jaundice, hepatitis, hypothrombinemia
|
|
|
What is the most dangerous adverse effect of the Thioamides?
|
Agranulocytosis
|
|
|
What 2 mechanisms of Potassium Iodides render them effective in Hyperthyroidism treatment?
|
1. inhibition of hormone release by reducing Thyroglobulin proteolysis
2. decrease the size and vascularity of the Hyperplastic gland |
|
|
With Iodide treatment thyrotoxic symptoms improve within __1__, but should not be used alone b/c the gland "escapes" from iodide block after __2__
|
1. 2-7 days
2. 2-8 weeks |
|
|
Why should chronic use of Iodides to treat Hyperthyroidism not be used in pregnancy?
|
Iodide crosses the placenta and could cause Fetal Goiter
|
|
|
What are 4 advantages of Iodide treatment for Hyperthyroidism?
|
1. simplicity
2. inexpensive 3. relatively nontoxic 4. Absence of glandular destruction |
|
|
List the adverse rxns of Iodide treatment
|

1. Acneiform rash
2. Swollen salivary glands 3. Mucous membrane ulceration 4. Conjunctivitis 5. Rhinorrhea 6. Metallic taste 7. Drug fever 8. Bleeding disorders 9. Anaphylaxis |
|
|
What are the disadvantages of Potassium Iodide treatment? (4)
|
1. "escape"
2. Aggravation of Thyrotoxicosis 3. Allergic rxns 4. Increased intraglandular iodine which can delay the onset of Thioamide therapy or prevent use of radioactive iodine therapy for several weeks |
|
|
The only radioactive isotope used for treatment of Thyrotoxicosis
|
Radioactive Iodine
|
|
|
How is RAI administered?
|
Oral solution
-RAI is rapidly absorbed and concentrated in the Thyroid gland |
|
|
What becomes evident within weeks after Radioactive Iodine treatment?
|
Thyroid parenchymal destruction
-epithelial swelling -necrosis -follicular disruption -edema -Leukocyte infiltration |
|
|
What does the therapeutic effect of RAI depend on?
|
Emission of Beta rays
-penetration range of 400-2000 micrometers -effective half-life of 5 days |
|
|
What are 4 advantages of RAI?
|
1. easy administration = oral solution
2. Effectiveness 3. Low expense 4. Absense of pain |
|
|
What is the major disadvantage of RAI?
|
induction of Hypothyroidism
|
|
|
What is the main contraindication of RAI?
|
Pregnancy b/c RAI crosses the placenta and is also excreted in Breast Milk
|
|
|
What is the mechanism of action of the Anion Inhibitors (Perchlorate, Pertechnetate, Thiocyanate)?
|
competitively inhibit the iodide transport mechanism and therefore block Iodide uptake
*effectiveness is unpredictable |
|
|
List 3 Anion Inhibitors
|
1. Thio-cyanate
2. Per-chlorate 3. Per-tech-netate |
|
|
Anion Inhibitor that is no longer used clinically because it causes Aplastic Anemia
|
Potassium Perchlorate
|
|
|
Though not FDA approved these act by inhibiting conversion of T4 to T3 in the liver, kidney, pituitary, and brain
|
Iodinated Contrast media
-Ipodate = by mouth -Dia-triz-oate = IV |
|
|
Since many symptoms of Thyrotoxicosis result from sympathetic hyperactivity, what have also been used for treatment?
|
B-adrenergic blockers or Guan-ethi-dine
|

