![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
107 Cards in this Set
- Front
- Back
|
Periodontium |
peri - around; odonotos - tooth functional tissues that surround the teeth and attaches them to the jaw |
|
|
Gingiva |
tissues that cover the cervical portions of the teeth and the alveolar process |
|
|
Periodontal Ligament |
(PDL) fibers that surround the root of the tooth; attach to bone & cementum |
|
|
Cementum |
thin layer of mineralized tissue that covers the root of the tooth |
|
|
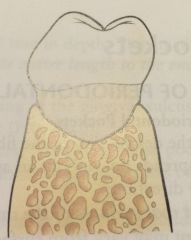
Alveolar Bone |
bone that surrounds the roots of the teeth |
|
|
Gingival Margin |
thin rounded edge of the free gingiva |
|
|
Alveolar Mucosa |
dark red in color, apical boundary |
|
|
Free Gingival Groove |
shallow linear depression that separates the free and attached gingiva |
|
|
Mucogingival Junction |
boundary between attached gingiva and alveolar mucosa |
|
|
Free Gingiva |
unattached portion that surrounds the tooth in the region of the CEJ |
|
|
Attached Gingiva |
tightly connected to the cementum on the cervical third of the root and to the periosteum of the alveolar bone |
|
|
Interdental Gingiva |
fills interdental embrasure between two adjacent teeth |
|
|
Stippling |
may or may not be apparent in healthy tissue |
|
|
Col |
valley like depression in the portion of the interdental gingiva that lies directly apical to the contact area |
|
|
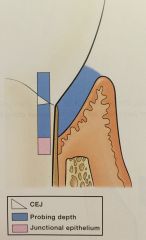
Gingival Sulcus |
space between the free gingiva and the tooth surface |
|
|
Gingival Crevicular Fluid |
seeps from the underlying connective tissue into the sulcular space |
|
|
Alveolar Process |
(Alveolar Bone) bone of the upper or lower jaw that surrounds and supports the roots of the teeth -60% inorganic material, 25% organic, 15% water |
|
|
Alveolar Bone Proper |
(Cribriform Plate) thin layer of bone that lines the pocket to surround the root of the tooth |
|
|
Cortical Bone |
compact bone that forms the hard, outside wall of the mandible or maxilla on the facial and lingual aspects - will not show up in a radiograph |
|
|
Alveolar Crest |
most coronal portion of the alveolar process - can be seen on radiograph |
|
|
Cancellous Bone |
(Spongy Bone) fills interior portion of the alveolar process - between cortical bones & alveolar bone proper |
|
|
Periosteum |
connective soft tissue covering the outer surface of bone; collagenous tissue and an inner layer of elastic fibers |
|
|
Innervation |
nerve supply to the periodontium |
|
|
Trigeminal Nerve |
sensory, motor and intermediate roots that attach directly to the brain - sensory of most of the skin of the front part of the face and head, teeth, oral cavity, maxillary sinus and nasal cavity |
|
|
Anastomose |
join together |
|
|
Lymphatic System |
network of lymph nodes connected by lymphatic vessels that play a role in the body's defense against infection |
|
|
Lymph Node |
bean-shaped structures located on either side of the head, neck, armpits and groin - filter & trap bacteria, fungi, viruses and other unwanted substances to safely eliminate them from the body |
|
|
Histology |
study of microscopic structures |
|
|
Tissue |
interconnected cells that perform a similar function within an organism |
|
|
Cells |
smallest structural unit of living matter capable of functioning indepenently |
|
|
Extracellular Matrix |
mesh like material that surrounds the cells |
|
|
Epithelial Tissue |
makes up the outer surface of the body (skin) and lines the body cavities such as the mouth and stomach |
|
|
Stratified Squamous Epithelium |
composed of flat cells arranged in several layers |
|
|
Basal Lamina |
underlies epithelium |
|
|
Keritinization |
cells on the surface become stronger and waterproof |
|
|
Keratinized Epithelial Cells |
have no nuclei and form a tough, resistant layer on the surface of the skin |
|
|
Nonkeritinized Epithelial Cells |
have nuclei and act as a cushion against mechanical stress and wear |
|
|
Connective Tissue |
fills spaces between the tissues and organs in the body |
|
|
Epithelial-Connective Tissue Interface |
is the boundary where the epithelial and connective tissues meet |
|
|
Epithelial Ridges |
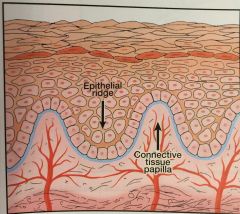
(Pete Pegs) deep extensions of epithelium that reach down into the connective tissue |
|
|
Connective Tissue Papillae |
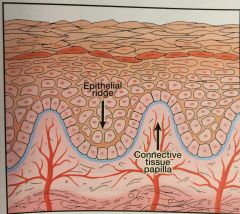
fingerlike extensions of connective tissue that extend up into epithelium |
|
|
Cell junctions |
cellular structures that mechanically attach a cell and its cytoskeleton to its neighboring cells or to the basal lamina |
|
|
Desmosome |
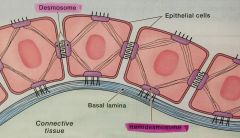
connects two neighboring epithelial cells |
|
|
Hemidesmosome |
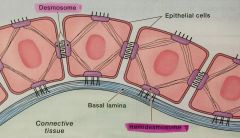
connects epithelial cells to the basal lamina |
|
|
Gingival Epithelium |
specialized stratified squamous epithelium that functions well in the wet environment of the oral cavity |
|
|
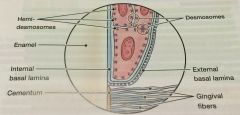
Oral Epithelium |
(OE) epithelium that faces the oral cavity - free gingiva, attached gingiva |
|
|
Sulcular Epithelium |
(SE) epithelium that faces the tooth surface without being in contact - sulcus |
|
|
Junctional Epithelium |
(JE) epithelium that attaches the gingiva to the tooth - base of the sulcus |
|
|
Parakeritinized |
partially keritinized |
|
|
Keratin |
tough, fibrous structural protein that occurs in the outer layer of the skin and the OE |
|
|
Gingival Crevicular Fluid |
slight in health and increases with disease |
|
|
Internal Basal Lamina |
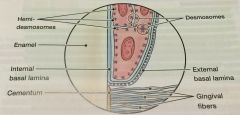
between epithelial cells of JE and the tooth surface |
|
|
External Basal Lamina |
between epithelial cells of the JE and the gingival connective tissue |
|
|
Supragingival Fiber Bundles |
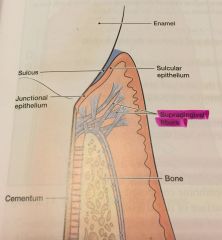
(gingival fibers) network of ropelike collagen fiber bundles in the gingival connective tissue - located coronal (above) the crest of the alveolar bone |
|
|
Collagen Fibers |
enable gingiva to form a rigid cuff around the tooth - hold gingival connective tissues together |
|
|
Dentogingival Unit |
JE and the gingival fibers |
|
|
PDL |
(Periodontal Ligament) fibrous connective tissue that surrounds the roots of teeth and joins the root cementum with the socket wall |
|
|
Fiber Bundles of PDL |
specialized connective tissue that surrounds the root of the tooth and connects it with alveolar bone |
|
|
Sharpey fibers |
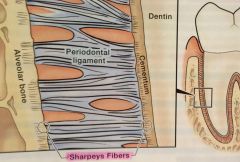
ends of periodontal ligament fibers that are embedded in the cementum and alveolar bone |
|
|
Cementum |
mineralized layer of connective tissue that covers the root of the tooth |
|
|
OMG |
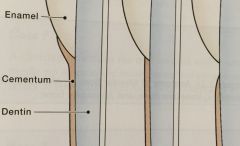
Overlap - 60% Meet - 30% Gap - 10% relationship of cementum to enamel at the CEJ |
|
|
Radiolucent |
easily penetrated by X-rays - appear dark gray to black |
|
|
Radiopaque |
absorb or resist the passage of X-rays - appear light gray or white |
|
|
Lamina Dura |
alveolar bone proper identified on radiographs |
|
|
Crestal Irregularities |
appearance of breaks or fuzziness instead of a nice clean line at the crease of the interdental alveolar bone |
|
|
Triangulation |
is the widening of the periodontal ligament space caused by the resorption of bone along either the medial or distal aspect of the interdental crestal bone |
|
|
Pathogenesis |
is the sequence of events that occur during the development of a disease or abnormal condition |
|
|
Gingivitis |
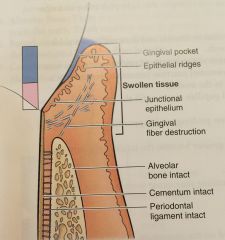
a bacterial infection that is confined to the gingiva - a type of periodontal disease |
|
|
Acute Gingivitis |
lasts for a short period of time - results in swollen gingiva |
|
|
Chronic Gingivitis |
lasts for months or years |
|
|
Reversible (Tissue Damage) |
damage in gingivitis is reversible - that is, with good patient self-care, the body can repair the damage |
|
|
Periodontitis |
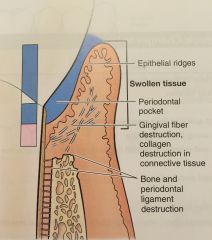
type of periodontal disease - apical migration of JE - loss of connective tissue - loss of alveolar bone |
|
|
Inflammation |
body's reaction to injury or invasion by disease-producing organisms - in periodontitis, this results in permanent destruction of the tissues of the periodontium (gingival connective tissue, PDL, alveolar bone) |
|
|
Alveolar Bone Loss |
resorption of alveolar bone as a result of periodontitis |
|
|
Horizontal Bone Loss |
most common pattern of bone loss |
|
|
Vertical Bone Loss |
less common pattern of bone loss |
|
|
Osseous Defects |
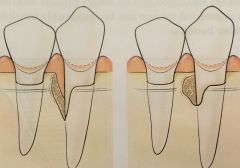
results from periodontitis, different types of defects in alveolar bone |
|
|
Infrabony Defects |
bone resorption occurs in an uneven, oblique direction, primarily affects one tooth |
|
|
Osseous Craters |
bowl-shaped defect in the interdental alveolar bone, with bone loss nearly equal on the roots of two adjacent teeth |
|
|
Furcation Involvement |
occurs on multi-rooted teeth when periodontal infection invades the area between and around the roots, resulting in a loss of alveolar bone between the roots of the teeth |
|
|
Attachment Loss |
the destruction of fibers and bone that support the teeth |
|
|
Disease Site |
an area of tissue diseased; may involve only a single surface, may involve several surfaces |
|
|
Inactive Disease Site |
a disease site that is stable, with the attachment level of the JE remaining the same over time |
|
|
Active Disease Site |
a disease site that shows continued apical migration of the JE over time |
|
|
Gingival Pocket |
deepening of the gingival sulcus as a result of swelling or enlargement of the gingival tissue |
|
|
Periodontal Pocket |
pathogenic deepening of the pocket |
|
|
Suprabony Pockets |
occur when there is horizontal bone loss |
|
|
Infrabony Pockets |
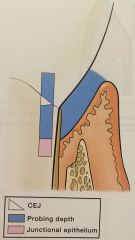
occur when there is vertical bone loss |
|
|
Classification |
systematic arrangement into groups or categories based on common attributes |
|
|
Periodontal Disease |
refers to inflammation of the periodontium gingivitis: limited to inflammation of the gingival tissues periodontitis: involves all the structures of the periodontium |
|
|
American Academy of Periodontology |
(AAP) initiated the currently accepted classification by organizing the International Workshop for a Classification of Periodontal Diseases and Conditions in 1999 |
|
|
Plaque-Induced Gingival Disease |
involving inflammation of the gingiva in response to bacteria located at the gingival margin; most common form of gingival disease |
|
|
Non-Plaque-Induced Gingival Disease |
caused by viral infections, fungal, skin diseases, allergic reactions, mechanical trauma; less common type |
|
|
Chronic Periodontitis |
most common form of periodontitis; bacterial infection within the supporting tissues of the teeth - destruction of PDL fibers and alveolar bone & pocket formation and/or recession of gingival margin |
|
|
Aggressive Periodontitis |
bacterial infection characterized by rapid attachment loss and less response to periodontal therapy - may be localized or generalized |
|
|
Periodontitis as a manifestation of systemic diseases |
Hematological (blood) Disorders: leukemia or acquired neutropenia Genetic Disorders: down syndrome or leukocyte adhesion deficiency syndrome |
|
|
Necrotizing Periodontal Diseases |
NUG: (Necrotizing Ulcerative Gingivitis) tissue necrosis that is limited to the gingival tissues, no attachment loss NUP: (Necrotizing Ulcerative Periodontitis) tissue necrosis combined with loss of attachment and alveolar bone loss |
|
|
Tissue Necrosis |
localized tissue death |
|
|
Periodontal Absess |
localized collection of pus that forms in circumscribed areas of the periodontal tissues |
|
|
Periodontitis associated with Endodontic lesions |
involves infection or death of the tissues of the dental pulp |
|
|
Epidemiology |
study of the health and disease within the total population and the risk factors that influence health and disease |
|
|
Prevalance |
number of all cases (both old and new) of a disease that can be identified within a specified population at a given point in time |
|
|
Incidence |
number of new disease cases in a population that occur over a given period of time |
|
|
Periodontal Pathogens |
bacteria that are capable of infecting the tissues of the periodontium |
|
|
Disease Progression |
in this context, means that disease gets worse |
|
|
Intermittent disease progression theory |
states that periodontal disease is characterized by periods of disease activity and inactivity |
|
|
Risk Factors |
factors that modify or amplify the likelihood of developing periodontal disease. - major established risks are specific baterial pathogens, cigarette smoking and diabetes mellitus |

