![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
225 Cards in this Set
- Front
- Back
|
Periodontium |
peri - around; odonotos - tooth functional tissues that surround the teeth and attaches them to the jaw |
|
|
Gingiva |
tissues that cover the cervical portions of the teeth and the alveolar process |
|
|
Periodontal Ligament |
(PDL) fibers that surround the root of the tooth; attach to bone & cementum |
|
|
Cementum |
thin layer of mineralized tissue that covers the root of the tooth |
|
|
Alveolar Bone |
bone that surrounds the roots of the teeth |
|
|
Gingival Margin |
thin rounded edge of the free gingiva |
|
|
Alveolar Mucosa |
dark red in color, apical boundary |
|
|
Free Gingival Groove |
shallow linear depression that separates the free and attached gingiva |
|
|
Mucogingival Junction |
boundary between attached gingiva and alveolar mucosa |
|
|
Free Gingiva |
unattached portion that surrounds the tooth in the region of the CEJ |
|
|
Attached Gingiva |
tightly connected to the cementum on the cervical third of the root and to the periosteum of the alveolar bone |
|
|
Interdental Gingiva |
fills interdental embrasure between two adjacent teeth |
|
|
Stippling |
may or may not be apparent in healthy tissue |
|
|
Col |
valley like depression in the portion of the interdental gingiva that lies directly apical to the contact area |
|
|
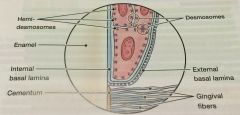
Gingival Sulcus |
space between the free gingiva and the tooth surface |
|
|
Gingival Crevicular Fluid |
seeps from the underlying connective tissue into the sulcular space |
|
|
Alveolar Process |
(Alveolar Bone) bone of the upper or lower jaw that surrounds and supports the roots of the teeth -60% inorganic material, 25% organic, 15% water |
|
|
Alveolar Bone Proper |
(Cribriform Plate) thin layer of bone that lines the pocket to surround the root of the tooth |
|
|
Cortical Bone |
compact bone that forms the hard, outside wall of the mandible or maxilla on the facial and lingual aspects - will not show up in a radiograph |
|
|
Alveolar Crest |
most coronal portion of the alveolar process - can be seen on radiograph |
|
|
Cancellous Bone |
(Spongy Bone) fills interior portion of the alveolar process - between cortical bones & alveolar bone proper |
|
|
Periosteum |
connective soft tissue covering the outer surface of bone; collagenous tissue and an inner layer of elastic fibers |
|
|
Innervation |
nerve supply to the periodontium |
|
|
Trigeminal Nerve |
sensory, motor and intermediate roots that attach directly to the brain - sensory of most of the skin of the front part of the face and head, teeth, oral cavity, maxillary sinus and nasal cavity |
|
|
Anastomose |
join together |
|
|
Lymphatic System |
network of lymph nodes connected by lymphatic vessels that play a role in the body's defense against infection |
|
|
Lymph Node |
bean-shaped structures located on either side of the head, neck, armpits and groin - filter & trap bacteria, fungi, viruses and other undated substances to safely eliminate them from the body |
|
|
Histology |
study of microscopic structures |
|
|
Tissue |
interconnected cells that perform a similar function within an organism |
|
|
Cells |
smallest structural unit of living matter capable of functioning indepenently |
|
|
Extracellular Matrix |
mesh like material that surrounds the cells |
|
|
Epithelial Tissue |
makes up the outer surface of the body (skin) and lines the body cavities such as the mouth and stomach |
|
|
Stratified Squamous Epithelium |
composed of flat cells arranged in several layers |
|
|
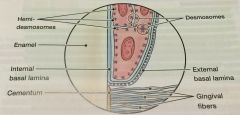
Basal Lamina |
underlies epithelium |
|
|
Keritinization |
cells on the surface become stronger and waterproof |
|
|
Keratinized Epithelial Cells |
have no nuclei and form a tough, resistant layer on the surface of the skin |
|
|
Nonkeritinized Epithelial Cells |
have nuclei and act as a cushion against mechanical stress and wear |
|
|
Connective Tissue |
fills spaces between the tissues and organs in the body |
|
|
Epithelial-Connective Tissue Interface |
is the boundary where the epithelial and connective tissues meet |
|
|
Epithelial Ridges |
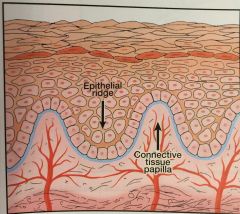
(Pete Pegs) deep extensions of epithelium that reach down into the connective tissue |
|
|
Connective Tissue Papillae |
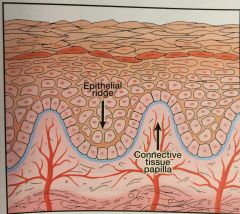
fingerlike extensions of connective tissue that extend up into epithelium |
|
|
Cell junctions |
cellular structures that mechanically attach a cell and its cytoskeleton to its neighboring cells or to the basal lamina |
|
|
Desmosome |
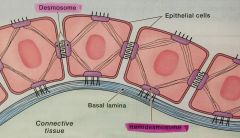
connects two neighboring epithelial cells |
|
|
Hemidesmosome |
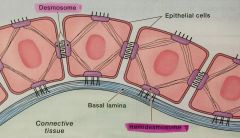
connects epithelial cells to the basal lamina |
|
|
Gingival Epithelium |
specialized stratified squamous epithelium that functions will in the wet environment of the oral cavity |
|
|
Oral Epithelium |
(OE) epithelium that faces the oral cavity - free gingiva, attached gingiva |
|
|
Sulcular Epithelium |
(SE) epithelium that faces the tooth surface without being in contact - sulcus |
|
|
Junctional Epithelium |
(JE) epithelium that attaches the gingiva to the tooth - base of the sulcus |
|
|
Parakeritinized |
partially keritinized |
|
|
Keratin |
tough, fibrous structural protein that occurs in the outer layer of the skin and the OE |
|
|
Gingival Crevicular Fluid |
slight in health and increases with disease |
|
|
Internal Basal Lamina |
between epithelial cells of JE and the tooth surface |
|
|
External Basal Lamina |
between epithelial cells of the JE and the gingival connective tissue |
|
|
Supragingival Fiber Bundles |
(gingival fibers) network of ropelike collagen fiber bundles in the gingival connective tissue - located coronal (above) the crest of the alveolar bone |
|
|
Collagen Fibers |
enable gingiva to form a rigid cuff around the tooth - hold gingival connective tissues together |
|
|
Dentogingival Unit |
JE and the gingival fibers |
|
|
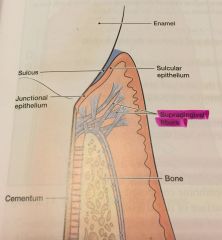
PDL |
(Periodontal Ligament) fibrous connective tissue that surrounds the roots of teeth and joins the root cementum with the socket wall |
|
|
Fiber Bundles of PDL |
specialized connective tissue that surrounds the root of the tooth and connects it with alveolar bone |
|
|
Sharpey fibers |
ends of periodontal ligament fibers that are embedded in the cementum and alveolar bone |
|
|
Cementum |
mineralized layer of connective tissue that covers the root of the tooth |
|
|
OMG |
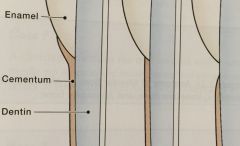
Overlap - 60% Meet - 30% Gap - 10% relationship of cementum to enamel at the CEJ |
|
|
Radiolucent |
easily penetrated by X-rays - appear dark gray to black |
|
|
Radiopaque |
absorb or resist the passage of X-rays - appear light gray or white |
|
|
Lamina Dura |
alveolar bone proper identified on radiographs |
|
|
Crestal Irregularities |
appearance of breaks or fuzziness instead of a nice clean line at the crease of the interdental alveolar bone |
|
|
Triangulation |
is the widening of the periodontal ligament space caused by the resorption of bone along either the medial or distal aspect of the interdental crestal bone |
|
|
Alveolus |
bony socket, cavity in the alveolar bone that houses root of a tooth |
|
|
Pathogenesis |
sequence of events that occur during the development of a disease or abnormal condition
exist in 3 basic states 1.) health 2.) gingivitis 3.) periodontitis |
|
|
Gingivitis |
a type of periodontal disease characterized by changes in the color, contour, and consistency of gingival tissue |
|
|
Acute Gingivitis |
gingivitis that lasts for short period of time
often characterized by fluid in the gingival connective tissues that results in swollen gingiva |
|
|
Chronic Ginigivitis |
gingivitis that lasts for months or years
fibrotic (leathery) consistency |
|
|
Reversible tissue damage |
the tissue damage in gingivitis is reversible - with good patient self-care, the body can repair the damage |
|
|
Periodontitis |
a type of periodontal disease that is characterized by 1.) apical migration of junctional epithelium 2.) loss of connective tissue attachment 3.) loss of alveolar bone |
|
|
Apical Migration of Junctional Epithelium |
movement of the junctional epithelium apical to its normal location |
|
|
Inflammation |
the body's reaction to injury or invasion by disease-producing organisms. The inflammatory response that occurs in periodontitis results in permanent destruction of the tissues of the periodontium |
|
|
Alveolar bone loss |
resorption of alveolar bone as a result of periodontitis |
|
|
Horizontal bone loss |
*most common pattern of bone loss
fairly even, overall reduction in height of alveolar bone |
|
|
Vertical bone loss |
*less common
uneven reduction in height of alveolar bone progresses more rapidly in bone next to root surface trench like area of missing bone alongside the root |
|
|
Osseous defects |
bony defects in the alveolar bone
(periodontitis results in defferent types of defects in the alveolar bone) |
|
|
Infrabony defects |
results when bone resorption occurs in an uneven, oblique direction
*primarily affects one tooth *classified by basis of # of osseous walls (may have 1, 2, or 3 walls) |
|
|
Osseous crater |
bowl-shaped defect in the interdental alveolar bone, with bone loss nearly = on the roots of 2 adjacent teeth |
|
|
Furcation involvement |
occurs on multi-rooted tooth when periodontal infection invades the area between and around the roots, resulting in a loss of alveolar bone between the roots of teeth
bone loss may be hidden by gingival tissue or may be clinically visible |
|
|
Attachment loss |
destruction of the fibers and bone that support the teeth |
|
|
Disease site |
is the area of tissue destruction, may involve one or more surfaces of the tooth |
|
|
Inactive disease site |
a disease site that is stable, with the attachment level of the JE remaining the same over time |
|
|
Active disease site |
a disease site that shows continued apical migration of the JE over time |
|
|
Gingival pocket |
is a deepening of the gingival sulcus as a result of swelling or enlargement of the gingival tissue |
|
|
Periodontal pocket |
a pathologic deepening of the gingival sulcus
1.) apical migration of JE 2.) destruction of the PDL 3.) destruction of alveolar bone |
|
|
Apical Migration |
movement of the cells of the JE from their normal position (coronal to CEJ) to a position apical to the CEJ |
|
|
Suprabony pocket |
-occur when there is horizontal bone loss
-JE located coronal to crest of alveolar bone |
|
|
Infrabony pocket |
-occur when there is vertical bone loss
-JE is located apical to crest of alveolar bone
-cratered-out area of bone alongside of the root surface |
|
|
Classification |
a systematic arrangement into groups or categories based on common attributes
|
|
|
Gingivitis |
inflammation of the periodontium that confined to the gingiva
results in damage to the gingival tissue that is reversible |
|
|
Periodontitits |
inflammatory disease of the supporting structures of the periodontium (gingiva, PDL, alveolar bone, and cementum) |
|
|
Periodontal disease |
refers to inflammation of the periodontium |
|
|
American Academy of Periodontology (AAP) |
initiated the currently accepted classification by organizing the International Workshop for a Classification of Periodontal Diseases and Conditions in 1999
includes 8 major categories |
|
|
Plaque-Induced Gingival Disease |
periodontal diseases involving inflammation of the gingiva in response to bacteria located at the gingival margin
*gingivitis associated w/ plaque biofilm formation = most common form of gingival disease |
|
|
Non-plaque induced gingival lesions |
not caused by bacterial plaque biofilm |
|
|
Chronic periodontitis |
*most common form of periodontitis
bacterial infection w/in supporting tissues of the teeth |
|
|
Aggressive Periodontitis |
bacterial infection characterized by a rapid loss of attachment and a less predictable response to periodontal therapy (than chronic)
-localized -generalized |
|
|
Periodontitis as a manifestation of systemic diseases |
(category) a group of periodontal diseases that is associated w/ 2 general categories of systemic diseases
1.) hematological (blood) disorders ex: leukemia or acquired neutropenia 2.) Genetic disorders ex: down syndrome or leukocyte adhesion deficiency syndrome
|
|
|
Necrotizing periodontal diseases |
unique type of periodontal disease that involves tissue necrosis (localized tissue death) |
|
|
Periodontal abscess |
localized collection of pus that forms in a circumscribed area of the periodontal tissue |
|
|
Tissue Necrosis |
localized tissue death
|
|
|
Periodontitis associated with endodontic lesions |
category of periodontal disease that involves infection or death of the tissue of the dental pulp |
|
|
Epidemiology |
the study of health and disease within the total population (rather than an individual) and the risk factors that influence health and disease
- how much disease, invesitages possible causes, applies results to treatment recommendations |
|
|
Incidence |
number of new disease cases in a population that occur over a given period of time |
|
|
Prevalence |
number of all cases (both old and new) of a disease that can be identified w/in a specified population at a given point in time |
|
|
Disease Progression |
the disease gets worses |
|
|
Periodontal pathogens |
bacteria that are capable of infecting the tissues of the periodontium
|
|
|
Intermittent disease progression |
theory that states periodontal disease is characterized by periods of disease activity and inactivity (remission) |
|
|
Risk factors |
factors that modify or amplify the likelihood of developing periodontal disease
major risk factors = 1.) bacterial pathogens 2.) cigarette smoking 3.) diabetes mellitus |
|
|
Bacteria/ Bacterium |
the simplest organisms that can be seen only through a microscope. -innocuous -pathogenic |
|
|
Innocuous |
species of bacteria that are no harmful |
|
|
Pathogenic |
a species of bacteria hat are capable of causing disease (aka virulent bacteria)
|
|
|
Virulent |
Species of bacteria that are capable of causing disease (aka pathogenic) |
|
|
Cell membrane |
tough protective layer encloses nearly all bacteria |
|
|
Gram staining |
a laboratory method that reveals differences in the chemical and ohysical poroperties of bacterial cell walls that divides bacteria into Gram-positive (PURPLE) and Gram-negative (RED) bacterial cell wall types |
|
|
Gram-positive bacteria |
bacteria with thick, single cell walls that show a purple stain under a microscope; most of the bacteria associated with a healthy periodontium are gram-positive |
|
|
Gram-negative bacteria |
bacteria with double cell walls that show a red stain under the microscope; believed to play an important role in inflammatory periodontitis |
|
|
Aerobic bacteria |
bacteria that requires O2 to live |
|
|
Anaerobic bacteria |
bacteria that cannot live in the presence of O2 |
|
|
Facultative anaerobic bacteria |
bacteria that can exist either with or without O2 |
|
|
Biofilm |
a well organized community of bacteria that adheres to a surface and is embedded in an extracellular slime layer, forms rapidly on almost any surface that is wet |
|
|
Extracellular slime layer |
a protective barrier that surrounds the mushroom-shaped bacterial mircrocolonies from antibiotics, antimicrobials, and body's immune system |
|
|
Nonmotile |
not capable of movement |
|
|
Aggregatibacter actinomycetemcomitans |
an important periodontal pathogen; strongly associated with aggressive periodontitis, implicated in chronic periodontitis (Gram-negative, nonmotile) |
|
|
Tannerella forsythia |
an important periodontal pathogen, most common species detected on or in the epithelial cells recovered in periodontal pockets (Gram-negative, nonmotile) |
|
|
Porphyromonas gingivalis |
an important periodontal pathogen, low numbers in health or gingivitis but more frequently detected in aggressive forms of periodontitis, increase periodontal disease progression, inhibit migration of leukocytes across epi barrier shown to induce and elevate host response in subjects w/ various forms of periodontitis (Gram-negative, nonmotile) |
|
|
Mixed infection |
periodontal disease is a mixed infection "bacterial soup" different bacteria within the plaque biofilm |
|
|
Transmission |
the transfer of periodontal pathogens from the oral cavity of one person to another |
|
|
Communicable |
a disease that may be passed from one person to another by direct or indirect contact via substances such as inanimate objects *little/no evidence periodontal infections are communicable |
|
|
Acquired Pellicle |
film composed of a variety of salivary glycoproteins and antibodies that forms within min after cleaning a tooth surface, protects the enamel from acidic activity |
|
|
Fimbriae |
hair-like structures possessed by some bacteria hat enable them to attach rapidly upon contact with the tooth surface |
|
|
Bacteria blooms |
periods when specific species or groups of species grow at rapidly accelerated rates with in a dental plaque biofilm |
|
|
Mushroom-shaped microcolonies |
bacteria clustered together and form a mushroom-shape that attach to the tooth surface at a narrow base |
|
|
Fluid channels |
a series of channels that penetrate the extracellular slime layer of a biofilm that provides nutrients and O2 for the bacterial mircocolonies and facilitate movement of bacterial metabolites, waste products and enzymes within the biofilm structure |
|
|
Fluid forces |
of the saliva surrounding the biofilm which influences the shape of the plaque biofilm (& spatial arrangement of the bacteria inside) |
|
|
Coaggregation |
the cell to cell adherence of one oral bacterium to another; the ability to adhere and coaggregate is an important determinant in the development of oral bacterial biofilms |
|
|
Tooth-associated plaque biofilm |
bacteria that attach to an area of the tooth surface that extends from the gingival margin almost to the JE @ base of pocket |
|
|
Tissue-associated plaque biofilm |
bacteria that adheres loosely to the epithelium of the pocket wall that can invade the gingival CT and be found w/in the periodontal CT and on the surface of the alveolar bone |
|
|
Unattached bacteria/plaque |
bacteria that is free-floating w/in the pocket environment |
|
|
Virulence factors |
the mechanisms that enable biofilm bacteria to colonize, invade and damage the tissues of the periodontium |
|
|
Peptides |
short chains of amino acids found in living bacterial cell membranes that control the transport of molecules in and out of the bacterial cell. T cells recognize these peptides and alert the immune system to the presence of bacteria |
|
|
Exotoxin |
harmful proteins released from the bacterial cell that act on the body's host cells at a distance |
|
|
Leukotoxin (LT) |
an exotoxin that may enable these bacteria to destroy leukocytes in the sulcus or pocket |
|
|
Bacterial enzymes |
agents that are harmful or destructive to host cells; a variety of enzymes produced by periodontal pathogens are important in tissue destruction |
|
|
Dormant bacteria |
inactive state in order to survive adverse environmental conditions |
|
|
Local contributing factors |
oral conditions or habits that increase an individual's susceptibility to periodontal infection |
|
|
Dental calculus |
a mineralized bacterial plaque biofilm, covered on its external surface by nonmineralized, living bacteria plaque biofilm |
|
|
Pellicle |
a thin bacteria-free membrane that forms on the surface of the tooth during the late stages of eruption |
|
|
Morphology |
the study of anatomic surface features of the teeth |
|
|
Overhanging restoration (overhang) |
a dental restoration that is not smoothly contoured with the tooth surface |
|
|
Palatogingivial groove |
developmental defect that forms on the palatal surface of a tooth and is most frequently seen on maxillary lateral incisors -plaque biofilm retention= common problem since groove is difficult/ impossible to clean effectively |
|
|
Pathogenicity |
the ability of the dental plaque to cause periodontal dissease |
|
|
Plaque biofilm pathogenicity |
ability of the bacteria in the dental plaque biofilm to produce periodontal disease |
|
|
Food impaction |
forcing food between teeth during chewing, trapping of food in the interdental area |
|
|
Tongue thrusting |
the application of forceful pressure against the anterior teeth with the tongue |
|
|
Mouth breathing |
a process of inhaling and exhaling air primarily through the mouth, rather than the nose (often occurs during sleep) |
|
|
Biologic width |
the space on the tooth surface occupied by the JE and the CT attachment fibers immediately apical to the JE |
|
|
Embrasure space aka Gingival Embrasure Space |
the small triangular open space(apical to contact area) between the curved proximal surfaces of two teeth - in health: interdental papillae fills space |
|
|
Encroaching on the embrasure space |
moving into/ in on the embrasure space |
|
|
Proshesis |
a appliance used to replace missing teeth |
|
|
Removable prothesis |
an appliance used to replace missing teeth that the patient can remove for cleaning and before going to bed; commonly called a partial denture |
|
|
Trauma from occlusion
|
excessive occlusal forces that cause damage to the periodontium |
|
|
Primary trauma from occlusion |
excessive occlusal forces on a sound (healthy) periodontium |
|
|
Secondary trauma from occlusion |
normal occlusal forces on an unhealthy periodontium (previously weakened by periodontitis) |
|
|
Functional occlusal forces |
normal occlusal forces produced during the act of chewing food |
|
|
Parafunctional occlusal forces |
occlusal forces that result from tooth-to-tooth contact made when not in the act of eating. |
|
|
Clenching |
continuous or intermittent forceful closure of the maxillary teeth against the mandibular teeth |
|
|
Bruxism |
the forceful grinding of teeth |
|
|
Occlusal adjustment |
a clinical therapy involving minor adjustments in an individual's bite that can be used to help control the damage from trauma from occlusion |
|
|
immune system |
a collection of responses that protects the body against infections by bacteria, viruses, fungi, toxins, and parasites; the immune system defends the body against invading microorganisms, as well as toxins in the environment |
|
|
Host |
a human in or which another organism lives; in the case of perio disease bacterial pathogens infect the host (individual living w the disease) |
|
|
Host response |
the way that an individual's body responds to an infection. Also see immune system and inflammation |
|
|
Leukocyte |
WBCs that act as a much like independent single-cell organisms able to move and capture microorganisms on their own |
|
|
Polymorphonuclear leukocytes (PMNs) |
phagocytic cells that actively engulf and destroy microorganisms; PMNs play a vital role in combating the pathogenic bacteria responsible for periodontal disease (aka neutrophils) |
|
|
Neutrophil |
phagocytic cells that actively engulf and destroy microorganisms play a vital role in combating the pathogenic bacteria responsible for periodontal disease (aka PMNs) |
|
|
Chemotaxis |
the process whereby leukocytes are attracted to an infection site in response to biochemical compounds released by invading microorganisms |
|
|
Lymphocytes |
small leukocytes that play an important role in recognizing and control foreign invaders; 2 main types that fight against perio disease = B and T |
|
|
B Lymphocytes |
small lymphocytes that help in the defense against bacteria, viruses, and fungi; principal fxn is to make antibodies- further differentiate into one of two types of cells= plasma B and memory B |
|
|
Antibody |
Y shaped proteins; one end of the y binds to the outside of the b cell and the other end binds to a microorganism and helps kill it |
|
|
Immunoglobulin |
Y shaped protein; 55 major classes are IgM, IgD, IgG, IgA, and IgE |
|
|
T lymphocyte |
small leukocytes whose main fxn is to intersify the response of other immune cells (such as B lymph and macrophages) to bacteria invasion |
|
|
Cytokine |
a general name for powerful regulatory proteins released by immune cells that influence the behavior of other near by cells; signal the immune system to send additional phagocytic cells to the site of an infection |
|
|
Complement system |
a complex series of protein circulating in the blood that works to facilitate phagocytosis or kill bacteria directly by puncturing bacteria cell membranes |
|
|
Membrane attack complex |
a protein unit created by the complement system that is capable of puncturing the cell membranes of certain bacteria |
|
|
Opsonization |
coating of the surface of a microorganism by complement components to facilitate the engulfment and destruction by phagocytes |
|
|
Endothelium |
thin layer of epi cells that line the interior surface of the blood vessels |
|
|
Transedothelial migration |
the process of immune cells exiting the vessels and entering tissue |
|
|
Phagocytosis |
the process by which leukocytes engulf and digest microorganisms |
|
|
Phagosomes |
during the process of phagocytosis, these are phagocytic vesicles that surround the bacterium |
|
|
Phagolysosome |
during the process of phagocytosis, these lysosome granules fuse with the vesicle to form |
|
|
Inflammatory biochemical mediator |
biologically active compounds secreted by cells that activate the body's inflammatory response; cytokines, prostaglandins, and matrix metalloproteinase = important in perio |
|
|
Chemokines |
major subgroup of cytokines that cause additional immune cells to be attracted to the site of infection/injury |
|
|
Acute vs Chronic Inflammation |
short-term normal inflammatory response that protects and heals the body following a physical injury or infection
long lived out of control inflammatory response that continues from more that a few weeks -pathological condition=active inflammation, tissue destruction, and attempts to repair |
|
|
C-reactive protein (CRP) |
a special type of plasma protein that is present during episodes of acute inflammation or infection; most important cardiovascular risk predictor |
|
|
Prostoglandins |
a series of powerful biochemical mediators, the most important = D,E,F,G, H, & I |
|
|
Biochemical Mediators |
biologically active compounds secreted y immune cells that activate the body's inflammatory response (important to perio= cytokines, prostaglandins, matrix metalloproteinase) |
|
|
Prostoglandins of the E series (PGE) |
a series of powerful biochemical mediators, one of the most important, play an important role in the bone destruction during periodontal disease |
|
|
Matrix metalloproteinases (MMPs) |
a family of at least 12 diff enzymes produced by various cells of the body that can act together to break down the CT matrix; presence of increased MMP levels causes extensive collagen destruction in the perio tissue |
|
|
systemic risk factors |
conditions or diseases that increase an indiviuals susceptibility to perio infection by modifying or amplifying the host response to the bacterial infection (including diabetes, osteoporosis, hormone alteration, meds, tobacco, genetic) |
|
|
Diabetes Mellitus |
a disease in which the body does not produce or properly use insulin (hormone needed to convert sugar starches and other foods into energy to sustain life) |
|
|
Type I vs Type II |
- type of diabetes caused by destruction of insulin producing cells of the pancreas
-type of diabetes that occurs when body doesn't make enough insulin, body cells ignore insulin and fail to use it to help bring glucose into cells *most common type |
|
|
Gestational diabetes |
a form of diabetes that occurs during pregnancy in women who have never had diabetes before pregnancy |
|
|
Well-controlled diabetes |
a form of diabetes that is controlled does NOT increase periodontal disease risks |
|
|
Leukemia |
type of caner that beings in the blood cells in which bone marrow produces lg number of abnormal WBC that do not fxn properly |
|
|
Acquired Immunodeficiency Syndrome (AIDS) |
communicable disease caused by HIV, increased risk for developing certain cancers, and infections due to a weakened immune system |
|
|
Linear gingival erythema (LGE) |
a gingival manifestation of immunosuppression characterized by a distinct linear erythematous (red) band that is limited to the free gingiva (formally known as HIV associated gingivitis) |
|
|
Osteoporosis |
a reduction in bone mass that causes an increased susceptibility to fractures, occurs most commonly in postmenopausal women, in sedentary or bedridden individuals, and pt receiving long term steroid therapy |
|
|
Osteopenia |
condition in which there is a decrease in bone density but not necessarily and increase in risk or incidence of bone fracture, most common in 50+ who have lower than average bone density but don't have osteoporosis |
|
|
Postmenopausal osteoporosis |
disorder caused by the cessation of estrogen production and is characterized by bone fractures |
|
|
Pregnancy ginigivitis |
ging inflammation initiated by plaque biofilm and exacerbated by hormonal changes in the 2nd and 3rd tris |
|
|
Pregnancy associated pyogenic granuloma |
LOC mushroom shaped ging mass projecting form the ging margin or more commonly from ging papilla during pregnancy |
|
|
Menopausal gingivostomatitis |
decreased levels of circulating hormones in women who are menopausal or post menopausal that may result in oral changes, such as thinning of the oral mucosa, dry mouth, burning sensations, altered taste, ging recession, & alv bone loss |
|
|
Drug induced gingival enlargement |
an esthetically disfiguring overgrowth of the gingiva that is a side effect associated w certain meds (anticonvulsants, calcium channel blockers, immunosuppressants) |
|
|
Phenytoin |
one of the most commonly used anticonvulsant meds to control convulsions or seizures in the tx of epilepsy ( assoc. w drug influenced ging enlargement) |
|
|
Cyclosporine |
an immunosuppressive agent used for prevention of transplant rejection as well as for management of a number of autoimmune conditions (rheumatoid arthritis) assoc. w drug influenced gingival enlargement |
|
|
Nifedipine |
a calcium channel blocker used as coronary vasodilator in the tx of hypertxn, angina, and cardiac arrhythmias, associated w drug influenced gingival enlargement |
|
|
Ask, Advise, Refer Model |
Program- the ADHA's smoking cessation initiative- 3 step program 3 minutes or less can save lives |
|
|
Multifactorial etiology |
periodontitis is a disease that results from the interaction of many factors |
|
|
Biologic equilibrium |
a state of balance in the internal environment of the body |
|
|
Disease- promoting factors |
factors leading to the change or advancement of periodontal destruction |
|
|
Health- promoting factors |
factors preventing the destruction of periodontal disease |
|
|
Risk assessment |
process of identifying risk factors that increase an individual's probability of disease |

