![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
70 Cards in this Set
- Front
- Back
|
What is the incubation period for Measles?
|
8-12 days after initial exposure the Paramyxovirus
|
|
|
Cough + Coryza + Conjunctivitis = ?
|
Measles
|
|
|
Measles
**occur 2-3 days of onset of symptoms (of 3 C's) |
Small irregular red spots with central gray or bluish white specks...what disease?
|
|
|
Measles
|

Approximately 5 days after the onset of symptoms, an erythematous maculopapular rash erupts on the head & spreads caudally, lasting 4-5 days
|
|
|
What are 2 severe complications of Measles?
|
Acute Encephalitis
Subacute Sclerosing Panencephalitis |
|
|
This infection has an incubation period of 14-21 days. When symptoms do occur, an erythematous maculopapular, discrete rash, with generalized lymphadenopathy & slight fever. The rash rarely last longer than 5 days. Fever may accompany the onset of rash.
|
Rubella
|
|
|
This is common in adolescents with Rubella infection
|
Polyarthralgia & Polyarthritis
|
|
|
These 2 things are rare complications of Rubella infection
|
Encephalitis & Thrombocytopenia
|
|
|
Common acute disease of infants & young children caused by Human Herpesvirus 6 (HHV-6)
|
Roseola Infantum
|
|
|
Illness that begins with an abrupt fever characterized by temps of 103-106F that persists for 1-5 days. During the fever, the child generally appears well & has no physical findings to explain the fever. On the 3rd-4th day, a maculopapular rash appears on the trunk & spread peripherally. The rash typically appears as the fever resolves. Initially, leukocytosis up to 20,000 microliters with a left shift may exist, but by the 2nd day of illness, leukopenia & neutropenia may be noted.
|
Roseola Infantum (HHV-6)
|
|
|
What complication may occur in Roseola Infantum?
|
Febrile Seizures due to rapid increase in temp during onset of infection
|
|
|
Describe the 3 stages of the rash in Erythema Infectiosum (Fifth Disease)
|
1. marked redness of the cheeks = "slapped cheek"
2. lacy or reticulate, red, pruritic rash then starts on the arms & spreads to trunk & legs 3. Fluctuations in the severity of the rash lasting for 2-3 wks. Fluctuations occur with temp changes & exposure to light |
|
|
What are 3 complications of Erythema Infectiosum?
|
Arthritis
Hemolytic Anemia Encephalopathy |
|
|
When is Hand-foot-and-mouth disease common? (what part of the year)
|
Spring & Summer
|
|
|
What virus causes hand-foot-and-mouth disease?
|
Coxsackie A virus
|
|
|
Describe the symptoms of hand-foot-and-mouth disease
|

Prodrome of fever, anorexia, & oral pain
Crops of ulcers on the tongue & oral mucosa & a vesicular rash on the hands, feet, & occasionally buttocks Individual vesicles often have a "football" shape with surrounding redness |
|
|
When can fatal disseminated Varicella (chickenpox) develop?
|
1. in immunocompromised children
2. neonates whose mothers develop the infection within 1 week of delivery |
|
|
Describe the disease progression of Varicella
|
-incubation of 10-21 days
-prodrome of mild fever, malaise, anorexia, & occasionally a scarlatiniform or morbilliform rash -Pruritic rash occurs on following day appearing first on the trunk & then spreading peripherally. Rash begins as red papules & develops rapidly into vesicles. Vesicles then become cloudy, break, & form scabs. Lesions occur in widely scattered "crops", so several stages of lesions are usually present at the same time |
|
|
When are patients infectious with Varicella?
|
from 24 hours before the appearance of the rash until all the lesions are crusted, which usually occurs 1 wk after the onset of the rash
|
|
|
What 3 things may occur in immunocompromised patients with Varicella infection?
|
1. Meningoencephalitis
2. Hepatitis 3. Pneumonitis **associated with a 20% mortality rate **immunization with varicella vaccine has reduced the frequency of this infection in the US |
|
|
This represents a reactivation of Varicella-zoster virus infection & occurs predominately in adults who previously have had varicella & have circulating antibodies
|
Herpes Zoster
|
|
|
HOw does Herpes Zoster present?
|

follows a Dermatomal distribution due to dorsal root ganglion storage
begins with pain along the affected sensory nerve & is accompanied by fever & malaise -a vesicular eruption then appears in crops confined to the dermatomal distribution & clears in 7-14 days |
|
|
What is contraindicated when Varicella is suspected? Why?
|
Ibuprofen b/c of increased risk of Streptococcal Cellulitis
|
|
|
Why should Aspirin be avoided when treating fever in the setting of Viral infection?
|
to avoid Reye's Syndrome
|
|
|
What may the itching associated with Fifth Disease, Varicella, & Herpes Zoster be treated with?
|
Oral Antihistamine
|
|
|
What reduces the risk of secondary bacterial infection with a Chickenpox infection?
|
daily bathing in lukewarm water
|
|
|
What are Immunocompromised children who are exposed to Varicella-zoster given?
|
VZIG within 96 hours of the exposure & are observed closely
|
|
|
What 2 bacteria cause most bacterial skin infections?
|
group A Beta-hemolytic streptococci
S. aureus |
|
|
What causes Bullous Impetigo?
|
toxin-producing strain of S. aureus
|
|
|
Describe the Bullous Impetigo lesions
|
Begin as red macules that progress to bullous (fluid-filled) eruptions on a red base
-range from a few mm to a few cm in diameter After the bullae rupture, a clear, thin, varnishlike coating forms over the denuded area |
|
|
What can Bullous Impetigo lesions be mistaken for?
|
Cigarette burns, raising the suspicion of abuse
|
|
|
Describe Nonbullous Impetigo
|

1. caused by both group A beta-hemolytic + S. aureus
2. begin as papules that progress to vesicles & then to painless pustules measuring approximately 5 mm in diameter with a thin red rim 3. Pustules rupture, revealing a honey-colored thin exudate that then forms a crust over a shallow ulcerated base 4. Lymphadenopathy is common with Strep impetigo (fever is uncommon) |
|
|
What causes Scalded Skin Syndrome? When does it most commonly occur?
|
exfoliative toxin-producing isolate of S. aureus
In infancy & rarely occurs beyond 5 yoa |
|
|
Describe the progression of Scalded Skin Syndrome
|
1. Onset is abrupt
2. Diffuse redness, marked skin tenderness, & fever 3. Within 12-24 hrs, superficial flaccid bullae develop & then rupture almost immediately, leaving a beefy red, weeping surface |
|
|
What does a positive Nikolsky sign mean in SSSS?
|
separation of the dermis on light rubbing
|
|
|
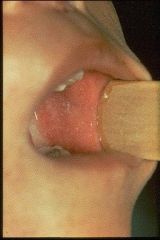
Staphylococcal Scalded Skin Syndrome
|

What is this?
|
|
|
Furuncles
|

These begin as superficial folliculitis & are most frequently found in areas of hair-bearing skin that are subject to friction & maceration, especially the scalp, buttocks, & axillae
|
|
|
What is a Carbuncle?
|
accumulation of furuncles
|
|
|
What is the most common cause of hematogenously spread cellulitis?
|
Strep pneumoniae
|
|
|
What is limited Nonbullous Impetigo treated with?
|
topical mupirocin ointment
|
|
|
What are Bullous Impetigo & Nonbullous Impetigo, if numerous, treated with?
|
First-generation Cephalosporin = Cephalexin
-effective against both Staph & group A Strep or Clindamycin or Trimethoprim-Sulfamethoxazole for MRSA |
|
|
How is Scalded Skin Syndrome treated?
|
Mild-Moderate = anti-staph medication
Severe = meticulous fluid management & i.v. Oxacillin or Clindamycin |
|
|
How is Superficial Folliculitis treated?
|
aggressive hygeine & topical mupirocin
**exception -- folliculitis of the male beard is treated with oral antistaph drug |
|
|
How is simple Furunculosis treated?
|
moist heat
|
|
|
How are large & deep furuncles treated?
|
Incision & drainage -> topical mupirocin
|
|
|
What is the etiologic agent of Tinea Versicolor?
|
Malassezia furfur
|
|
|
Tinea Versicolor
|

Superficial tan or hypopigmented oval scaly lesions on the neck, upper part of the back, chest , & proximal arms in a christmas tree distribution
|
|
|
What is the treatment for Tinea Versicolor?
|
Selenium Sulfide shampoo or other antifungal agents
|
|
|
What can Diaper Rash result from?
|
1. Atopic Dermatitis = a form of eczema, is a non-contagious disorder characterized by chronically inflamed skin and sometimes intolerable itching
2. Primary irritant dermatitis 3. Primary or Secondary Candida infections |
|
|
Topical Nystatin along with Barrier Creams
|

What is the treatment for Candida Diaper Rash?
|
|
|
What is the cause of Acne Vulgaris?
|
enlargement of SEBACEOUS GLANDS, increased sebum production, proliferation of Propionibacterium acnes, & secondary inflammation changes
|
|
|
What is the stimulus for Sebaceous gland development & secretion leading to Acne Vulgaris?
|
Androgens
|
|
|
Why would you want to differentiate common acne from NOdulocystic Acne?
|

Latter causes hypertrophic or pitted scarring
|
|
|
This drug works by decreasing the colonization of P. acnes & decreasing the development of microcomedomes by lessening the concentration of free fatty acids
|
Benzoyl Peroxide
|
|
|
These drugs have strong anticomedogenic activity; however, side efects may limit use & include dryness, burning, & most importantly photosensitivity by reducing the thickness of the stratum corneum layer
|
Topical Retinoids = TRetinoin, Adapalene, Tazarotene
|
|
|
What must be obtained before initiating treatment of Retinoic Acid for acne?
|
Pregnancy test within 2 wks of therapy b/c it is a teratogen
-contraception must be used from 1 month prior to 1 month after therapy Controversial associations of Isotretinoin & mood alterations have also been reported |
|
|
What is a risk factor for Psoriasis?
|
HLA type C6
|
|
|
Psoriasis
|

Nonpuritis rash that consists of red papules that coalesce to form plaques with sharply demarcated borders & a silvery or yellow-white scale. The scales tend to build up into layers, and their removal may result in pinpoint bleeding (Auspitz sign)
|
|
|
How do you differentiate b/w Psoriasis & Reiter's Syndrome?
|
Reiter's Syndrome will have lesion of the mucous membrane
|
|
|
How do you differentiate b/w Psoriasis & Atopic Dermatitis?
|
Atopic Dermatitis is pruritic & concentrated in flexural creases, whereas psoriasis is not usually pruritic & favors extensor surfaces
|
|
|
What is the treatment management of Psoriasis?
|
It is characterized by remissions & exacerbations
-educate patient that the disease is chronic & recurrent & cannot be cured but can be controlled -keep the skin well hydrated -Tar preps may be added to the daily bath or used as ointment -Severe cases = natural sunlight or UVB light in conjunction with Tar lubricant |
|
|
T or F: Psoriasis is pruritic
|
False
|
|
|
Acute, self-limited, hypersensitivity reaction that is uncommon in children. Etiologic agents include viral infection (herpes, adenovirus, & Epstein-barr), Mycoplasma pneumoniae infection, drug ingestion (esp Sulfa drugs, immunizations, & food rxns
|
Erythema Multiforme
|
|
|
Describe the lesions in Erythema Multiforme
|

Erythematous macules -> Papules -> plaques -> vesicles -> Target lesions
Lesions change over days, not hours Tend to occur over dorsum of hands & feet, palms & soles, & extensor surfaces of extremities, but may spread to trunk Burning & itching are common Systemic manifestations include fever, malaise, & myalgias |
|
|
What is the most common cause of recurrent erythema multiforme in children?
|
Herpes Simplex Virus
|
|
|
What is Stevens-Johnson's Syndrome?
|

Most severe form of Erythema Multiforme
-prodrome of 1-14 days of fever, malaise, myalgias, arthralgias, arthritis, headache, emesis, & diarrhea -followed by sudden onset of high fever, erythema multiforme skin lesions, & inflammatory bullae of 2 or more mucous membranes |
|
|
What are the most common causes of Stevens-Johnson Syndrome?
|
Drugs & Mycoplasma infections
|
|
|
Most severe form of cutaneous hypersensitivity & is similar to Staphylococcal Scalded Skin Syndrome in that both result in sloughing of the epidermal layer
|
Toxic Epidermal Necrolysis
|
|
|
List the size classifications for Congenital Nevi
|
Large = > 20 cm
Intermediate = 2-20 cm Small = < 2 cm |
|
|
T or F: Giant/Large Nevi have an increased risk of Melanoma
|
True
-must be followed annually for changes & may require complete excision |

