![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
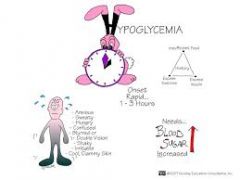
S/S of hypoglycemia/ nx |
Teach the child and parents how to recognize hypoglycemia and what may cause it to occur.
CAUSES of hypoglycemia include:
TREATMENT of hypoglycemia |
|
|
|
s/s of hyperglycemia/nx |
S & S include: Polyuria, polydipsia, blurred vision, weakness, headache, weak, rapid pulse, nausea and vomiting, to acetone breath (fruity odor) to mental status changes and Kussmaul respirations which is diabetic ketoacidosis (DKA)
Causes include :
Hospitalized -Treat dehydration with IV 0.9% or 0.45% N/S and electrolytes
|

|
|

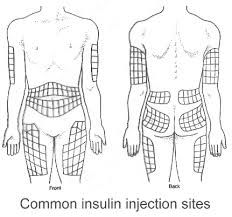
Insulin administration technique |
Insulin increases glucose transport into cells and promotes conversion of glucose to glycogen, decreasing serum glucose levels. Insulin is given subcutaneous with 27 to 29 gauge needle and syringe or other administration device. |

|
|
|
DM teaching/dietary teaching
|
Chronic metabolic syndrome in which body is unable to use carbohydrates due to lack of insulin produced from the pancreas or resistance to the insulin produced by the pancreas causes the inability to transport glucose into the cells properly. Leads to inability to store fats properly and causes a decrease in protein synthesis
Disease requires lifestyle alterations (diet, glucose monitoring, and insulin administration)
Type 2 is:
Signs and Symptoms
Imbalanced Nutrition: Less than body requirements related to inability to metabolize glucose AEB loss of weight.
Risk for injury related to hyper-hypoglycemia AEB S/S of elevated or low blood sugar.
Infants and toddlers may have hydration problems
Children need to assume their own care
Diet The goals of nutritional management in children are to: Glycemic index of selected foods has an impact on the manipulation of dietary needs |
|
|
|
Insulin onsets/peaks/duration |
Short –acting insulin- Humulin Regular onset is 30 min to 1 hour and lasts 5-8 hours. (Peak is 2-5 hours) Regular Insulin can be administered IV.
Insulin increases glucose transport into cells and promotes conversion of glucose to glycogen, decreasing serum glucose levels. Insulin is given subcutaneous with 27 to 29 gauge needle and syringe or other administration device. Assess for local allergic reaction and signs of lipoatrophy or lipohypertrophy (rotate sites!) |
|
|
|
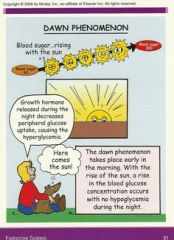
Dawn phenomenon teaching |
early morning elevated blood sugar due to growth hormones secreted in the early morning hours.
|
|
|
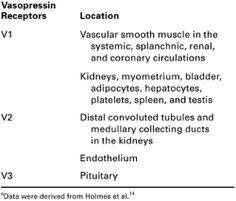
Diabetes insipitus - Vasopressin teaching/assessment |
Hereditary (autosomal dominant) or acquired as the result of a head injury or tumor causing decreased secretion of vasopressin, the antidiuretic hormone from pituitary gland
Signs and Symptoms
Interventions |

|
|
|
Dose considerations of thyroid replacement medications |
x |
|
|
|
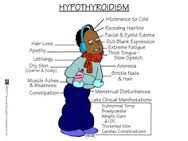
S/S hypothyroidism
|
Sluggish, lethargic, sleepy
Enlarged tongue, dry skin and hair Hypotonia– flaccid muscle tone & can cx constipation May have bulging soft mass in the belly button (umbilical hernia) |
|
|
|
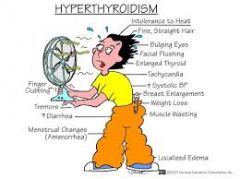
S/S hyperthyroidism |
x |
|
|
|
Immunization schedules- tetanus/MMR
|
tetanus 5 doses=2,4,6 mo, 15-18mo, 4-6y
MMR= 2 doses---- 12-15mo, 4-6y |
|
|
|
Immunization contraindications |
Allergy to neomycin: notify physician before taking inactivated poliovirus vaccine, MMR, & varicella (chickenpox)
Rotavirus vaccine is a live attenuated oral vaccine
Assess allergies, such as to Latex, eggs, etc.
Contraindications to Live Virus Administration |
|
|
|
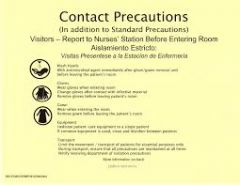
Communicable disease precautions |
Medical aseptic technique: purpose is to prevent spread of infection
Transmission-based precautions include three types:
Reverse isolation
|
|
|
|
Communicable periods of chicken pox |
x |
|
|
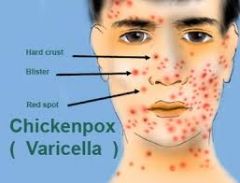
Chicken pox-- S/S / teaching/precautions |
x |
|
|
|
Immunization teaching |
x |
|
|
|
HIV precautions |
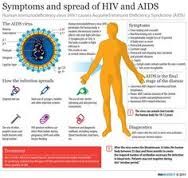
Acquired via
Infectious but not highly contagious
Prevention |
|
|
|
Rubeola precautions |
Susceptible HCWs should not enter room if immune caregivers are available. No recommendation for wearing face protection (e.g., a surgical mask) if immune. Pregnant women who are not immune should not care for these patients 17, 33. Administer vaccine within three days of exposure to non-pregnant susceptible individuals. Place exposed susceptible patients on Droplet Precautions; exclude susceptible healthcare personnel from duty from day 5 after first exposure to day 21 after last exposure, regardless of post-exposure vaccine |
|
|
|
Obsessive compulsive disorder -S/S |
Recurrent persistent repetitive thoughts invade the conscious mind
Obsessions
Differs from adults in that the sx are usually not part of an obsessive personality
Clomipramine: to control behavior
|
|
|
|
ADHD medication s/e |
Receptive language: listening/understanding
Manifestations of ADHD
Hyperactivity (at least 2 of the following)
Dexedrine
|
|
|
|
ADHD testing |
Einstein Evaluation of School Related Skills
|
|
|
|
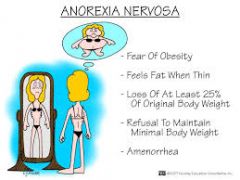
Anorexia nervosa nx |
Failure to maintain minimum normal weight for age & height (less than 85% of expected body weight)
Etiology may be genetic Primary symptom is severe weight loss There is:
May require hospitalization
Most gain weight in hospital setting
|
|
|
|
Bulimia r/f |
Misuse of laxatives and/or diuretics Leads to:
|
|
|
|
Eating disorder nx
|
x
|
|
|
|
Autism S/S & teaching |
Developmental disorder manifested by motor-sensory, cognitive and behavior dysfunctions
Lack of pointing or gesturing at an early age
Early identification, referral and intervention
Approach the child at a slow pace and with few distractions
|
|
|
|
Pregnancy/STD prevention teaching |
x |
|
|
|
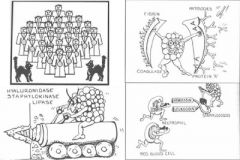
Staphylococcus nx |
primary infections of newborns at umbilicus/circumsision, scaled skin syndrome, s/s small pustules indicates staph, isolate/iv abx topical abt creams |
|
|
|
Diaper rash interventions
|
x |
|
|
|
Accutane teaching |
x |
|
|
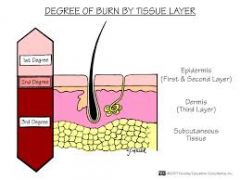
Burn care intervention/ teaching |
skin thinner so burn deeper, larger body surface area results in greater loss of f/e, iommature response systems cause shock and HF, ^bmr= ^protien/calorie needs, smaller muscle mass and fat results in ^ protien calorie needs, skin more elastic and pulling on scarring causes larger formation of scar tissue, immature immune system predis the child to developing infections, prolonged immobilization affects growth and development, TBSA- size of burn is calculated as a % of TBSA,charts are used according ot age not rule of 9's as in adult, burn either partial/full thickness]
First/superficial tx is to immerse in cold water to stop burning and apply antimicrobial or silvadene ointment
second/partial thickness- blistered moist pink/red tx is same as superficial if small area/deep dermal burn if larger area
deep dermal/deep partial is mottled ran tan or dulll white w blisters and is painful, immerse in cold water cover with sterile dressing/clean cloth, do not break blisters and seek medical attention
third/full thickness leathery and tough dry skin does not refull or blanch, dull brown tan black pearly white and painless, immerse in cold h20/wrap and apply sheet or sterile dressing, do not tx have client lay down and activate EMS
Firsts 48h after burn watch hyponatremia and ^k+
Diag- Will see ^ HCT, decreased HGB, ^ WBC, monitor ABGS,
STAGES IN TX OF BURNS- emergent/recisitative stage begins with burn and continues until fluid recusuitation is stable, includes estimating extent of the burn, initial first aid and fluid recisitation and assess for shock and possible transport 1 stop burning 2. eval injury and establish airway first esp if smoke inhalation 3. cover burn 4 transport to ER Superficial burn care- ointment dressings, silvadene unless allergic to sulfa NX- hospital major burns, resp status, elev hob 30 open airway for intubation o2 lfow face mask for ABG's, may need ventillator for assist and sedation, npo at first and guidelines are used to replace the extensive fluid/e lossess, fluid replacement necessary all burns 20% or more TBSA, colloids/crystalloids, blood/blood products are used for fliod replacement, (cystalloid: amin 2 large bore periph or CV line to maintain urinary output to 30 to 50 ml/h; lactated ringers: isotonic is IV due to closeness to extracellular fluids, may require hemodynamic monitoring)I&o closely wewight q day, pain meds IV usually smaller amts more freq. wound care: open= antimicrob tx; closed= dressings, asess for s/s infections STAGE 2:Diuresis----closure of burns, tx of hydrotherapy, debridement exission and grafting of full thickness wounds, enternal/parenteral feedings, topical/systemic antimicrobial agents to prevent infection--nx 4k-6k calories q day due to excessive protien breakdown, enternal feedings with NG tube are started within 24-48j to prevent hypermetabolism and improve nitrogen balance, weight and I&o, Vitamins, Enternal feedings contrain in curling ulcers/bowel obstruc/ feedig intol/pancreatitiis/septic ileus- asess BS x4; if unable to tolerate feedings-subclavian cath is inserted and TPN is admin Assess VS frew , I&o 30ml/h admin tetanus toxoid to prevent tetanus in wound if wound on face= clean with NS,mechanical debridement during hydrotherapy, enzymatic debridemtn with Elase, surgical debridement called escarotomy,
open wound care- apply sulfamylon abx prevent infec, caution with renal pulmon clients will feel pain with application, 1-3q day; With silvadene monitor for WBC for leukopenia, 1-2 q day completely cover, CLOSED usually bid, wet dressings soaked every 2h
STAGE 3 long recovery for children, active passive ROM by pt in hydrotherapy and q 2h, early ambulation, splints to immobilize,
|

|
|
|
Lice S/S & treatment |
aka pediculosis- capitus (head) common in children, corporis is on body, pubis is pubic area aka crabs, trans via contam items, s/s white rice looking parasite, matted hair and pustules on face tx- rid nix or kwell shampoo and repeat in 1wk, vinegar 1:1 to clean combs, petroleum to eyebrows |

|
|

Eczema teaching |
usually during first 2 y, s/s local vasodilation in affected area usually face with vesicles that weep.
nx- relieve puritis inflam and prevent infec, emollen baths/wet compresses, soap substitutes, cortisone creams, hypoallergic formulas, new drug elidel advertised |
|
|
|
Strawberry nevus teaching
|
dilated capillaries in dermal space that occurs a few weeks after birth usually on head or face, becomes raised, 60% disappear by 5y and 90% by 9y, if not excision/laser |
|
|
|
Cradle cap care |
remove with shampoo and soft rag or dandruff shamp for older child |
|
|
|
Endocrine system |
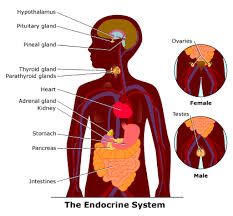
One of the control systems of body which uses hormones to target glands
Maternal endocrine dysfunction can affect the fetus
Most inborn errors of metabolism can be detected by clinical signs or screening tests performed in utero
|
|
|
|
Diag tests |
PKU is an important screening device for identifying enzyme deficiency Tissue biopsy
Diag burns- eval of renal perfusion/nutritional status; with assmt of nitrogen loss is measured in 24h total nitrogen, urea nitrogen, amino acid nitrogen, protienuria, elevated urine specific gravity. |
|
|
|
Vals |
sodium 135-145 K 3.5-5 |
|

