![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
77 Cards in this Set
- Front
- Back
|
What is proximal tubule well adapted for? What are they "reach" in? Why?
What do the epithelial cells have? Basolateral membrane structure? |

|
|
|
What are the two parts of the proximal tubule? Proportions?
|

|
|
|
What are the three functional segments of the PT?
|

|
|
|
What are the three major functions of the proximal tubule?
|

|
|
|
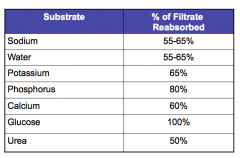
What substates are reabsorbed in the PT? Which ones are 100% reabsorbed?
Sodium, water, potassium, phosphorus, calcium, glucose, urea |
|
|
|
What are the two different pathways of reabsorption in the PT?
|

|
|
|
1. Involves movement of a substance against electrochemical gradient and requires energy. EXAMPLE?
|
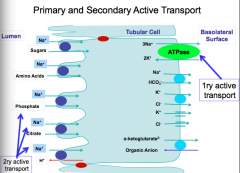
Primary active transport
Na+-K+-ATPase |
|
|
Does not use energy directly but depends on primary active transport. TWO DIFFERENT TYPES? EXAMPLES?
|
Secondary active transport:
Antiport (exchanger): ex: Na + -H + -exchanger Symport (co-transporter): ex: Na + -Pi --co-transporter |
|
|
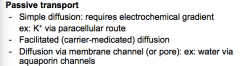
Three types of passive transport?
|
|
|
|
Form of endocytosis. EXAMPLE?
|
Pinocytosis
Insulin uptake by PT cells |
|
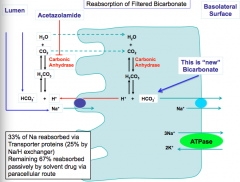
Draw this out.
|

|
|
|
What are three ways to regulate PT reabsorption?
|
Glomerulotubular balance
Arterial pressure (pressure natriuresis) Hormonal regulation |
|
|
What is glomerulotubular balance?
|
|
|
|
What is the arterial pressure effect?
|

|
|
|
What are two mechanisms of hormonal regulation? What does each do?
|

|
|
|
Two reasons that PT is highly susceptible to ischemia:
|
1. ATP dependence for the function of Na-K-ATPase
2. Apical and basolateral (polarized) structure of PT cells is dynamic and ATP dependent process relying on cytoskeleton. |
|
|
What does the polarized structure of PT cells involve the formation and maintenance of?
|
Cell-cell and cell-substratum attachments and the targeted delivery of plasma membrane components to the appropriate domains.
|
|
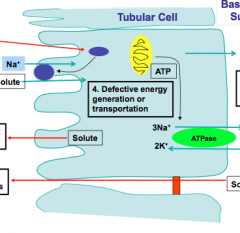
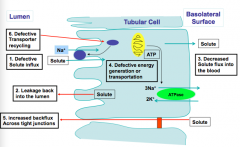
Identify some possible defects in PT function.
|
|
|
|
What are two ways to classify PT dysfunction?
|
1. Based on mechanism of disfunction
2. Classification based on the mode of inheritance (genetic or acquired) |
|
|
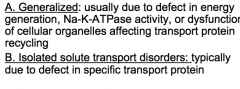
What are the two ways to classify on the basis of mechanism of disfunction?
|
|
|
|
Isolated PT Dysfunction: DEFECT IN GLUCOSE REABSORPTION
Hereditary renal glucosuria: Type of trait, mutation, and defect results in what? What is the glucose concentration exceeds normal threshold? |

|
|
|
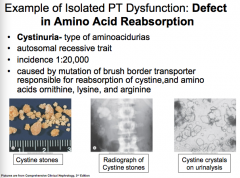
Isolated PT Dysfunction: DEFECT IN AMINO ACID REABSORPTION
Cystinuria = type of aminoacidurias Type of trait, mutation, effects of mutation? |
|
|
|
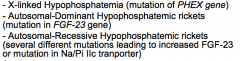
Example of Isolated PT dysfunction: DEFECT IN PHOSPHATE REABSORPTION:
Can the defect in isolated phosphate reabsorption be inherited or acquired? |
Can be inherited or acquired.
|
|
|
What are some inherited causes? List mutation.
|
|
|
|
What are some acquired causes?
|

|
|
|
What is the most common inherited phosphate wasting disorder? How is it inherited? What is it caused by? Does the transport protein (Na-Pi) have a mutation? What is it characterized by? How does it present clinically?
|

|
|
|
What is Hartnup disease? Symptoms? Mutation?
|
Isolated PT dysfunction
|
|
|
What is Vitamin D-rickets type 1? Defect? Leads to what?
|
Isolated PT Dysfunction
|
|
|
What do defects in uric acid handling cause?
|
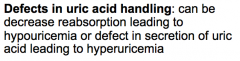
Isolated PT dysfunction
|
|
|
What is Faconi Syndrome?
How is it inherited? What are some possible mechanisms behind it? |
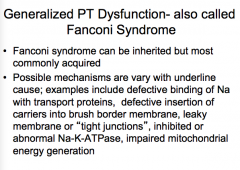
Generalized PT disfunction
|
|
|
What are the metabolic abnormalities of Faconi syndrome?
|
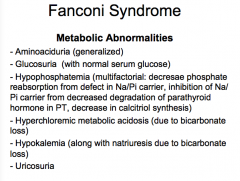
--Aminoaciduria
--Glucosuria --Hypophosphatemia --Hyperchloremic metabolic acidosis --Hypokalemia --Uricosuria |
|
|
What are the clinical manifestations of Faconi syndrome?
|

|
|
|
What are some inherited causes of Faconi syndrome?
|
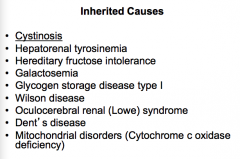
CYSTINOSIS!
|
|
|
What is an important drug that causes Faconi syndrome?
Dysproteinemia that cause Faconi syndrome? |
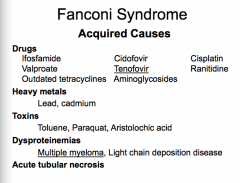
Drug = tenofovir
Dysproteinemia = Multiple myeloma |
|
|
True or false:
Isolated PT dysfunctions are common and never results from disorders of specific transport proteins. |
False:
...RARE and TYPICALLY RESULT.. |
|
|
True or false:
Generalized PT dysfunctions lead to more severe clinical manifestations from loss of multiple substances and usually accompanied by cause-specific extra renal manifestations (underline defects leading to generalized PT disorders could be not unique to PT cells or underline cause also exerts additional organ toxicities) |
True
|
|
|
True or false:
Inherited PT disorders are mostly encountered in adults. |
False = children
|
|
|
True or false:
Acquired forms of PT dysfunctions or mild forms or inherited PT disorders occur in adults. |
TRUE
|
|
|
What does water homeostasis determine?
What does osmolality reflect? What does osmotic pressure determine? What are the effective osmoles that determine body fluid osmolality and the ineffective ones that cross easily between body compartments? |

|
|
|
How do you calculate Posm? Simply effective Posm?
What is the relationship between Posm and total body osmolality? What does TBO equal? How do you approximate plasma Na? WHAT ARE PLASMA SODIUM CHANGES MAINLY DETERMINED BY? |

|
|
|
Effect of each on Posm and Pna:
"Normal" TBW Increase in TBW Decrease in TBW |

|
|
|
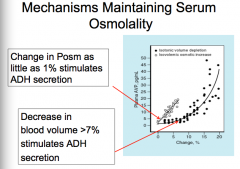
What is the pathway of mechanisms maintaining serum osmolality?
|

|
|
|
What is the normal Posm? What is the osmotic threshold for ADH release? What is the osmotic threshold for thirst?
|

|
|
|
What two changes stimulate ADH secretion? Numbers?
|
|
|
|
What is the principle target for regulation of water reabsorption by ADH?
What two ways does ADH regulate this (think time)? |

|
|
|
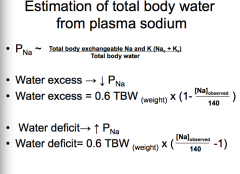
How do you estimate total body water from plasma sodium?
What effect does water excess and deficit have on Pna? How do you calculate water excess and water deficit? |
|
|
|
What is the most common electrolyte disorder? What does the serum concentration have to be?
|

|
|
|
What two ways can hyponatremia occur with a different Posm?
|
1. Increased osmolality (hyperomolar) hyponatremia
2. Normal osmolality and hyponatremia (pseudohyponatremia) 3. Decreased osmolality (hypoosmolar) hyponatremia (TRUE HYPONATREMIA) |
|
|
Mechanism behind increased osmolality (hyperosmolar) hyponatremia.
|

|
|
|
Mechanism behind normal osmolality and hyponatremia:
|

|
|
|
Mechanism behind decreased osmolality (hypoosmolar) hyponatremia: TRUE HYPONATREMIA
|

|
|
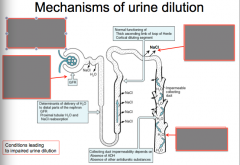
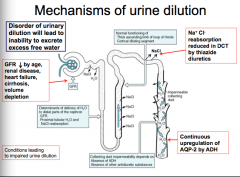
What does disorder of urinary dilution lead to?
Locations and mechanisms that cause urine dilution: |
|
|
|
How does true hyponatremia occur?
Can changes in TBW co-exist with total Na changes (decrease or increase in Na)? Which increase predominantes? What is usually present in the majority of cases of true hyponatremia? |

|
|
|
What are some causes of true hyponatremia (hyponatremia with volume depletion)?
|

|
|
|
What are some causes of true hyponatremia with normal volume status?
|

|
|
|
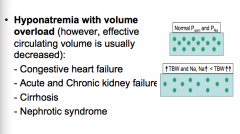
What are some causes of true hyponatremia (with volume overload)? But what happens to effective circulating volume usually?
|
|
|
|
What are other causes of true hyponatremia? Think osmostat and drinking.
|

|
|
|
What serum Na+ concentration is considered hypernatremic?
What does it occur as a result of? Think TBW Can changes in TBW co-exist with total Na changes? What predominates? What is the main defense mechanism against hypernatremia? What does this imply? |

|
|
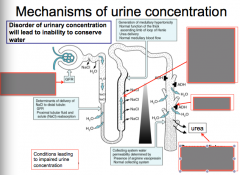
Identify the mechanisms of urine concentration:
|

|
|
|
What are two main causes of hypernatremia?
|
Sodium gains
Increased water losses |
|
|
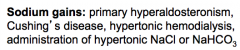
What are causes of sodium gains?
|
|
|
|
What are the two different types of increased water losses?
|
Renal losses
Extrarenal losses |
|
|
What are some examples of renal losses?
|

|
|
|
What are some examples of extrarenal losses?
|

|
|
|
What are the two types of diabetes insipidus? What is the main problem with each?
|
Central DI = lack of ADH
Nephrogenic DI = resistance to ADH |
|
|
What are the types of central DI (think just general terms here)?
|
Congenital and acquired (from brain trauma, infection, or burns)
|
|
|
What are the two types of nephrogenic DI (again just general terms)?
|
Congenital
Acquired |
|
|
What are the mutations in congenital nephrogenic DI?
|
V2 receptor or AQP-2 mutation
|
|
|
What are the four acquired forms of nephrogenic DI?
|
Defect in medullary interstitial tonicity
Defect in cAMP generation AQP-2 downregulation Pregnancy |
|
|
What are some causes of the defect in generation of medullary interstitial tonicity in NEPHROGENIC DI?
|
Chronic kidney disease
Hypokalemia Hypercalcemia Sickle cell disease Protein malnutrition |
|
|
What are some causes of defect in cAMP generation in acquired nephrogenic DI?
|
CKD, hypokalemia, hypercalcemia, demeclocycline, lithium
|
|
|
What are some causes of AQP-2 downregulation in acquired nephrogenic DI?
|
CKD, hypokalemia, protein malnutrition, lithium
|
|
|
What happens in pregnancy to cause acquired nephrogenic DI?
|
Placental synthesis of vasopresinase
|
|
|
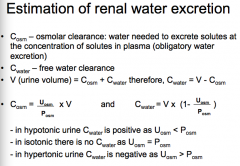
How do you estimate renal water excretion? What is Cosm? What is Cwater? Equation for urine volume?
When is Cwater positive, zero, or negative? |
|
|
|
What defines polyuria? Equation for urine volume? When can V increase?
What could cause Cosm to increase? What could cause Cwater to increase? |

|
|
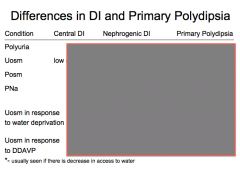
Complete the chart.
|

|
|
|
1. Plasma sodium is primarily regulated by what?
2. Serum osmolality is maintained by what three things? 3. What is always present in true hyponatremia? 4. What develops if there is a compromised thirst mechanism or limited access to water is present? |
1. Changes in total body water.
2. Intact ADH, thirst, renal water handling. 3. Impaired urinary dilution 4. Hypernatremia |

