![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
Under normal physiologic conditions, how does hydrostatic press within vessels relate to colloid osmotic press?
|
They approx balance out. Result = fluid retained in intravascular space (within vessels). |
|
|
Under what 3 conditions can increased V of fluid pass across the vascular wall? |
1. Increased hydrostatic press due to hypertension and/or Na+ retention (hypernatremia). 2. Decreased colloid osmotic press (ie decreased plasma protein conc, esp albumin). 3. Lymphatic and/or venous obstruction. |
|
|
The leakage of what fluid (transudate or exudate) is consistent with edema? |
Transudate (low cell count, few proteins). |
|
|
In acute inflammation, there is a net outflow of fluid from _____, ______, and _____ into extracellular tiss that overwhelms that capacity for resorption by postcapillary venules and lymphatics. |
Arterioles, capillaries, venules. |
|
|
The fluid that forms in extracellular tiss in inflammation is typically an _____. What characterizes this type of fluid? |
Exudate. Increased amount of proteins and cell #s compared to transudate. |
|
|
For transudative effusion:
-appearance? -relative amount of total protein? -relative cell count? |
Clear, light yellow. Low. Low. |
|
|
For modified transudative effusion: -appearance? -relative amount of total protein? -relative cell count? -often seen in what common disease in cats? |
Clear, light yellow. High. Low. FIP yields modified transudate that is high proteins but poorly cellular. |
|
|
For exudative effusion: -appearance? -relative amount of total protein? -relative cell count? |
Turbid, yellow. High. High. |
|
|
What are the 4 main outcomes of the acute inflammatory response? |
1. Resolution 2. Healing by fibrosis 3. Abscess formation 4. Progression to chronic inflammation (often involves macrophagic granulomas). |
|
|
What is a hallmark of chronic inflammation? |
Fibrosis |
|
|
What is chronic inflammation? |
Inflammation of prolonged duration: wks, months, yrs. |
|
|
What are 3 instances when chronic inflammation can occur? |
1. Acute inflammatory response fails to eliminate initial cause. 2. Repeated episodes of acute inflammation. 3. Unique characteristics/virulent factors in inciting substance/microbe, eg mycobacterium in Johne's, fungal bacteria, bacteria hiding in urinary stones. |
|
|
What are some examples of conditions associated w chronic inflammation in animals? |
-various bacterial, fungal, and protozoan infectious agents -autoimmune diseases, eg rheumatoid arthritis, allergic dermatitis -foreign bodies -lick granuloma -EOSINOPHILIC GRANULOMAS OF CATS!!!! |
|
|
Describe eosinophilic granuloma. |
AKA rodent ulcers, linear granulomas. Thick plaques, fibrous tiss along lips. Ropey tissue along back of legs. Filled w macs. |
|
|
Eosinophilic granulomas and other conditions associated w chronic inflammation cause the inflammation via what 4 mechanisms?
|
-persistent +/- resistant infection -isolation -unresponsiveness -autoimmunity |
|
|
Chronic inflammation is maintained by ______. |
inflammatory mediators |
|
|
In chronic inflammation, inflammatory mediators lead to what 5 things? |
1. Infiltration and activation of lymphocytes, macs, plasma cells, and MNGCs. 2. Necrosis 3. Fibroplasia (proliferation of fibroblasts and deposition of collagen) 4. Granulation tiss formation (angiogenesis and neovascularization) 5. Re-epithelialization and tiss repair (initiation of wound healing) |
|
|
True or false?
An abscess may form where acute inflammation fails to eliminate the inciting cause. |
True |
|
|
An abscess is a collection of which cells? |
Predominantly neuts. Also cell debris, macs, fibroblasts, and a variable # of lymphocytes (pus). |
|
|
Describe the role of fibroblasts in abscess formation |
Produce collagen, which forms a thin wall that can become a thicker fibrous capsule --> wall off exudate. |
|
|
Granulomatous inflammation is caused by what? |
Persistence of inciting stimulus for inflammation. |
|
|
True or false? Granulomatous inflammation typically causes minor tissue injury. |
False. It causes extensive tiss injury and necrosis. |
|
|
In granulomatous inflammation there is a shift in inflammatory cells from neuts to what? |
Lymphocytes, macs, and MNGCs. |
|
|
When does a granuloma form? |
When cells in granulomatous inflammation organize themselves into a distinct mass/nodule. |
|
|
What are the cellular components of granulomas/nodular granulomas? |
Central area: macs, epithelioid macs, MNGCs. Outer layer: fibroblasts, lymphocytes, plasma cells. |
|
|
How do caseating granulomas differ from non-caseating granulomas? |
Caseating have central core of necrosis |
|
|
What are 2 common causes of granuloma formation? |
Fungal infections Myobacterium |
|
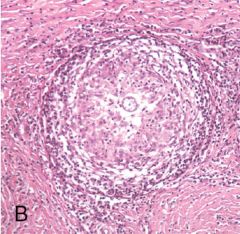
What is this? How do you know? |
Nodular granuloma. Concentric layers. |
|
|
True or false? Abscesses are typically more chronic than granulomas. |
False. Granulomas more chronic. |
|
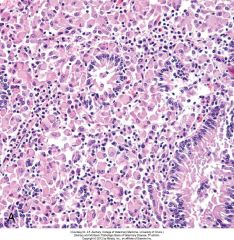
What sort of inflammation is this? Taken from ileum of ruminant w Johne's. |
Diffuse granulomatous inflammation. Note diffuse activated macs (cells w pink nuclei) and lymphocytes, bit of hemorrhage. Note normal epithelial lining vs inflammatory cell pop'n. |
|

What is this in a bovine lung? Could the animal have been treated effectively w antibiotics? Why/why not? |
Abscess. Nope. Drugs can't get in bc fibrous capsule too thick. |

