![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
34 Cards in this Set
- Front
- Back
|
Penicillins, Cephalosporins, Monobactams, and Carbapenems are all what type of antibiotic?
What do they inhibit? |
B-lactams.
Cell wall synth. |
|
|
What rxns in cell wall synth are blocked by B-lactams?
What mediates both of these rxns? How does Penicillin affect this setup? B-lactamase? What are B-lactamases structurally similar to? |
1.) Transpeptidation between Peptidoglycan strands.
2.) Carboxypeptidation of the strands once bound (they want to lose a D-Ala, to permit adding another chain) Penicillin Binding Proteins "prep" the chains for both 1 and 2. Penicillin has a higher affinity for PBPs; it makes a *stable* acyl-enzyme once bound. B-Lactamase can turn penicillin into a *reactive* acyl-enzyme that degrades in water --> inactivated. PBPs. |
|
|
PBPs can mediate which of the following that are essential for cell viability?
- cell elongation - maintainence of cell shape - septum formation during division |
all are mediated by high Molecular Mass PBPs and are essential for cell-viability.
|
|
|
Transglycosylases polyermerize glycan strands.
Transpeptidases cross-link new peptidoglycan. Which processes are penicillin sensitive? |
Transpeptidases are penicillin sensitive, Transglycosylases are not.
|
|
|
Which two properties determine Intrinsic Resistance re: B-lactams?
Extrinsic resistance? |
The affinity of the B-lactam for any one of the essential PBPs of the target organism
The ability of the B-lactam to reach the PBPs in the periplasm of gram (-) bacteria. Presence/absence of reistance mech. - production of B-lactamase - \mem permeability - efflux pump - mut i/essential PBPs |
|
|
B-lacatamase-mediated resistance can be mediated in two ways, what are they and their chief characteristics?
What happens to B-lactamases produced by Gram + bacteria? - bacteria? |
Chromosomally encoded: often inducible
Plasmid-encoded: found on R-factors and trasmitted amongst strains +: excreted into the medium -: retained in the periplasm |
|
|
Staphylococcus aureus strains that produce B-lactamase can be tx'ed with B-lactamase-resistant B-lactamases. Name a few.
What are ESBLs? What are they often the result of? |
Oxacillin, Dicloxacillin; 2nd/3rd gen cephalosporins
nosocomial strains have arisen that produce β-lactamases that hydrolyze previously hydrolysis-resistant antibiotics - Often results from a single point mutation |
|
|
In which type of bacteria can porins mediate resistance? How do/can they do it?
|
Gram -
1) porins can be altered (mut in constriction loop or barrel) resulting in a decrease in rate of permeation of the antiB 2) deletion of the only pore through which the AntiB can permeate through - ex: pseudomonas aeruginosa |
|
|
_____ ______ contributed to resistance to B-lactams in Pseudomonas, Salmonella, and Neisseria.
In Neisseria, resistance is mediated by a mut in the _____ region that relieves repression and promotes over-expression of the _____ _____. |
Efflux pumps
promoter region; efflux pump. |
|
|
Mutations of PBPs can cause a decrease in the rates of inactivation by B-lactams. How do these altered PBPs evolve? Observed in which organisms?
Do all of these aa changes decrease inactivation by the antibiotic? |
recombination w/ DNA from commensal (non-path) species
Staph aureus, strep pneumo, and neisseria gonorrhoeae no, only some. |
|
|
What is PRSP? Characteristics?
Is it resistant to anything else? Tx? (3) |
Penicillin resistant Strep pneumo
contains muts in ALL of the essential PBPs that lower their inactivation rate by B-lactams. Yes, many other antiBs too. currently tx'ed w/ vancomycin (+ cefotaxime), linezolid, or streptogramins. |
|
|
How does Neisseria become resistant to Penicilin? (2)
How can resistances be transferred from a resistant strain to a sensitive strain? Do efflux overexpression or muts in porin confer marked resistance alone? Are the genes transferred randomly? Tx'ed? |
1. Plasmid-med prod. of B-lactamase
2. Chromosomal muts in endogenous genes (PBPs, porins, efflux pumps) chromosomal resistance genes can be transferred by homologous recombination. No. When combined they DO confer marked resistance. No, in a specific order. ceftriazone or cefixime (ciprofloxacin, tetracycline, and penicillin are no longer effective) |
|
|
mut PBP1 --> increased efflux pump expression --> mut in porin --> mutations in PBP1
The above describes the stepwise progression of antiB resistance genes in which organism? Resistance mechanisms in this organism are chromosomally mediated, and require the presence of which gene? How was it created? |
Neisseria gonorrhoeae.
mosiac penA gene (encodes an essential PBP). - created in nature by recombination w/ commensal species. |
|
|
MRSA strains acquired what from an unkonwn source that displays extremely low rates of acylation w/ virtually all B-lactam antiBs? In strains with this, what is the *ONLY* drug target?
Can B-lactams be used to tx MRSA? Tx? (3) |
new PBP (PBP 2a)
PBP 2a. No. Canvomycin, Linezolid, or Dalfopristin/Quinupristin. |
|
|
What is Panton-Valentine leukocidin? What carries this in high %? What does it cause?
|
a cytotoxin that causes leukocyte destruction and tissue necrosis
CA-MRSA severe necrotizing hemorrhagic pneumonia |
|
|
As the acylation rate of PBPs decreases, what increases?
|
their resistance to B-lactam antiBs (higher MICs)
|
|
|
What are the modes of B-lactam resistance in Gram - bacteria? +?
|
mut in porin, mut in PBP, B-lactamase prod, efflux pump overexpression
B-lactamse (excreted into media), alterations in PBPs, inability to activate autolysins. |
|
Fill in the B-lactams that are active in the following spectrums. Say them out loud.
|
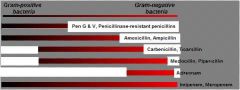
From top to bottom:
- penG&V, Penicillinase resistant penicillins - Amox and Amp - Carbenicillin, Ticarcillin - Mezlocillin, Pipericillin - Aztreonam - Imipenem, Meropenem |
|
|
Given the targets, give useful things for Tx'ing:
Neisseria meningitidis sensitive strep pneumo enterococci (combined w/aminoglycoside) Syphillis Staph aureus, but not MRSA. |
Pen G & V
Penicillinase-resistant penicillins |
|
|
Which penicillins can be used to Tx all of the following?:
UTIs (e.coli), otitis media and RTIs (h.influ & sensitive strep pneumo) Listeria |
Amoxicillin and Ampicillin (oral)
|
|
|
Proteus mirabilis, pseudomonas aeruginosa, serratia marcescens, and klebsiella pneumoniae are all difficult to tx gram (-) bacteria. Which B-lactams are used to tx and how are they used?
|
Ticarcillin, Pipericillin, Mezlocillin, in combo w/ aminoglycoside
|
|
|
What is the broadest Spectrum B-lactamase available? When is it used?
What is it hydrolzed by in mammals? Result? |
Impenem
- serious infect of unknown origin - mixed infections renal dipeptidase; it is marketed with cilistatin (a renal dipeptidase inhibitor) |
|
|
How does pseudomonas aeruginosa become resistant to Imipenem?
|
deletion of a porin
|
|
|
What are Clavulanic Acid and Sulbactam? What do they do? Are they antibacterial as single agents? Examples?
Can resistance develop? how? |
B-lactamase inhibitors
irreversibly b/ B-lactamases and inhibit activity. no, activity is poor. Augmentin (Amox + clavulanate) Unasyn (Amp + sulbactam) Yes, mut in B-lactamase. |
|
|
What is the spectrum of effectiveness for the following generations of cephalosporins:
1st 2nd 3rd - give generic drug name examples of the classes. Which is usefuly in txing... i) gonorrhea ii) CA-skin infections iiI) CA-pneumonia caused by h. influ or klebsiella Which penetrates the CNS, and is useful for meningitis caused by Gram -'s? |
1st: mostly +; cephalexin
2nd: in the middle; cefuroxime 3rd: mostly -; ceftriaxone, Cefotaxime 3rd, 1st, 2nd 3rd |
|
|
Are B-lactams metabolized? How are they excreted? Are they widely or narrowly distributed?
Rapidly or slowly eliminated? Average half-life? Exception? Quick fix? |
No, urine, widely. (remember policeman example)
Rapidly via glomerular filtration. ~30-120min cetriaxone: 8hrs co-admin an oral probenicid, which blocks renal tubular secretion. |
|
|
Are penicillins typically toxic?
What is the most common ADR of penicillins? If rxn is seen to one, is it likely rxns will occur to others? Exception that does not provoke hypersensitivity rxns? |
no, among the least toxic because their target has no mammalian counterpart.
hypersensitivity (rash, fever, bronchospasm, anaphylaxis) Yes. Aztreonam |
|
|
Almost all _____ antiBs produce intense local pain upon IM injection. Some of them can also cause _____ disorders. how? Way to avoid this?
|
cephalosporins
Bleeding disorders (cefotetan, cefoperazone, cefamandole) - side chain interference with prothrombin formation Co-admin vit K. |
|
|
Which types of ADRs are most common w/ the cephalosporins?
T/F: Patients with a mild allergy to penicillin may be able to tolerate a cephalosporin Patients with a history of anaphylaxis should never receive cephalosporins |
hypersensitivity
T, T. |
|
|
2nd and 3rd generation cephalosporins carry a high risk of what?
The ceph's that can cause bleeding disorders can also produce what? |
superinfections.
disulfiram-like rxn (nausea, vomiting) in conjunction w/ alcohol. |
|
|
Is Vancomycin more useful w/ Gram + or -? why?
|
+; does not readily penetrate the outer membrane of gram - bacteria.
|
|
|
What is used to tx this following constellation of infections (also give method of admin):
MRSA Enterococcus faecium and E. faecalis Penicillin-resistant Strep Pneumo Pseudomembraneous colitis caused by Clostridium difficile. |
Vancomycin
all IV, except for Psuedomembraneous colitis = orally b/c it is not absorbed from the GI tract. |
|
|
High lvl, plasmid mediated vancomycin resistance is often found in what? (2) Most prominent by far?
What induces this resistance? Mechanism? |
Enterococcus faecalis and E. Faecium (VREs).
E. Faecium. Vancomycin itself. replacement of D-Ala-D-Ala C- w/ D-Ala-D-Lactate --> no longer b/ vancomycin with high affinity. |
|
|
How do you end up with VISA and VRSA staph aureus?
Mech? What have these strands obtained? how? Are VISA and VRSA strains still resistant to other antiBs? What would super-suck? |
prolonged exposure (25d to 18w) to vancomycin
Thickening of cell wall that traps the antiB in the outer layers. vanA; horizontal transfer of transposon. Yes. Vanco resistant MRSA. |

