![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
What are obligate intracellular pathogens? What does this mean re: drug tx?
|
viruses; drugs must penetrate into cells to be effective.
|
|
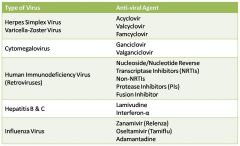
Put in the txments
|
|
|
|
Poxviruses, Herpesviruses, Adenoviruses, Hepadnaviruses, and Papillomaviruses are all what type of viruses?
|
DNA
|
|
|
Rubella virus, rhabdovirus, arenaviruses, arborviruses, orthomyxoviruses, and paramyxoviruses are all what types of viruses?
|
RNA
|
|
|
I'm giving the drug, give the stage of viral lifecycle it blocks:
Protease inhibitors NRTIs, NNRTIs Rimantadine Acyclovir Admantadine Interferon-a Enfuvirtide Neuramidase inhibitors Palivizumab Acyclovir Foscarnet Docosanol Entecavir |
Viral attachment/entry:
- enfuvirtide, docosanol, palivizumab Penetration: - interferon-a Uncoating: - Admantadine, Rimantadine Nucleic acid synth - NRTIs, NNRTIs, Acyclovir, Foscarnet, Entecavir Late protein synth/processing: - Protease inhibitors Packaging/assembly/release: - neuramidase inhibitors |
|
|
What agents are used to tx herpes simplex & varicella-zoster virus infections?
- what does it need for actv? - What is the difference between the two agents? What viral enzyme ensure selectivity? |
Acyclovir and Valacyclovir
- phos'ed to triphosphate form - Valc. is the prodrug form of Acyc. that is converted in intestine and liver. viral TKase converts these to monophosphate derivative w/ 100x selectivity. |
|
|
What are the three ways Acyclovir and Valacyclovir inhibit DNA synth?
|
Competition with dGTP for the viral DNA polymerase
Incorporation into and termination of the growing viral DNA chain Inactivation of the viral DNA polymerase |
|
|
What are the pharmacoKinetics of Acyclovir and Valacyclovir?
Toxicities? Resistances? |
Given topically, orally, or IV
Valacyclovir achieves 3-5x conc. when given orally Virtually none at normal doses. Alterations in either viral TKase or viral DNA polymerase. |
|
|
CMV reactivations leading to:
CMV retinitis Colitis CNS dz Esophagitis Pneumonia .... are common in what pt population? |
AIDS pts.
|
|
|
How do we tx CMV?
- similarities to Acyclovir and Valacyclovir? - Which of the two is preferred orally? - Most common SE? Do we also see nausea, diarrhea, fever, rash, HA, etc? - mech of resistance? |
Ganciclovir and Valganciclovir
- basically the same but have an additional CH2OH group - Valganciclovir; b/c of higher serum concentrations. - myelosuppression; yes, we see these as well. decrease in formation of the triphospate form muts in DNA polymerase |
|
|
What is Phosphonoformic acid?
- mech? - does it require phos to be actv? - uses? - Toxic to kidneys? Liver? Effects on ions? HA, hallucinations and seizures? - resistances Can it still be used in ganciclovir resistant CMV? |
Forcarnet
- inhibits DNApoly @ diff site than acyc or gancic. - no, it doesn't. - CMV retinitis w/ gancic; HSV&VZV that are acyclovir resistant. - Nephrotoxicity, messes w/ calcium lvls (up or down), kypokalemia, hypomagnesemia .... HA, hallucinations, and seizures --> yes. point mutations in DNA polymerase. Yes. |
|
|
Amantadine and rimantadine effect which influenza strains?
|
H5N1; H1 & H3
|
|
|
How does amantadine work?
Uses? SE? Resistances? |
blocks M2 proton channel; prevents virus from acidifying/uncoating it's RNA
- very effective prophylaxis, reduces duration of Sx - GI distress, CNS effects - point mut in M2 proton channel |
|
|
What are Zanamivir (Relenza) and Oseltamivir (Tamiflu)? Work against influenza A or B?
When must they be given? Administration? Side effects (diff for each)? Resistance? |
sialic acid deriviatives that act as neuramidase inhibitors.
- Both. - early on - Zanamivir --> inhalation - Oseltamivir --> orally Coughing, bronchospasm (zanamivir) CNS effects (oseltamivir) Rarely observed worldwide. |
|
|
What is HAART?
What are the four classes of antiretrovirals that are available for use? |
Highly Active AntiRetroviral Therapy.
NRTIs NNRTIs Protease inhibitors Fusion inhibitors |
|
|
What are the three NRTIs I should know?
- mech? - Side effects? |
Abacavir, Lamivudine (3TC), and Zidovudine (AZT)
- compet. inhib of HIV rev. Transcriptase & cause chain termination when incorporated into viral DNA. - mitochondral toxicity, - increases risk of lactic acidosis with hepatic steatosis - lipid metabolism disorders |
|
|
NNRTIs (3)?
- mech? - b/ site re: NRTIs? - require phos? - general SEs? + which two should be avoided in pregnancy? - All three are substrates of what? + which is an inhib? inducer? mixed? |
Delaviridine, Efavirenz, Nevirapine
- inhibit HIV rt. - close but distinct - no. - skin rash, GI intolerance - delaviridine and efavirenz - CYP3A4 + inhib: delaviridine; induc: nevirapine; mix: efavirenz |
|
|
What are the two protease inhibitors I should know?
- mech? - result? - Which can cause increased spontaneous bleeding in pts with hemophilia A or B? How about a redistribution & accumulation of body fat? - all PIs are substrates of what? - How is this useful? |
Atazanavir and Lopinavir/Ritonavir combo
- block cleavage of Gag-Pol polyprotein --> structural proteins can't be produced in mature viron core. - immature, non-infectous particles. - all three; Lopinavir/Ritonavir - CYP3A4 - subtherapeutic doses of ritonavir inhib CYP3A4 --> \met of lopinavir --> ^blood lvls of lopinavir. |
|
|
What is Enfuvirtide?
- mechanism? - used when? - SE? - $? |
Fusion inhibitor
- b/gp41 in viral particle membrane, prevents fusion with host membrane. - in combo w/ other drugs - local injection site rxns, eosinophilia - very $$$ |
|
|
What is a new integrase inhibitor?
- mech? - resistance? - when used? |
Raltegravir
- targets integrase that gets the viral DNA into the host genome - mut of integrase - only in combo w/ other drugs |
|
|
What is CCR5? What is Maraviroc?
Did resistance occur anyway? Uses? |
- CCR5 is the coreceptor for HIV viral entry
- antagonist of CCR5 - yes, some viruses have mutated to use CXCR4 instead of CCR5 for a co-receptor Only in combo w/ other drugs. |
|
|
What is used to tx Hep B and C infections?
- mech? - what 4 things happen as a result? |
interferon-a
- increases synth of proteins that lead to host viral resistance. - these proteins inhibit: 1) synth of mRNA 2) translation of viral proteins 3) protein processing 4) viral assembly and release |
|
|
How is interferon-a administered? What does pegylation do?
- Therapeutic uses of interferon-a? - SE? + contraindications? |
subQ or intraM
- lengthens the time for elimination - HBV, HCV, Papillomavirus infections - Flu-like syndrome that resolves upon continued administration - neurotoxicity - abortifacient in primates **PREGNANCY*** see above |

