![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
Name the disorders of the sclera and episclera. |
• Episcleritis • Scleritis • Scleral Discolouration |
|
|
What is the episclera? |
Covers the sclera |
|
|
Where does the episclera lie? |
Connective tissue that lies between the superficial scleral stroma and Tenon’s capsule. |
|
|
What does the episclera contain? |
Contains numerous blood vessels that nourish the sclera |
|

What is this? |
Episcleritis |
|
|
What is episcleritis? |
Benign, inflammatory condition
• no infection present; so no stringy discharge/pus • normally idiopathic, infrequently a systemic association exists |
|
|
Who does episcleritis commonly affect? |
30-40 year olds Males slightly < F |
|
|
What are the signs of episcleritis? |
• Acute onset redness, often confined to one area • 70% of cases are unilateral (unlike conjunctivitis) • Sometimes no symptoms • VA usually normal • Cornea & Anterior Chamber clear • ES often looks worse than it is! |
|
|
What are the symptoms of episcleritis? |
• Symptoms vary considerably • ‘Mild pain’, ‘FB sensation’, ‘Burning’ or ‘Tenderness’ • Photophobia and watery discharge also common |
|
|
What are the 2 types of episcleritis? |
Simple ES Modular ES |
|
|
Which type of episcleritis is more common? |
Simple ES more commonly |
|
|
How can simple episcleritis appear? |
Can be sectoral (70%) or diffuse (30%) |
|
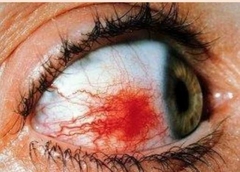
What is this? |
Simple ES sectoral |
|

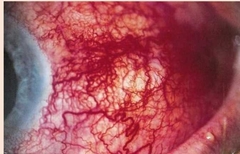
What is this? |
Simple ES diffuse |
|
|
How would nodular episcleritis appear? |
• Translucent white nodule within inflamed area (freely movable) • More painful than simple ES • Greater likelihood of systemic involvement |
|

What is this? |
Nodular ES |
|
|
What is the treatment for Episcleritis? |
• Most cases self-limiting (resolution in 2 or 3 weeks) • Can use simple lubricants in mild cases • Topical steroids e.g. prednisolone • Only effective if used early • Oral non-steroidal anti-inflammatory agents (NSAIDs) e.g. Flurbiprofen |
|
|
Why would episcleritis reoccur? |
Systemic involvement? In particular: inflammatory bowel disease, ulcerative colitis & Crohn’s disease |
|
|
What is Scleritis? |
• Sclera undergoes inflammation, oedema and sometimes necrosis • Covers the spectrum of seriousness: may be trivial, self-limiting or a potentially blinding condition |
|
|
Is scleritis common? |
Much less common than episcleritis |
|

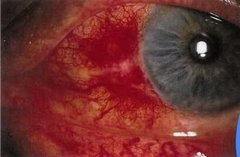
What is this? |
Scleritis
Note there is no limbal flush like anterior uveitis |
|
|
How would scleritis develop? |
Typically less acute in onset than ES (e.g. develops over days) |
|
|
What would you see with Scleritis? |
• As well as dilation of scleral vessels, there is also dilation of bulbar conjctiva & episcleral vessels • Anterior chamber reaction often present |
|
|
What is Scleritis associated with? |
• Scleritis is associated with systemic collagen disease • Around 50% of cases have systemic involvement e.g. RA, lupus |
|
|
When can scleritis occur. |
After glaucoma surgery |
|
|
Who does scleritis affect? |
• Typically Affects older age group than ES • Pxs. Typically, 30-60, peak in 40’s. • F>M (1.6 to 1) |
|
|
What are the signs of Scleritis? |
• Bilateral in ~50% of cases • Deep purplish ocular injection on presentation • Like ES, it can be segmental or diffuse • VA can be normal or reduced • But VA often reduced in posterior scleritis |
|
|
What are the symptoms of Scleritis? |
• Pain (deep, ‘stabbing sensation’), often worse at night • Sometimes pain can be falsely localised (appearing peri-orbital or even temporal) • Photophobia & excessive lacrimation are also common. |
|
|
What are the 2 types of Scleritis? |
Anterior scleritis 98%
Posterior scleritis 2% |
|
|
Name the types of anterior scleritis |
Necrotising 13% Non necrotising 85% |
|
|
What are the types of non necrotising anterior scleritis. |
Diffuse Nodular |
|
|
What would be seen with diffuse non necrotising scleritis? |
• In diffuse variety, eye is completely reddened (purplish haze) • Most common type & most benign • Eye feels very tender |
|
|
What would be seen with nodular non-necrotising anterior Scleritis? |

• Non-mobile nodules on the surface of sclera • Nodules correspond to points of focal inflammation & oedema |
|
|
What are the types of necrotising Scleritis? |
With inflammation
Without inflammation |
|
|
What is Necrotising AS without inflammation: (scleromalacia perfornas)? |

• Associated with RA • Insidious and painless “melting” away of the sclera • Rupture of the globe is possible |
|
|
Describe Necrotising AS with inflammation. |
• White avascular areas surrounded by areas of scleral reddening
• Ischaemic areas thin over time |
|
|
What is common with Necrotising AS with inflammation? |
• Anterior Uveitis • Glaucoma • Cataract |
|
|
What is posterior scleritis? |
• Extremely rare but extremely serious
• Painful proptosis & diplopia
• Restriction of eye movements & lid swelling also possible
• Anterior segment may appear normal |
|
|
What happens to the globe with posterior scleritis? |
Posterior globe flattens |
|
|
What happens to the vision with posterior scleritis? |
Visual loss usually severe |
|
|
What is the treatment for Scleritis? |
• Refer for medical (systemic association) & ophthalmological investigation • Urgent referral to Ophthalmologist required in necrotising AS and in PS
• Topical steroids may be of palliative help only • Oral NSAIDs (e.g. ibuprofen) usually tried first
• If inflammation doesn’t respond, systemic steroids tried next
• Immuno suppressants prescribed in necrotising scleritis and in PS • Sometimes also in other forms of the condition when steroids alone don’t work |
|
|
How do you distinguish episcleritis from scleritis? |
• How quickly did the condition develop • Ask about systemic conditions • Blanching technique: instil 2.5% phenlyephrine
• In ES, vessels radiate posteriorly from limbus. • They criss-cross in scleritis
• Vascular mobility: in ES vessels can be moved over sclera using cotton-tip • Nodular mobility: nodular ES versus nodular scleritis |
|
|
What would be seen with the blanching teqnique to distinguish between episcleritis and Scleritis? |
Episcleral & conj vessels will narrow |
|
|
Why would there be scleral discolouration? |
Often due to systemic conditions |
|
|
Name the focal scleral discolourations? |
• Senile scleral translucency (oval grey areas) • Alkaptonuria (black-brown) • Haemochromatosis (rust-brown) • Metallic foreign body (rust staining) • Systemic Minocycline (blue-grey in para-limbal areas) |
|
|
What is diffuse scleral discolouration? |
• Sclera has an overall blue or yellow colour... • Jaundice (yellowing) • Conditions that lead to thinning & increased transparency of sclera (blue due underlying uvea) |

