![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
108 Cards in this Set
- Front
- Back
|
Where is GnRH released from? |
The hypothalamus |
|
|
Where are FSH and LH released from? |
The anterior pituitary |
|
|
What does FSH do? |
-FSH stimulates the ovary to produce estradiol/ estrogen -Causes follicle growth in the ovaries (immature eggs) |
|
|
Describe estradiol positive and negative feedback |
-Estradiol will be released by the growing follicle. Estradiol causes a negative feedback of FSH. -Estradiol causes a positive feedback on LH |
|
|
What does LH do? |
Causes the release of progesterone |
|
|
What are the three phases of the menstrual cycle? How long does each last? |
1. Follicular (day 1-13/14) 2. Ovulatory (16-32 hrs) 3. Luteal (14 days total) |
|
|
When does mittleschmerz occur? |
During the ovulatory phase |
|
|
What is the corpus luteum? What is the role of it? |
a. Corpus luteum: a hormone-secreting structure that develops in an ovary afteran ovum has been discharged but degenerates after a few days unless pregnancyhas begun.b. The corpus luteum will secrete largeamounts of estrogen and progesterone and prepare the uterus for fertilization c. Progesterone causes the endometrium tothicken, filling with fluids and nutrients to nourish the potential embryo. Inaddition, it will cause mucus in the cervix to thicken, so that sperm andbacteria are less likely to enter the uterus. Will also increase basal bodytemperature by 0.5-1.0 degrees F --> returns to baseline when progesteronesecretion stops |
|
|
During which phase of the menstrual cycle does a person bleed? |
Follicular phase |
|
|
What drugs are used for a medical abortion? Describe the MOA of each |
Mifeprostone & Misoprolol -Mifeprostone: progesterone antagonist. W/o progesterone, the uterine wall will slough off -Misoprolol: prostaglandin analog - will lead to uterine contraction |
|
|
What is the difference b/w menorrhagia and metrorrhagia? |
-Menorrhagia: Heavy or prolonged bleeding -Metrorrhagia: bleeding b/w menstrual cycles |
|
|
When should you perform an endometrial biopsy? |
-Endometrium >4cm -Women >35 y/o who are amenorrheac to r/o endometrial hyperplasia or carcinoma |
|
|
How should you tx acute heavy bleeding? |
-High dose IV estrogens -Followed by high dose OCP that is tapered until bleeding stops -If high dose IV estrogen fails, perform D&C |
|
|
Describe primary vs secondary amenorrhea |
1. Primary amenorrhea: -Failure of onset of menses & no development of 2/2 sex characteristics @ 13 y/o -Failure of onset of menses w/ development of 2/2 sex characteristics @ 15 y/o 2. Secondary amenorrhea: absence of menstruation x 3 mo's w/ previously nl menstruation |
|
|
What are the causes of primary amenorrhea in those WITH 2/2 sex characteristics? |
Uterus present: -Outflow obstruction (imperforate hymen, transverse vaginal septum) Uterus absent: -Mullerian agenesis -Androgen insensitivity |
|
|
What are the causes of primary amenorrhea in those WITHOUT secondary sex characteristics? |
Ovarian causes: -Premature ovarian failure -Gonandal dysgenesis Non-Ovarian causes: -hypothalamus pituitary failure -Puberty delay (anorexia, illness, athlete) |
|
|
What occurs with unopposed estrogen? |
-Proliferation of the endometrium -No progesterone to cause shedding |
|
|
What is the initial lab workup for amenorrhea? |
-Pregnancy test -Serum prolactin -FSH/LH -TSH |
|
|
What is cryptomenorrhea? |
-Menses occurs but is unable to exit the vaginal due to outflow obstruction (ex: intact hymen, transverse vaginal septum) |
|
|
What are teh S&S of cryptomenorrhea? |
-On vulval inspection: a tense, bulging, bluish membrane is seen -On rectal examination: a large bulging mass is felt. |
|
|
What are the hypothalamus pituitary dysfxn causes of secondary amenorrhea? |
-Dz of hypothalamus or pituitary -Anoerxia/ exercise -Severe bodily stress |
|
|
How do you tx hypothalamus pituitary dysfxn causing secondayr amenorrhea? |
-Stimulate GnRH production using clomiphene |
|
|
What is the role of prolactin? What does it inhibit? What inhibits prolactin? |
-Role: aids in mammary gland development and milk secretion in pregnancy -Inhibits: GnRH secretion -Inhibited by: Dopamine |
|
|
What will the labs of someone with a prolactinoma look like? |
-Remember*: prolactin inhibits GnRH, however there is no direct way to measure GnRH -Low FSH/LH -High Prolactin levels |
|
|
What are the S&S of estrogen deficiency? |
-Hot flashes -Sleep/ mood disorders -Vaginal atrophy/ dryness -Thin/ dry skin -Dyspareunia |
|
|
What is Asherman's syndrome? |
-Uterine scarring 2/2 postpartum hemorrhage, D&C, or endometrial infection |
|
|
When is adenomyosis? |
-Growth of endometrial tissue in the myometrium -Different from endometriosis bc endometriosis is growth of endometrial tissue OUTSIDE the uterine cavity |
|
|
What is the average age of dx in adenomyosis? |
-35-50 y/o |
|
|
What are the S&S of adenomyosis? |
-Menorrhagia -Dysmenorrhea -Dysparenunia -*Uniformly enlarged, boggy uterus* |
|
|
How do you tx adenomyosis? |
-MRI/US -G.S: post- TAH |
|
|
What is endometritis? |
-Infection of the endometrium during pregnancy or post-partum -If no pregnancy, called PID |
|
|
What are the MC bacterial causes of endometritis? When do these infections usually occur? |
Bacteria: -GABHS -S. Aureus Timing: -S/P C-Sec = MC due to retained uterine products -S/P Vaginal delivery |
|
|
How do you try and prevent endometritis during C-Sec? |
-Give one dose of 1st gen cephalosporin |
|
|
How do you tx endometritis? |
-C-Sec: Gentamicin & clindamicin -Vaginal delivery/ chorioamnionitis: ampicillin + gentamicin |
|
|
What is the MC area for endometrial tissue to travel to in pt's with endometriosis? |
-Ovaries |
|
|
What is the MC cause of infertility? |
-Endometriosis |
|
|
How do you tx endometrial hyperplasia w/o atypia? |
-Progesterone tx PO or via IUD -Recheck endometrial thickness in 3-6 mo's |
|
|
What is the MC gynecological malignancy in the US? |
Endometrial CA |
|
|
What are causes of inc estrogen exposure? |
-Nulliparity -Chronic anovulation -Obesity -ERT -Tamoxifen |
|
|
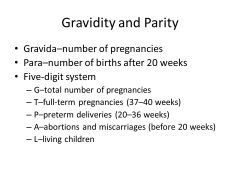
Describe the gravidity parity system |
|
|
|
How do you dx menopause? |
-Inc serum FSH/LH -Dec serum estrogen |
|
|
What drug induces ovulation? |
-Clomiphene |
|
|
How do you tx stress incontinence? |
-Pelvic floor exercises -Alpha agonists: Midodrine, pseudoephedrine -Surgery |
|
|
What is the cause of urge incontinence? |
-Detrusor mm overactivity... detrusor mm forms the wall of the bladder -AKA overactive bladder |
|
|
How do you tx overactive bladder/ urge incontinence? |
-Bladder training -Anticholinergics: 1st line - Tolterodine, propantheline. 2nd line - oxybutinin |
|
|
What GYB cancer has the highest mortality? |
-Ovarian CA -Rarely sx until late in the dz course |
|
|
What serum marker can be used in ovarian CA to monitor progress? |
CA-125 |
|
|
What is the MC benign ovarian neoplasm? |
-Dermoid cystic teratomas |
|
|
What are possible complications of PCOS? |
-Infertility -Inc risk endometrial hyperplasia -Inc risk endometrial CA |
|
|
How do you tx hirsuitism in PCOS? |
Spironolactone |
|
|
What HPV is MC associated with Cervical CA? |
-16 & 18 strains |
|
|
What is the first sx of cervical CA? |
-Post coital bleeding/ spotting |
|
|
What are the RF for cervical insufficiency? |
-Hx of cervix trauma or procedure -Multiparity -Abnl uterus -DES exposure in utero |
|
|
How do you tx cervical insufficiency? |
-Weekly progesterone injections OR -Cerclage |
|
|
What is the MC sx of vulvar CA? |
Itching |
|
|
What are the signs seen on exam in trichomonas infection? |
-Frothy yellow/ green discharge -Strawberry cervix |
|
|
How can you tx chlaymdia? |
-Azithromycin 1 g 1x OR -Doxycycline 100 mg BID x 7 d's |
|
|
How can you tx gonorrhea? |
-Azithromycin 1 g 1x AND -Ceftriaxone IM 250 mg 1x |
|
|
What causes a chancroid? |
Haemophilus ducreyi |
|
|
What are the S&S of a chancroid? |
-Painful genital ulcer -(+/-) foul smelling d/c from the ulcer -Painful inguinal LAD |
|
|
How do you tx chancroid? |
-Azithromycin 1 g 1x OR -Ceftriaxone 250 mg IM 1x |
|
|
What is a potential complication of PID? |
Fitz-Hugh Curtis syndrome |
|
|
What exam findings are necessary to dx PID? |
1. Abd tenderness 2. Adnexal tenderness 3. Cervical motion tenderness |
|
|
What is the MC cause of TSS? |
S. Aureus |
|
|
What are the S&S of TSS? |
-Sudden onset fever, tachycardia pharyngitis -Diffuse macular rash, palms & soles included, resembling sunburn |
|
|
If someone has WBC casts on UA and UTI sx, what does this indicate? |
Pyelonephritis!!!!! AH!!!! |
|
|
How do you tx an ectopic pregnancy? |
-Unruptured: methotrexate
-Ruptured: laparoscopic salpingostomy |
|
|
What is true for bHCG levels in ectopic pregnancy? |
Will fail to double in 24-48 hrs |
|
|
What is the MC cause of mastitis? |
S. Aureus |
|
|
How should you tx mastitis w/o abscess? |
-Warm compresses -Abx: dicloxacillin, clindamycin, or keflex -Can continue to breast feed from the affected breast |
|
|
What will a biopsy of fibrocystic breast disorder show? |
Straw-colored fluid |
|
|
Where is the MC location of breast CA? |
Upper outer quadrant |
|
|
Where does Breast CA mets to? |
-Liver -Lungs -Bone -Brain |
|
|
What is the MC type of breast CA? |
Infiltrative ductal carcinoma |
|
|
What is paget's disease of the breast? |
-Found in breast CA -chronic eczematous, itching, scaling rash on the nipple and the areola |
|
|
When may you see an abnormally high hCG? |
Choriocarcinoma |
|
|
What is the role of progesterone during pregnancy? |
–Relaxes smooth muscle (the uterus) –Inhibits uterine contractions therebypreventing spontaneous AB |
|
|
Where is oxytocin produced? |
The posterior pituitary |
|
|
What is the role of oxytocin in pregnancy? |
-Stimulates uterine contractions andpotentially preterm labor... artificial oxytocin is used to induce labor -Responsible for the milk ejection reflex whennipples are stimulated |
|
|
What tests should be done during an initial prenatal visit? |
-Pelvic (pap smear) -G/C culture -UA for UTI -CBC – anemia -Rh status -screen and type -hCG, -RPR, -hepatitis -rubella immunity, chicken pox immunity -HIV -Ifat high risk for gestational DM, test may be done at first visit |
|
|
Is Rh (+) or (-) more troublesome? |
-RH (-) is more troublesome, if not first pregnancy must give Rhogam @ 28 wks |
|
|
When can you begin to hear fetal heart tones? |
10-12 wks |
|
|
When is first screen? |
-10-12 wks -US that tests for Trisomy 21 (DS) and Trisomy 18 (Edwards) |
|
|
When should a pregnant woman begin to feel movement? |
15-20 wks |
|
|
When can you determine a babies sex?
|
18-20 wks via US |
|
|
When should you do a GBS swap? |
-35-37 wks |
|
|
What is dystocia? What are the types? |
Dystocia = abnl labor progression 1. Power: uterine contractions 2. Passenger: abnl fetal positioning 3. Passage: abnl maternal anatomy |
|
|
How can you tx shoulder dystocia? |
-McRobert's manuever -Wood's "Corkscrew" maneuver |
|
|
What is a molar pregnancy vs choriocarcinoma? |
-Molar pregnancy: abnormal gestational tissue resulting in a non-viable pregnancy -Choriocarcinoma: occurs when the tissue becomes malignant |
|
|
What are the types of molar pregnancy? |
-Complete: Egg w/ no DNA is fertilized by 1-2 sperm. Inc risk of choriocarcinoma w/ this type -Partial: Egg w/ DNA is fertilized by 2 sperm. |
|
|
What are the S&S of hydratiform mole? |
-Bleeding/ brown d/c: occurs at 6 wks-5 mo's. -Abnl size/ date of uterus: larger than expected. -Hyperemesis gravidum: from inc. amount of BHCG |
|
|
How do you dx hydratiform mole?
|
-Labs: MARKEDLY increased BHCG; low AFP -US: "snowstorm"/ "cluster of grapes" appearance |
|
|
How do you tx molar pregnancy & choriocarcinoma? |
-Molar pregnancy: uterine suction curettage -Chorio: Methotrexate -MUST FOLLOW BCHG LEVELS WEEKLY TO ENSURE DECREASE |
|
|
When do you test for gestational DM? |
24-28 wks |
|
|
When should you deliver a child if the mother has gestational DM? |
-38 wks |
|
|
When do you give rhogam? |
-28 wks -Again w/in 72 hrs before delivery -Any abnl bleeding ` |
|
|
What are tocolytics? What are the purpose of them? Name examples. |
-Tocolytics: inhibit uterine contractions. Given 48 hr before premature delivery. -Purpose: allow for exogenous steroids to take full action on fetus. -Ex's: Terbutaline, ritodrine, MgSO4 |
|
|
When should you not give a tocolytic? |
Intrauterine infection |
|
|
What anti-emetic drug is first line in pregnancy? |
-Pyridoxine |
|
|
What is placental previa? What are the types? |
-Abnormal positioning of the placenta over the cervix -Marginal: 2-3 cm away from cervix -Partial: partially covering the cervix -Complete: fully covering the cervix |
|
|
What are the S&S of placenta previa? |
-PAINLESS, bright red bleeding in the 3rd trimester -Bleeding will cease in 1 hr -No abd or uterine pain -Soft uterus |
|
|
How do you tx placenta previa? |
-Hospitalization for stabilization -Tocolytics until exogenous steroids kicked in for fetus |
|
|
What is abruptio placentae? |
When the placenta immaturely separates from the uterine wall |
|
|
What are the RF for abruptio placentae? |
-MATERNAL HTN = MC -Cocaine use -ETOH -Smoking -Folate deficiency |
|
|
What are the S&S of abruptio placentae? |
-PAINFUL, dark red blood that does not stop -Abd pain -Rigid uterus -Fetal bradycardia = fetal distress |
|
|
What is the tx for abruptio placentae? |
-Immediate delivery |
|
|
What is HELLP syndrome? |
Develops during pre-clampsia -H: hemolytic anemia -E & L : elevated liver enzymes -L & P: low platelets |
|
|
What HTN drugs are safe in pregnancy? |
-Labetalol -Methyldopa -Hydralazine -Nifedipine |

