![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
17 Cards in this Set
- Front
- Back
|
Division of Liver blood flow and circulation |
60-70% Portal vein 30-40% Hepatic artery Peculiarity -> Blood flows from one capillary to the other (portal vein -> hepatic vein) |
|
|
Liver lobule anatomy |
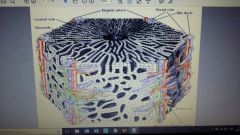
No fibrous tissue |
|
|
Which stain we need to use to highlight reticulin fibers? |
Silver stain -> Reticulin network highlights liver cells plates/sinusoids and links centrilobular veins to portal tract |
|
|
Liver failure description |
-Most severe consequence of liver disease -Can be acute or chronic -Mortality: 80% |
|
|
When do we have symptoms of Liver failure? |
80-90% hepatic functional capacity loss |
|
|
Therapy for Liver failure |
Liver transplant |
|
|
Difference between acute and chronic liver failure |
Acute -> sudden and massive destruction
Chronic -> After decades of progressive liver injury |
|
|
Acute ("fulminant") liver failure definition |
Failure that occurs within 26 weeks of initial liver injury without pre-existing liver disease. Can be caused by massive hepatic necrosis (drugs -> acetaminophen; acute viral hepatitis A, B, E -> immune-mediated cell destruction; Toxins) |
|
|
Clinical features of Acute Liver Failure |
-Jaundice -Ascites -Fetor hepaticus (sweet fecal breath smell, "breath of the dead") -Hypoalbuminemia -Hypoglycemia -Palmar erythema -Spider angiomata -Testicular atrophy -Balding -Gynecomastia -Bleeding disorders -Hepatorenal syndrome -Hepatic encephalopathy |
|
|
Gross appearance of Acute Liver Failure |
Small, shrunken liver. Massive necrosis areas surrounded by regenerating hepatocytes. Scar formation and ductular reaction |
|
|
Chronic liver failure and cirrhosis |
Associated with cirrhosis in: -Chronic viral hepatitis -Non-alcoholic fatty liver disease -Alcoholic fatty liver disease -Autoimmune hepatic disease -Metabolic liver disease NB -> not all cirrhosis lead to liver failure (some can be compensated) and not all end-stage liver diseases show fully enstablished cirrhosis |
|
|
Definition of cirrhosis |
Diffuse transformation of the entire liver architecture with fibrosis and regeneration |
|
|
Morphology of cirrhosis |

-Diffuse involvement of liver -Regenerating hepatocellular nodules surrounded by collagen scars bands -Extremely variable size, pattern of scarring and vascular thrombotic obstruction -Is important to define the cause of cirrhosis -May partially regress with treatment of underlying cause |
|
|
Pathogenesis of cirrhosis |
1. Hepatocyte injury and necrosis 2. Necrosis -> hepatocyte regeneration, acrivation of stellate cells -> myofibroblast transition with collagen deposition, stem cells activation with ductular reaction 3. Formation of fibrous septa surrounding nodules of regenerating hepatocytes |
|
|
Features of Hep A |
-Epidemic -Fecal-oral transmission -Benign & self-limiting -Incubation period 2-6 weeks -Most common type worldwide -Rarely fatal -No carrier state -Vaccine available |
|
|
Features of Hep B |
-Infects hundreds of millions worldwide -Incubation time weeks to 6 months -More diffuse in Sub-Saharian Africa, China and India |
|
|
Scheme of Hep B development |
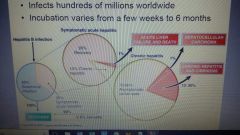
35% infections symptomatic -> of these, 10% become chronic -> of these, 1% dies and 9% progress -> of these, 70-90% become asymptomatic carriers and the rest develop chronic hepatitis and cirrhosis. 1% hepatocellular carcinoma |

