![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
129 Cards in this Set
- Front
- Back
|
spinal cord compression etiology
|
acute --> trauma, hematoma
subacute --> cancer (lymphoma, multiple myeloma, prostate, lung, breast, kidney, colon), epidural abscess chronic --> herniated disk |
|
|
spinal cord compression presentation
|
back pain (96%)
history of cancer, fever bowel or bladder dysfunction insidious onset of mild sensory disturbance lower limb weakness or rigidity |
|
|
spinal cord compression diagnosis
|
plain x-rays are 84-94% sensitive
gold standard is MRI if MRI is contraindicated --> CT myelogram |
|
|
spinal cord compression management
|
high-dose dexamethasone immediately upon suspicion
surgical decompression in trauma, herniated disk or epidural abscess radiotherapy in case on cancer |
|
|
syringomyelia etiology
|
central cavitation of spinal cord
communicating is associated with Arnold-Chiari non-communicating is associated with trauma or spinal cord tumors |
|
|
syringomyelia presentation
|
cervical and upper limb pain and temperature loss
may have lower motor neuron deficits in upper limbs and upper motor neuron deficits in lower limbs |
|
|
syringomyelia diagnosis and treatment
|
MRI is gold standard; surgery is unsatisfactory
|
|
|
subacute combined degeneration
|
B12 deficiency results in
corticospinal --> upper motor neuron signs, flaccid/spastic paralysis dorsal columns --> ataxia, vibration and propioception deficits, distal paresthesia diagnosis --> low serum B12 and high methylmalonic acid treatment --> B12 replacement |
|
|
anterior spinal artery occlusion
|
bilateral paralysis
pain, temperature and autonomic loss below lession conserved vibration and propioception |
|
|
Brown-Sequard syndrome
|
ipsilateral upper motor neuron signs below lesion
ipsilateral vibration and propioception loss below lesion contralateral pain/temerature loss 1-2 levels below lesion bilateral flaccid paralysis and anesthesia at level of lesion ipsilateral Horner syndrome if above T1 |
|
|
anterior cerebral artery irrigation
|
medial surface of frontal and parietal lobes
1 inch of supero-lateral surface of frontal and parietal lobes anterior limb of internal capsule caudate nucleus anterior 4/5 of corpus callosum |
|
|
anterior cerebral artery stroke presentation
|
contralateral lower limb paralysis
contralateral lower limb sensory loss urinary incontinece, behavioral disturbances |
|
|
middle cerebral artery irrigation
|
lateral surfaces of frontal, parietal and temporal lobes except superior inch
genu and posterior limb of internal capsule globus pallidus putamen |
|
|
middle cerebral artery stroke presentation
|
contralateral hemiplegia, contralateral anesthesia
contralateral homonymous hemianopia with eye deviation toward lesion contralateral central facial paralysis aphasia if left, apraxia and spacial disturbance if right |
|
|
posterior cerebral artery irrigation
|
cerebellum, brain stem, pons, occipital lobe
|
|
|
posterior brain circulation arteries
|
posterior cerebral artery
basilar artery cerebellar arteries paramedian branches vertebral artery |
|
|
posterior cerebral artery stroke
|
contralateral homonymous hemianopia
visual hallucinations agnosia associated Weber or Benedikt syndromes |
|
|
Weber syndrome
|
results from occlusion of penetrating branches of PCA
contralateral hemiplegia and CNIII palsy |
|
|
Benedikt syndrome
|
results from occlusion of penetrating branches of PCA
CNIII palsy with contralateral ataxia or athetosis |
|
|
paramedian branches of basilar artery stroke
|
quadriparesis with intact vertical eye movement
|
|
|
PICA stroke
|
Wallenberg / lateral medullary syndrome -->
lateral spinothalamic --> contralateral pain/temperature loss trigeminal nucleus --> ipsilateral facial sensory loss vesticular nucleus --> vertigo, nystagmus, nausea ambigus nucleus --> dysarthria, dysphagia, gag reflex inferior cerebellar peduncle --> ataxia descending sympathetics --> Horner syndrome |
|
|
Wallenberg syndrome
|
results from posterior cerebellar artery occlusion
lateral spinothalamic --> contralateral pain/temperature loss trigeminal nucleus --> ipsilateral facial sensory loss vesticular nucleus --> vertigo, nystagmus, nausea ambigus nucleus --> dysarthria, dysphagia, gag reflex inferior cerebellar peduncle --> ataxia descending sympathetics --> Horner syndrome |
|
|
cerebellar artery stroke
|
vertigo
vomitting nystagmus ipsilateral limb ataxia |
|
|
stroke diagnosis
|
initial test is noncontrast CT to diffeentiate between ischemic or hemorrhagic
CT will be normal in ischemic stroke in first 48 hours if ischemic --> check for embolic sources with echocardiogram, carotid duplex, 24-hour Holter and check for hypercoagulability if hemorrhagic --> do EKG for inverted T-waves |
|
|
tPA use in ischemic stroke
|
use if onset <3 hours in ischemic stroke
contraindications --> history of intracranial hemorrhage stroke or head trauma within 3 months hemorrhage within 3 weeks surgery within 2 weeks arterial puncture within 1 week lumbar puncture within 1 week BP > 185/110 anticoagulants thrombocytopenia PT > 15s |
|
|
stroke treatment
|
ischemic --> tPA if onset <3h; then aspirin +- dypiridamole OR clopidogrel +- endarterectomy
hemorrhagic --> nimodipine +- craniotomy or coiling or shunt |
|
|
seizures/epilepsy etiology
|
"VITAMINS" -->
Vascular (stroke, bleed, AVM) Infections (meningitis, encephalitis) Trauma Autoimmune Metabolic (hyponatremia, hypocalcemia, hypoglycemia, hypoxia, drug overdose) Idiopathic Neoplasm pSychiatric |
|
|
seizures/epilepsy general presentation
|
sudden onset of convulsions with or without aura
postictal symptoms --> disorientation, sleepiness, aching muscles associated signs --> incontinence, tongue biting, headache patients with syncope don’t have postictal symptoms or signs |
|
|
partial simple seizure
|
focal deficits without loss of consciousness
|
|
|
partial complex seizure
|
focal deficits with loss of consciousness
|
|
|
partial seizure with secondary generalization
|
begins as partial and converts to generalized
|
|
|
generalized tonic-clonic seizure
|
tonic contractions followed by clonic relaxation of muscles
first line --> valproic second line --> phenytoin, carbamazepine, lamotrigine |
|
|
absence seizures
|
sudden brief loss of consiousness without loss of postural tone
treat with ethusuximide or valproic |
|
|
atonic seizures
|
sudden loss of postural tone for 1-2 seconds
|
|
|
myoclonic seizures
|
sudden brief muscle contraction
|
|
|
status epilepticus
|
recurrent continuous seizures lasting at least 5-30min
|
|
|
epilepsy diagnosis
|
EEG is test of choice
abnormal EEG alone is not diagnostic (2-18% of population has abnormal EEG) first rule out reversible causes of seizures checking electrolytes, glucose, toxicology, arterial blood gases and structural lesions with CT or MRI |
|
|
acute management of seizures
|
1) secure ABCs
2) evaluate precipitating causes 3) medications in order: lorazepam/diazepam, phenytoin, phenobarbital, midazolam/propofol |
|
|
maintenance treatment of epilepsy
|
tonic-clonic --> valproic acid is first OR lamotrigine, carbamazepine, phenytoin
partial --> carbamazepine, phenytoin first OR lamotrigine, valproic second absence --> ethosuximide or valproic myoclonic and atonic --> valproic pregnant --> carbamazepine |
|
|
vertigo etiology
|
Meniere
labyrinthitis positional vertigo traumatic vertigo perilymphatic fistula cervical vertigo |
|
|
vertigo presentation
|
patient feels room is spinning without any real movement, nausea and vomitting
differentiate from presyncope which is described as lightheadedness and feeling of blackout vertigo is neurologic presyncope is cardiologic |
|
|
central vertigo Vs. peripheral vertigo
|
central --> gradual onset, absent tinnitus and hearing loss, diplopia, cortical blindness, dysarthria, weakness, vertical nystagmus
peripheral is contrary |
|
|
Meniere disease
|
endolymphatic pressure changes
peripheral episodic vertigo 1-8 hours common causes are syphillis and head trauma |
|
|
labyrinthitis
|
follows respiratory tract infection
peripheral vertigo lasts for several days |
|
|
benign paroxysmal positional vertigo
|
peripheral vertigo exacerbated by head movements lasts 10-60 seconds
|
|
|
central vertigo
|
due to cerebellar or brain tumor, bleed, bleed, drug toxicity or multiple sclerosis
|
|
|
vertigo treatment
|
peripheral --> symptomatic with meclizine or diazepam
Meniere --> low-salt diet and diuretics benign paroxysmal --> head maneuvers |
|
|
headache etiology
|
primary --> migraine (15% of population), cluster, tension
secondary --> hemorrhage, brain tumor, meningitis, temporal arteritis, glaucoma |
|
|
meningitis headache
|
accompanied with fever and nuchal rigidity
|
|
|
intracranial hemorrhage headache
|
associated with nuchal rigidity, sudden onset, severe and without fever
|
|
|
brain tumor headache
|
deep, dull, aching pain disturbs sleep
|
|
|
posterior brain fossa tumor headache
|
history of vomitting weeks before, or induced by coughing, lifting or bending
|
|
|
temporal arteritis headache
|
unilateral pounding, dull headache associated with visual disturbances, jaw claudication, weight loss, arthritis, increased ESR
|
|
|
migraine presentation
|
pain described as pulsatile, throbbing, unilateral, aggravated by movement
nausea and vomitting photophobia, phonophobia may have aura or not aura --> scintillating scotoma, flashes of light, motor, sensory or visual symptoms |
|
|
tension headahces presentation
|
tight, band-like, bilateral headaches
builds slowly, may persist for days and is not exacerbated by movement may have tightness of posterior neck muscles |
|
|
cluster headache presentation
|
excrutiating, unilateral, pulsatile, periorbital headache that begins without warning and peaks in intensity within 5 minutes; lasts 30 minutes to 3 hours, 1-3 times/day for a 4-8 week period; associated with rhinorrhea, reddening of the eye, lacrimation and nasal stuffness
|
|
|
headache diagnosis
|
clinical history and tests to exclude secondary causes
if severe, sudden onset of first time headache --> head CT |
|
|
acute management of migraines
|
mild --> NSAIDs
severe, first line --> triptans (contraindicated in heart disease) severe, 2nd line --> ergotamine + caffeine |
|
|
prophylaxis of migraines
|
first line --> propranolol, timolol, valproic acid, topiramate
second line --> verapamil, tricyclics, SSRIs |
|
|
treatment of tension headaches
|
relaxation + acetaminophen/NSAIDs +- muscle relaxant
|
|
|
treatment of cluster headaches
|
100% O2, prednisone and lithium
may use sumatriptan, ergotamine, verapamil |
|
|
pseudotumor cerebri etiology
|
8-10x more common in women
associated with obesity, COPD, Addison, oral contraceptives, tetracyclines, vit A toxicity |
|
|
pseudotumor cerebri presentation
|
headache, diplopia, abducens palsy, papilledema
CT/MRI are normal CSF is normal beyond increase in pressure |
|
|
pseudotumor cerebri treatment
|
weight loss
removing offending agent diuretics (acetazolamide, furosemide) prednisone may be useful as well as repeated lumbar punctures |
|
|
trigeminal neuralgia presentation
|
sudden, severe, sharp pain starts near mouth and progresses towards ear, eye or nostril and lasts few seconds; can be a manifestation of multiple sclerosis or posterior fossa tumors
|
|
|
trigeminal neuralgia treatment
|
carbamazepine
may also try phenytoin, baclofen or gabapentin |
|
|
Guillain-Barre syndrome presentation
|
progressive paralysis
arreflexia pain or tingling autonomic instability history of recent infection (campylobacter, herpes, CMV, EBV) lack of constitutional symptoms |
|
|
Guillain-Barre syndrome diagnosis
|
history + lumbar puncture looking for ↑proteins and normal cell count
(best initial test, 48 hours after onset) electromyography is most specific |
|
|
Guillain-Barre syndrome treatment
|
IV immunoglobulin or plasmapheresis are equally effective
glucocorticoids are not effective early respiratory support to prevent death |
|
|
What are the basic molecules used in serological classification of streptococcie?
(serological classification = using serum antibodies to identify similar and different types of bacteria) pg 281 |
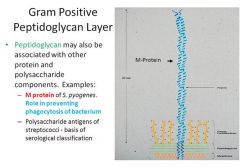
presence of POLYSACCHARIDE antigens associated with the gram POSITIVE peptidoglycan layer
|
|
|
myasthenia gravis diagnosis
|
best initial test --> acetylcholine receptor antibodies
most specific test --> electromyography (decrease in contraction on repetitive stimulation) edrophonium test is sensitive but not specific should do x-ray or CT to exclude thymoma |
|
|
Eaton-Lambert or botulism difference with myasthenia
|
Eaton-Lambert and botulism improve weakness with repetitive stimulation
myasthenia gets worse |
|
|
myasthenia gravis treatment
|
symptomatic relief --> pyridostigmine, neostigmine + plasmapheresis
thymectomy indicated in postbubertal and <60 with generalized myasthenia if thymectomy fails then steroids +- azathioprine mycophenolate is newer immunosuppressive avoid aminoglycosides |
|
|
amyotrophic lateral sclerosis presentation
|
upper motor neuron and lower motor neuron signs concomitantly is unique presentation
fasciculations, tongue atrophy, renervation after denervation on biopsy also nerve palsies (dysphagia, difficulty chewing, decreased gag reflex, etc) respiratory involvement with intact cognitive, sensory and autonomic function |
|
|
amyotrophic lateral sclerosis diagnosis
|
physical exam + electromyogram
CSF and MRI are normal |
|
|
amyotrophic lateral sclerosis management
|
riluzole slows progression
|
|
|
multiple sclerosis presentation
|
young female with relapsing remitting episodes of
weakness numbness tingling urinary urgency or retention blurry/double vision episodes resolve spontaneously |
|
|
multiple sclerosis diagnosis
|
clinical diagnosis + MRI of brain and spine
evoked potentials are rarely used CSF shows mild pleocytosis and mildly elevated proteins CSF for oligoclonal IgG banding is recommended when clinical suspicion remains after unconfirmatory MRI |
|
|
multiple sclerosis treatment
|
remitting relapsing disease --> interferon-B1a, interferon-B1b, glatiramer
secondary progressive disease --> interferon-B1b and mitoxanthrone (2nd-line) primary progressive disease --> no effective therapy acute exacerbations --> IV glucocorticoids spasticity --> baclofen trigeminal neuralgia --> carbamazepine bladder hyperactivity --> oxybutynin urinary retention --> bethanecol |
|
|
reversible causes of dementia
|
hypothyroidism
B12 deficiency hepatic encephalopathy CNS vasculitis syphilis brian abscess brain tumor anticholinergics apnea trauma subdural hematoma normal pressure hydrocephalus depression |
|
|
irreversible causes of dementia
|
Alzheimer (most common)
multifocal leukoencephalopathy Lewy bodies frontotemporal degeneration (Pick) vascular dementia Creutzfeld-Jakob |
|
|
dementia definition
|
memory loss along with impairment of other cognitive functions that interferes with social functioning
|
|
|
Alzheimer
|
memory loss + aphasia or apraxia or agnosia; inability to make plans and execute them
|
|
|
Pick disease
|
personality changes precede memory loss; patient lacks insight into condition
|
|
|
dementia with Lewy bodies
|
fluctuating cognitive impairment
|
|
|
Creutzfeld-Jakob
|
short, aggressive progression of dementia, myoclonus, ataxia and 14-3-3 protein in CSF
|
|
|
multi-infarct dementia
|
stepwise progression associated with discrete cerebrovascular events
|
|
|
Binswanger
|
slowly progressive vascular dementia that affects subcortical white matter
|
|
|
normal pressure hydrocephalus dementia
|
associated with gait abnormalities early in the course and urinary incontinence
|
|
|
dementia diagnosis
|
assesment of cognitive impairment with mini mental exam
CBC, electrolytes, calcium, creatinine, liver function tests, glucose, TSH, B12, RPR, HIV brain imaging in cases of focal deficits, seizures, gait abnormalities |
|
|
Alzheimer treatment
|
anticholinestrase inhibitors donepezil, rivastigmine, galantamine improve cognitive function
memantine is disease modifying used in advanced disease alone or in combo |
|
|
Huntington
|
chorea + behavioral disturbances (irritability, anger, paranoia, depression)
diagnosed with genetic testing for CAG triplet repeat expansion cerebral atrophy (cortex, basal ganglia) can be seen in brain imaging |
|
|
Parkinson etiology
|
structural lesions in basal ganglia
survivors of encephalitis neuroleptics (haloperidol, chlorpromazine) metoclopramide methyldopa reserpine |
|
|
Parkinson presentation
|
Bradykinesia
cogwheel Rigidity postural Instability resting Tremor "BRITish" |
|
|
Parkinson+ syndromes
|
parkinsonism + vertical gaze palsy --> supranuclear palsy
parkinsonism + ataxia --> olivopontocerebellar atrophy parkinsonism + orthostatic hypotension --> Shy-Drager syndrome |
|
|
diseases that mimic parkinsonism
|
severe depression
essential tremor normal pressure hydrocephalus Huntington |
|
|
Parkinson diagnosis
|
clinical diagnosis
|
|
|
Parkinson treatment with intact functional status
|
anticholinergics --> amantadine are first-line, then the rest
|
|
|
Parkinson treatment with compromised functional status
|
initial therapy is carbidopa/levodopa
if dyskinesia, akathisia or on-off --> add pramipexole, selegiline or COMT inhibitor (tolcapone) |
|
|
essential tremor
|
improves with alcohol; treat with propranolol
|
|
|
hereditary spherocytosis diagnosis and treatment
|
anemia, normal MCV, ↑LDH, ↑reticulocytes, ↑indirect bilirubin
spherocytes and negative Coombs test positive osmotic fragility test treat with folate or splenectomy |
|
|
paroxysmal nocturnal hemoglobinuria etiology
|
red cell membrane defect in phosphatidyl inositol glycan A leads to increased complement lysis and intravascular hemolysis
|
|
|
paroxysmal nocturnal hemoglobinuria presentation
|
symptoms of anemia acording to severity
hemoglobinuria (specially in morning urine) thrombosis (specially hepatic vein, Budd-Chiari) |
|
|
paroxysmal nocturnal hemoglobinuria diagnosis and treatment
|
↓DAF, hematuria
normal MCV, ↑LDH, ↑reticulocytes, ↑indirect bilirubin, ↓haptoglobin specific tests are sugar-water test and acidified hemolysis test treat with folate, corticosteroids and anticoagulation for thrombosis |
|
|
G6PDH deficiency
|
enzyme deficiency leads to ↓NADPH, ↓gluthathione peroxidase activity and ↑unmetabolized H2O2 which precipitates Hb (Heinz bodies)
precitpitated by infections, sulfa drugs, primiquine, quinidine, dapsone, nitrofurantoin presentation --> sudden-onset anemia symptoms, jaundice, dark urine normal MCV, ↑indirect bilirubin, ↑LDH, ↑reticulocytes, ↓haptoglobin, hemoglobinuria, Heinz bodies, bite cells definitive test is ↓G6PDH treat with hydrration |
|
|
aplastic anemia etiology
|
most common is idiopathic; radiation, benzene, NSAIDs, chloranphenicol, alcohol, alkylating agents; infections: hepatitis, HIV, CMV, EBV, ParvoB19;
|
|
|
aplastic anemia presentation
|
bleeding from thrombocytopenia
fatigue, anemia and may have infections from neutropenia may have history of using precipitating drugs |
|
|
aplastic anemia diagnosis and treatment
|
screening --> pancytopenia
confirm --> bone marrow biopsy showing absence of marrow cells, fat and no signs of cancer, infection or fibrosis in marrow treat --> bone marrow transplant; if not, antithymocyte globulin, cyclosporine and prednisone |
|
|
acute leukemia etiology
|
most have no apparent cause; associated with radiation, benzene, melphalan, etoposide, retroviruses, Down and Klinefelter, myelodysplasia and sideroblastic anemia
|
|
|
acute leukemia presentation
|
fatigue, anemia and bleeding from thrombocytopenia +- leukopenia or leukocytosis
ALL --> in children, hepatosplenomegaly, lymphadenopathy, bone pain AML --> DIC (promyelocytic M3), CNS meningitis-like (monocytic M4, M5) |
|
|
acute leukemia diagnosis
|
pancytopenia although leukocytes can be up, down or normal
leukemic blasts in peripheral blood bone marrow biopsy showing >20% blasts confirms diagnosis to differentiate --> AML --> Auer rods (specially M3), myeloperoxidase and esterase ALL --> CALLA and TdT specific types of leukemia are diagnosed with monoclonal antibodies |
|
|
acute leukemia treatment
|
AML --> AraC with danourubicin or idarubicin
ALL --> daunorubicin, vincristine and prednisone add all-trans-retinoic acid in promyelocytic leukemia remission is removal of 99.9% of leukemic cells and elimination of blasts in peripheral blood |
|
|
differential diagnosis for pancytopenia
|
marrow --> aplastic anemia, metastatic cancer to marrow, myelofibrosis
infectious --> parvirus, retrovirus auto-immune --> B12 deficiency, SLE, hypersplenism drugs --> chloramphenicol acute leukemia is only one that shows blasts in peripheral blood |
|
|
chronic myelogenous leukemia etiology
|
clonal disorder of myelocytes associated in 95%with translocation t(9,22) (Philadelphia chromosome) which produces an enzyme with tyrosine kinase activity
|
|
|
chronic myelogenous leukemia presentation
|
leukocytosis and sometimes thrombocytosis lead to
fatigue, night sweats, low-grade fever abdominal pain, splenomegaly, bone pain rare --> lymphadenopathy, infection or bleeding leukostasis has dyspnea, blurry vision, priapism, thrombosis, stroke |
|
|
chronic myelogenous leukemia diagnosis
|
leukocytosis (mostly neutrophils)
↓LAP (difference with leukemoid reaction) absent or very low blast count if leukocytosis and ↓LAP --> check for Philadelphia chromosome |
|
|
chronic myelogenous leukemia treatment
|
imatinib is an inhibitor of the tyrosine kinase produced by disease
90% hematologic response and 60-70% loose Philadephia chromosome if imatinib doesn’t work --> bone marrow transplant |
|
|
chronic lymphocytic leukemia presentation
|
older patients can be asymptomatic
0 --> lymphocytosis alone 1 --> lymphadenopathy 2 --> splenomegaly 3 --> anemia 4 --> thrombocytopenia infection and bleeding are unusual survival of stage 0-1 is 10-12 years survival of 3-4 is 1-2 years |
|
|
chronic lymphocytic leukemia diagnosis
|
suspected in older patient with leukocytosis (80-98% lymphocytes)
bone marrow biopsy confirms leukemic lymphocytes smudge cells on peripheral smear |
|
|
chronic lymphocytic leukemia treatment
|
stages 0-1, no specific treatment
symptomatic patients are given fludarabine (DOC) or chlorambucil prednisone for autoimmune hemolysis and thrombocytopenia pentostatin for relapses |
|
|
multiple myeloma presentation
|
bone pain (specially back, ribs), lytic lessions, osteoporoosis, pathologic fractures
hypercalcemia (polyuria, polydipsia, altered mental status) renal failure (Bence Jones light chains) infection with encapsulated bugs anemia |
|
|
multiple myeloma diagnosis
|
normo normo anemia, hypercalcemia, ↑BUN, ↑creatinine
lytic bone lessions on x-rays Bence Jones protein ↑serum microglobulin B2 (75%) electrophoresis with monoclonal IgG spikes cofirmation --> bone marrow biopsy showing >10%plasma cells confirms |
|
|
multiple myeloma treatment
|
younger patients --> transplant (pre-treat with thalidomide, dexamethasone)
older patients --> melphalon, prednisone, thalidomide treat hypercalcemia with loop diuretics |
|
|
monoclonal gammopathy of uncertain origin
|
overproduction of clonal immunoglobulin by plasma cells without systemic manifestations
patient is asymptomatic clue to diagnosis is elevated serum protein monoclonal Ig spike on protein electrophoresis no bone lessions, no anemia, no renal failure, no hypercalcemia no treatment necessary |
|
|
Hodgkin disease presentation
|
nontender lynmphadenopathy
cervical, supraclavicular or axillary nodes are most common B symptoms are drenching night sweats, 10% weight loss, fever |
|
|
Hodgkin disease diagnosis
|
first step --> excisional lymph node biopsy showing Reed-Sternberg cells
second step --> determine staging with CT if CT is unrevealing and radiotherapy is contemplated then do laparotomy also anemia, leukocytosis, eosinophillia, ↑LDH, ↑ESR (adverse prognosis) may be seen |
|
|
Hodgkin disease adverse prognostic factors
|
large mediastinal lymphadenopathy
age older than 40 B symptoms ↑ESR |
|
|
Hodgkin disease treatment
|
stage I and II --> radiotherapy
B symptoms or stage III or IV --> ABVD chemo (adriamycin, bleomycin, vinblastine, dacarbazine) has less side effects than MOPP chemo (meclorethamine, oncovin/vincristine, prednisone, procarbazine) potential side effects --> permanent sterility, cancer, leukemia, aplastic anemia, peripheral neuropathy |
|
|
non-Hodgkin lymphoma etiology
|
HIV, hepatitis C, EPV, HTLV-1, H. pylori
HIV and EPV are associated with Burkitt and high-grade high-stage lymphomas |

