![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
116 Cards in this Set
- Front
- Back
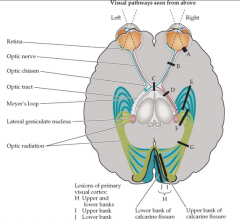
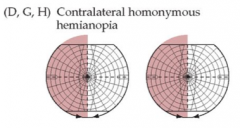
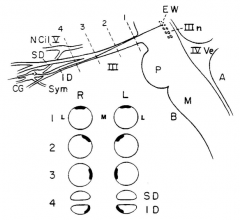
Lesion at D
|
|
|
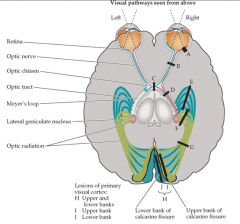
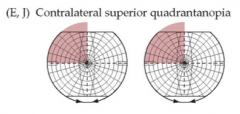
Lesion at E
|
|
|
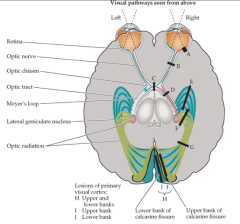
Lesion at J
|
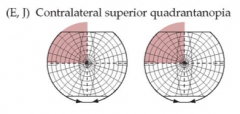
Contralateral superior quandrantanopia
|
|
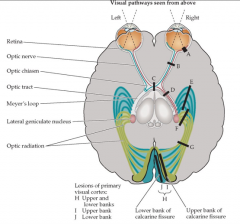
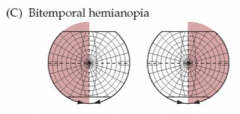
Lesion at C
|
|
|
|
Miosis
|
Constriction of the pupil
|
|
|
Autonomic innervation of the iris
|
Balance between sympathetic tone (dilation, radial muscles) and parasympathetic tone (constriction, sphincter muscles).
|
|
|
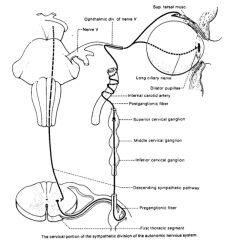
Sympathetic innervation of the iris
|
|
|
|
Parasympathetic innervation of the iris
|
Via the oculomotor nerve to the ciliary ganglion to synapse with postganglionic neuron.
|
|
|
Muller's muscle
|
Superior and inferior tarsal muscles.
Sympathetic innervation --> brings upper eyelid up and lower eyelid down. Horner's syndrone --> height of palpebral fissure on the affected side is less high than the affected side. |
|
|
A balloon aneurysm of the posterior communicating artery?
|
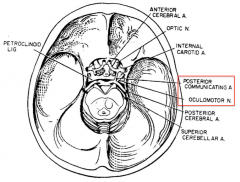
Compression of the oculomotor nerve. Pupil will be dilated because the parasympathetic tone is affected. Parasympathetic fibers ride superficially on the oculomotor nerve bundle; therefore compression causes PNS Sx first.
|
|
|
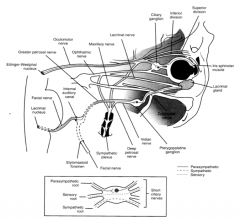
Where do PNS fibers travel from the midbrain to the eye?
|
Via the oculomotor nerve. Important, they ride on the surface of CN III and are vulnerable to compression forces (e.g. aneurysm).
|
|
|
Direct and indirect light reflex pathways
|
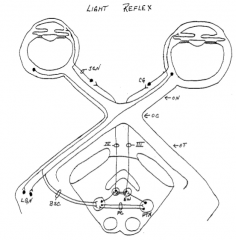
1st afferent nerve (ganglion cell --> optic nerve, chiasm, tract). 2nd afferent nerve is in the pretectal nucleus. The connection between the two PTN's is the posterior commissure. Efferent nerve is CN III.
|
|
|
Signs of accommodation reflex
|

Pupils constrict, eyes adduct, and lens becomes rounder (not seen).
|
|
|
Accommodation, macrognathia, SIADH, psychosis
|

|
|
|
Accommodation reflex
|
Results: pupillary constriction (parasympathetic to sphincter muscles), lens get rounder (ciliary muscle contraction), eye adduction (medial rectus muscle).
Superior colliculus fibers talk to oculomotor complex (both the EW nucleus and alpha motor neurons). Medial rectus muscle must contract and lateral rectus muscle must relax (abducens inhibition). |
|
|
Congruous vs incongruous lesions
|
Congruous lesions are usually post-geniculate, involving the optic radiations. Incongruous lesions are usually pre-geniculate.
|
|
|
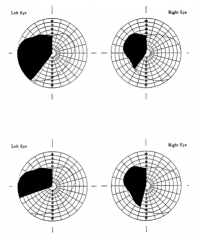
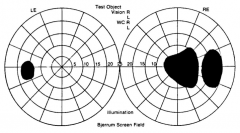
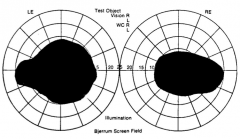
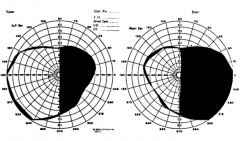
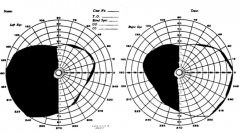
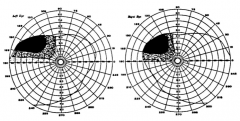
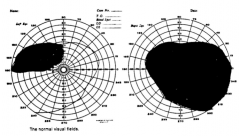
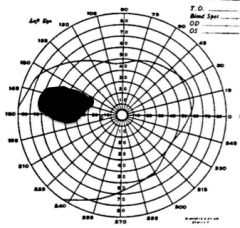
Right central scotoma (almost 10 degrees). This includes the foveal and maculal visual fields. Could be due to a retinal problem or the central fibers of the optic nerve.
|
|
|
Bilateral cecrocentral scotoma.
Continuity between the loss of macular vision and the blind spot. |
|
|
Right homonymous hemianopsia with macular involvement --> The lesion has to "whack more than 50% of the fibers behind the eyeball". Congruous.
Also, the right visual field defect is larger than the left. This is because 53% cross from the right eye and 47% stay ipsilateral from the left. |
|
|
Left homonymous hemianopsia with macular sparing. This patient may not even know they have a visual field defect because the "world they care about" is seen through the intact macular visual field.
|
|
|
Meyer's loop lesion or "pie in the sky" deficit. Left superior homonymous quadrantanopisa. Fibers that emerge from the lateral part of the lateral geniculate.
|
|
|
Right anopsia with a left superior temporal quadrantanopsia.
R sided lesion, prechiasmatic, affecting Wilbrand's knee area, possibly due to pituitary tumor |
|
|
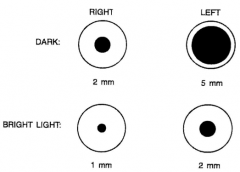
Less reactive pupil is probably the bad one.
R side impairment in a dark environment more so than light environment; therefore, missing sympathetic tone in the dark. |
|
|
Less reactive pupil is probably the bad one.
L side impairment in bright environment more so than the dark environment; therefore missing parasympathetic tone in the dark. |
|
|
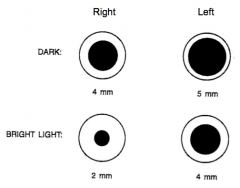
R side CN III injury --> anisocoria, strabismus, ptosis.
The affected eyes points inferior and laterally. |
|

|
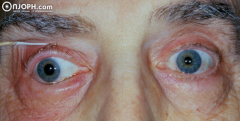
Anisocoria; R side myosis, ptosis.
Horner's syndrome --> impaired sympathetic tone. If the patient looks up and the ptosis resolves, then it's not a CN III injury and it's Horner's. This is because the CN III supplies the levator palpebrae. |
|
|
Visual agnosia
|
Impairment in recognition of visually presented objects. Apperceptive - cannot form a whole percept of visual information, although basic visual functions are normal.
Associative - inability to identify objects even with apparent perception and knowledge of them. |
|
|
Normal aging of lens
|
Sclerosis (hardening) and decreased elasticity of lens causes presbyopia (no near vision). Can't accommodate well enough to read fine print up close.
|
|

A unilateral retinal lesion at this location will result in what visual field deficit?
|
Left unilateral scotoma, slightly in upper temporal quadrant.
|
|
|
Fusion
|
The ability to keep a single image on both fovea
|
|
|
Lateral and medial walls of the orbit
|
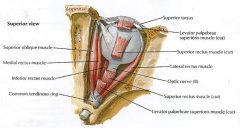
Medial wall is straight and points directly out. Lateral wall is concave and points temporally.
|
|
|
XYZ axes of eye and its movements
|
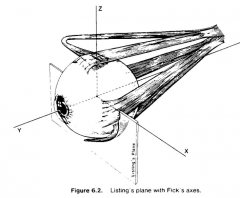
Ductions are monocular rotations.
X axis: pitch; supraduction, subduction, or elevation and depression. Y axis: roll; intorsion (medial) and extorsion (lateral), or incycloduction and exocycloduction. Z axis: yaw; adduction, abduction |
|
|
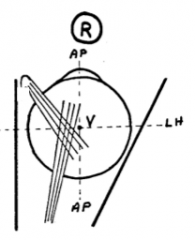
Superior rectus muscle
|
O: common tendinous ring
I: anterior to Listing's plane, medial to the AP axis Movements: supraduction (X axis), adduction (Z axis), intorsion (Y axis) 3 actions because it's pull is NOT parallel to any axis Innervated by LMN's exclusively from neurons in a contralateral nucleus, unlike other CN III ocular nerves. |
|
|
Inferior rectus muscle
|
O: common tendinous ring
I: anterior to Listing's plane Movements: subduction (X axis), adduction (Z axis), extorsion (Y axis) 3 actions because it's pull is NOT parallel to any axis |
|
|
Superior oblique muscle
|
O: body of the sphenoid (but forces start at the trochlea which is anteromedial)
I: behind Listing's plane, medial to AP axis Movements: subduction (X axis), abduction (Z axis), intorsion (Y axis) 51 degree angle; therefore it's a stronger intorter than subducter. |
|
|
The trochlear nerve arises from a nucleus on the (ipsilateral/contralateral) side?
The abudcens nerve arises from a nucleus on the (ipsilateral/contralateral) side? |
Contralateral
Ipsilateral |
|
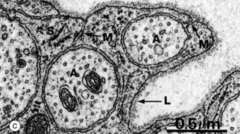
What is shown here?
|
Unmyelinated fibers enclosed by Schwann cells in the PNS. Note the mesaxons, labeled M.
|
|
|
Embryological origins of CNS cells
|
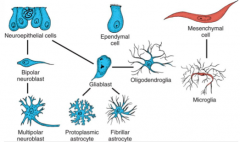
Neuroectoderm: Brain (neurohypophysis, CNS neurons, oligodendrocytes, astrocytes, ependymal cells, pineal gland), retina, spinal cord.
Mesenchymal cell: microglia. |
|
|
Version
|
To maintain fusion/foveation when distance between eyes and viewed object does not change. As the object comes closer, the visual axes of each eye approach each other and the angle gets bigger (vergence).
From infinity to ~20ft, the angle between the visual axes don't change appreciably. |
|
|
Vergence
|
To maintain fusion/foveation when distance between eyes and viewed object increases or decreases.
Convergence = objects within ~20ft Divergence = objects move away (visual axes get more parallel) |
|
|
Sherrington's Law
|
Law of reciprocal innervation: antagonist muscles operating on the same eye are reciprocally excited or inhibited.
i.e. This law describes what has to happen to cause a single eye to do something. E.g. If I want to contract my lateral rectus (EPSP), I need to relax my medial rectus (IPSP). |
|
|
Hering's Law
|
Law of yoked muscles: muscles that produce conjugate eye movements are similarly excited or inhibited.
The onset of movement must be the same, the rate of movement must be the same, the rotation must be the same, and the termination of movement must be the same. E.g. To look left: left eye has to contract lateral rectus while right eye has to contract medial rectus. |
|
|
MLF and gaze centers
|
Axons that connect ocular motor nuclei together:
1) oculomotor nucleus 2) trochlear nucleus 3) abducens nucleus Gaze centers contribute axons to MLF: Paramedian pontine reticular formation (PPRF) - horizontal gaze 1) paraabducens nucleus Mesencephalic gaze center - vertical gaze 2) 3 subnuclei: interstitial nucleus of Cajal, nucleus of Dar, riMLF MLF is located between rostral midbrain to caudal medulla. Highly myelinated and completely developed prenatally. |
|
|
Stimulation of PPRF
|
Ipsilateral horizontal gaze shift.
Diagram shows the ipsilateral abducens nucleus being stimulated and the contralateral medial rectus alpha motor neuron (III) also being stimulated. i.e. Hering's Law. At the same time the PPRF nucleus on one side is the stimulated, the PPRF on the contralateral side is inhibited, which leads to inhibition of the antagonist muscles in each eye. i.e. Sherrington's Law. A lesion in a PPRF nucleus, the eyes will turn to the contralateral side. |
|
|
Tropia
|
Malalignment of visual axes when there is free vision due to unopposed actions of unaffected muscles.
In tropia --> Light can hit the retina of both eyes. Tropias are manifest, phorias are latent. |
|

Patient is looking straight ahead.
|
Strabismus --> esotropia. Right abducens nerve lesion.
|
|
|
If I damage a trochlear nucleus, are the deficits ipsilateral or contralateral?
|
Contralateral
|
|
|
Strabismus --> Hypertropia.
Damage to right trochlear nerve or left trochlear nucleus. The eye is extorted because the IO is unopposed. The eye is supraducted because the SO is gone and the IO is unopposed. Pt compensates by head tilting to contralateral side and tilting of the head forwards/down. |
|
|
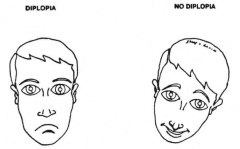
Uncrossed diplopia
|
Covering the right eye will make the out-of-focus image disappear.
|
|
|
Corneal light reflection test
|
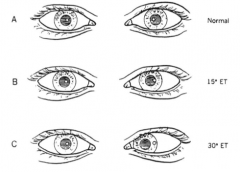
In normal eyes, the reflection should be located low and medial in each pupil. As an eye becomes esotropic, the reflection moves laterally.
|
|
|
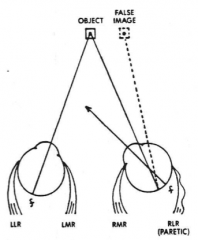
Primary and secondary deviation
|
The angle subtended when the good eye is viewing (primary) and the angle subtended when the bad eye is viewing (secondary). E.g. By making the bad eye focus on an object, a lot of 6th nerve impulses must be sent to move the eye a little--at the same time the good eye moves medially a lot (increasing the subtended angle).
|
|
|
Single cover test
|

Evaluation of tropia. Cover the fixating eye, observe the response of the non-fixating eye.
|
|
|
Cover-uncover test
|

Evaluation of tropia. Cover an eye, uncover the eye and observe the response in that eye.
When you uncover the good eye, you will see a big response. |
|
|
Orthophoria
|

No phoria when vision is blocked in an eye.
|
|
|
When the frontal eye fields are excited, which way do they eyes shift gaze?
|
Contralaterally.
By "thinking" I want to look left, the frontal area 8 sends an excitatory signal to the contralateral PPRF and inhibitory signal to ipsilateral PPRF. |
|
|
Bony vs membranous labyrinths
|
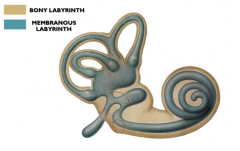
Bony labyrinth is a set of channels and spaces in BONE.
Membranous labyrinth is "suspended" in it, and contains sensory structures. |
|
|
|
|
|
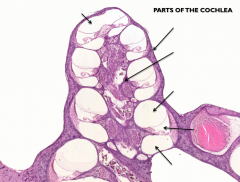
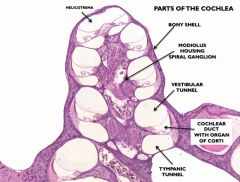
Vestibular and tympanic ducts of cochlea
|
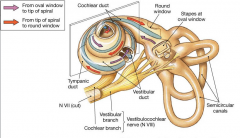
|
|
|
Where in the cochlear duct are high frequency sounds transmitted?
|
Hair cells at the base. Low frequency sounds are transmitted at the apex.
Small guitar strings have high notes --> basilar membrane is smallest at the base. |
|
|
Tensor tympani muscle
|
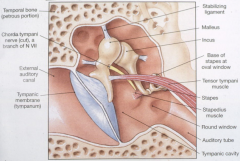
Pulls the malleus towards the inner ear and puts tension on the tympanic membrane. This decreases the movement of the TM and decreases transmission of sound to the oval window.
|
|
|
Malleus and stapes are derived from which pharyngeal arch?
|
1st arch. Therefore, the tensor tympani muscle is innervated by the CN V nerve.
|
|
|
Helicotrema
|
An opening in the basilar membrane at the apex of the cochlear duct that allows a compression wave from the scala vestibuli to be transmitted to the scala tympani.
|
|
|
Movement of the smallest stereocilia towards the longest stereocilia...
|
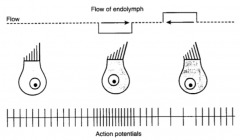
Depolarizes the hair cells.
|
|
|
Spiral ganglion cells are what type of neuron?
|
Special sensory, bipolar cells.
|
|
|
Tonotopic organization of the dorsal and ventral cochlear nuclei
|
Dorsal part of each nucleus preferentially respond to high frequency tones.
|
|
|
Decussating fibers of the dorsal and ventral cochlear nuclei
|
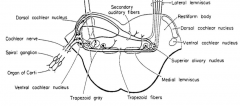
|
|
|
The tissue innervated by the afferent limb of CN V is derived from which germ layers?
|
Ectoderm and somatic mesoderm
|
|
|
The long ciliary nerves of V1 innervate what?
|
1) Sensory from cornea (corneal reflex)
2) Postganglionic sympathetic axons to pupillary dilator |
|
|
What nerve supplies the cheek, and the upper teeth and gums?
|
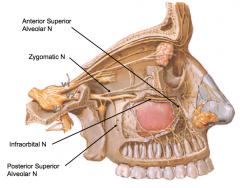
Infraorbital n. of V2
|
|
|
The lingual nerve carries what information?
|
GSA from the tongue (via CN V) and SVA from the tongue (CN VII).
GSA is pain, like biting your tongue. SVA is taste. |
|
|
The skin of the angle of the mandible is innervated by what?
|
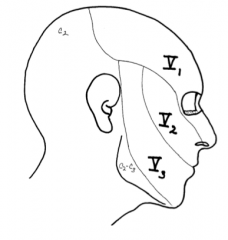
C2-C3, not CN V! Find out if patients are lying!
|
|
|
Which cranial nerves carry preganglionic autonomic axons?
|
CN III, V II, IX, X
|
|
|
What's the thalamic target of axons from the spinal trigeminal nucleus?
|
VPM via the ventral trigeminothalamic tract
|
|
|
The dorsal trigeminothalamic tract contains axons from where?
|
Axons from the principal trigeminal nucleus (light touch) that did not decussate but ascending ipsilaterally.
|
|
|
Masseter reflex
|
Afferent and efferent via CN V (a segmental reflex).
Normally suppressed by frontal lobe, but is released from suppression in frontal lobe lesions. A positive masseter reflex is a sign of frontal lobe path. |
|
|
Corneal reflex
|
Approach the patient's eye from the side with a cotton tip and touch the cornea. Normal response is bilateral blinking.
Afferent limb: long ciliary --> CN V Efferent limb: CN VII on ipsilateral and contralateral sides *Multisegmental. When the reflex is impaired, you need to test on both sides to figure out where the lesion is. *Not normally performed on conscious pts, but comatose pts. |
|
|
Lacrimation reflex
|
Irritation of the cornea leads to tearing
Afferent: long ciliary nerve --> CN V Efferent: stimulation of PS via CN VII to the lacrimal gland Postganglionic neurons are in pterygopalantine ganglia (hanging off the maxillary nerve V2) |
|
|
Branches of CN VII
|
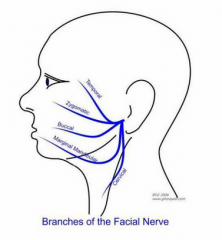
To Zanzibar By Motor Car:
Temporal Zygomatic Buccal Marginal Mandibular Cervical |
|
|
Bell's palsy vs. stroke
|
Both can present as unilateral facial paresis. With UMN damage (stroke), the upper face is OKAY (because the upper face receives UMN input bilaterally). With LMN damage (CN VIIth lesion), the entire side of the face is paretic.
|
|
|
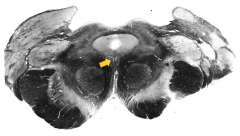
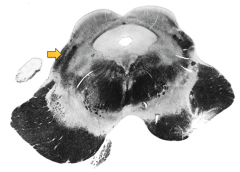
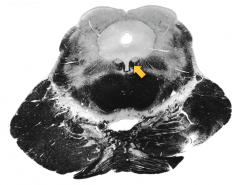
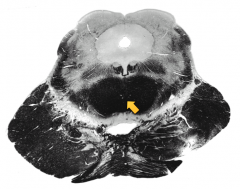
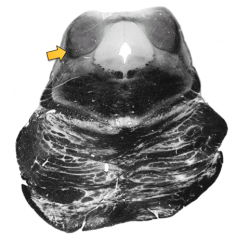
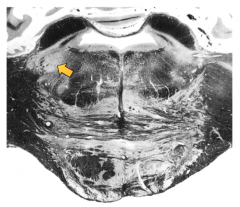
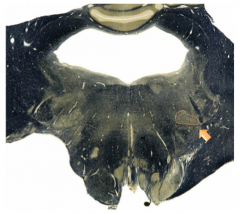
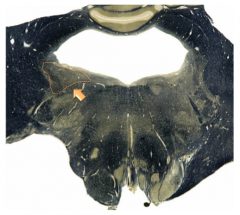
Rostral midbrain. Oculomotor complex (darker) and Edinger-Westphal nucleus (lighter).
|
|
|
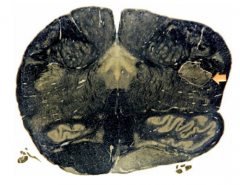
Rostral midbrain. Brachium of the inferior colliculus.
|
|
|
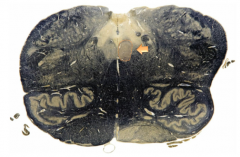
Intercollicular level of the midbrain. MLF with trochlear nucleus nearby.
|
|
|
Decussation of the superior cerebellar peduncle.
|
|
|
Lateral lemniscus entering the inferior colliculus.
|
|
|
CN V motor nucleus
|
|
|
2 major divisions of the facial nerve
|
Facial nerve proper and nervus intermedius
|
|
|
Bell's phenomenon
|

Upward and outward movement of the eye when an attempt is made to close it. Becomes noticeable when the orbicularis oculi muscle can't close the eye, e.g. Bell's palsy.
|
|
|
Titubation
|
Tremor of the axial body or head
|
|
|
What actions do the efferents of the vestibulocerebellum, spinocerebellum, and pontocerebellum relate to?
|
Vestibulocerebellum relates to eye movements and axial and proximal limb musculature.
Spinocerebellum relates to the control of axial muscles and limb musculature. Pontocerebellum relates to the planning, timing, and control of precise upper extremity movements. |
|
|
Parkinsonian gait
|
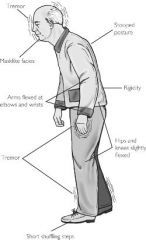
Stooped posture, stiff leg movements, arms flexed with little arm swing. Pts take short, shuffling steps that accelerate the further they walk. More than 2 steps to turn around.
|
|
|
Hemiparetic spastic gait
|
Spasticity causes the extremity to be stiff. In a hemiparetic gait the spastic stiff leg is circumducted (the leg swings in a semicircle from a medial to lateral direction) as the patient walks, and the toe hits the ground before the heel does. Often the arm on the paretic side does not swing well and is flexed at the elbow.
|
|
|
Slapping or steppage gait
|
Occurs when the pt has either a footdrop from weakness of the foot dorsiflexors or poor position sense in the feet. With a footdrop the pt flexes the hip so that the foot will clear the floor. Pts with poor position sense have a wide-based gait, their feet slap the floor, and they require visual assistance to walk. Pts with a slapping gait from poor position sense often have great difficulty ambulating in the dark.
|
|
|
Athetosis
|

Slow, involuntary, writhing movements of especially the hands
|
|
|
Blepharospasm
|
Abnormal twitch or contraction of the eyelid or surrounding facial muscles.
|
|
|
What do maculae detect?
|
Linear acceleration and head tilt (position). Maculae are located in the utricle and saccule (of the vestibule).
|
|
|
Utricle and saccule
|
Vestibular organs of the inner ear; both contain maculae. Utricle is positioned horizontally, and saccule vertically.
"Sac hanging down" Maculae contain otoliths sitting on a gelatinous layer within which mechanoreceptor hair cells are embedded. |
|
|
Lateral vestibulospinal tract
|
Cell bodies are located in the lateral vestibular nucleus (Deiter's nucleus) which is located on the lateral floor of the 4th ventricle in the pons and rostral medulla. Axons descend in the medial descending motor system (anterior funiculus) and are important in maintaining balance and extensor tone.
|
|
|
Medial vestibulospinal tract
|
Cell bodies are located in the medial vestibular nucleus (lateral pons and rostral medulla). Axons descend in the medial descending motor system (anterior funiculus) only down to the cervical spine. Important for controlling head and neck position.
|
|
|
Functions of superior olivary nucleus
|
1) Analysis of horizontal direction of sound input
2) Control of stapedius muscle (to mute yourself to your own sound), via stimulation of facial nerve |
|
|
Chorda tympani
|
The CT branches off the facial nerve just before its exit through the stylomastoid foramen. This nerve carries SVA fibers from the anterior 2/3 of the tongue (taste) and GVE fibers (preganglionic parasympathetic) to the submandibular ganglion, to supply the submandibular and sublingual glands. Fibers of CT travel to their destination via the lingual nerve (of V3).
|
|
|
The pterygopalatine ganglion houses postganglionic cell bodies of which nerves?
|
Parasympathetic nerves that innervate the nasal, palatine, and lacrimal glands. This ganglion receives fibers mainly from the greater petrosal nerve (of the facial nerve).
|
|
|
Name the two targets of the autonomic fibers of the facial nerve.
|
1) Lacrimal gland
2) Submandibular and sublingual glands |
|
|
Name the two branches of the facial nerve that carry preganglionic autonomic nerve fibers.
|
1) Greater superficial petrosal nerve
2) Chorda tympani |
|
|
Through which part of the internal capsule do the descending fibers that innervate the facial nucleus pass?
|
Genu
|
|

|
Spinal trigeminal tract
* at the level of the pyramidal decussation, caudal part of caudal medulla |
|
|
Spinal trigeminal nucleus
* at the level of the posterior column nuclei, rostral part of caudal medulla. Caudal part of Inferior olives are seen. |
|
|
Caudal third of hypoglossal nucleus
* at the level of rostral portion of the caudal medulla, caudal third of inferior olive, rostral portions of the sensory decussation (internal arcuate fibers) |
|

|
Solitary nuclei and tract
* at the level of the caudal half of the rostral medulla, middle of inferior olive, 4th ventricle flared open, restiform body is present |
|

|
Dorsal and ventral cochlear nuclei
* at the level of the rostral half of the rostral medulla, restiform bodies, lateral recesses of the 4th ventricle |
|
|
Facial nucleus (and facial nerve, laterally)
* at the level of the pons-medullary junction |
|
|
Vestibular nuclei (lateral, medial, and superior) and juxtarestiform body
* at the level of the pons-medullary junction |
|
|
What symptom would you expect in a pt with a lesion of the nerve to the stapedius?
|
Hyperacusis
|
|
|
Name the ascending auditory pathway that arises from the cochlear nerve.
|
Lateral lemniscus
|
|
|
What nucleus of the brainstem receives projections from the vestibular nuclei and plays a role in pharyngeal muscle activity?
|
Nucleus ambiguus (SVE fibers that enter CN XI, X, and XI)
|
|
|
Dix-Hallpike maneuver
|
A diagnostic test for Benign Paroxysmal Positional Vertigo (BPPV) in which the pt's head is rotated and extended, and after 5-10 s nystagmus is observed (positive test).
|
|
|
If a pt rotates leftward on a stool for 30 seconds and then stops, what type of nystagmus will be observed?
|
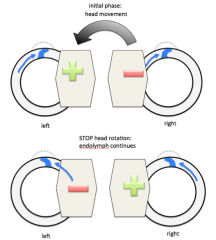
Post-rotatory nystagmus --> right horizontal nystagmus.
|

