![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
88 Cards in this Set
- Front
- Back
|
What is Parkinson's Disease?
|
A prevalent neurologic disorder characterized by progressive motor dysfunction due to tremor, rigidity, bradykinesia, and disturbance of posture
know the symptoms! |
|
|
What are the signs and symptoms of PD due to?
|
The signs and symptoms of PD are due to the progressive degeneration of the inhibitory dopaminergic pathway projecting from the substantia nigra to the caudate nucleus.
|
|
|
What do individuals of PD have a deficiency of?
|
Thus, individuals with PD have a deficiency of dopamine.
|
|
|
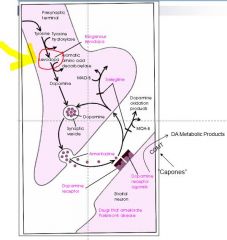
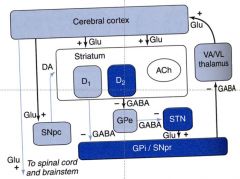
Schematic Diagram of the basal ganglia
|

Focus on the SNpc
- Resting tremor - Loss of Inhibition - Cholinergic Neurons act in deposition - Cholenergic = stimulus - Dopamine = inhibits |
|
|
PD and Dopamine receptors:
What is the cause of PD? |
D1 (increase cAMP) and D2 (decrease cAMP) receptors are abundant in the striatum and are the most important receptors in the cause and treatment of PD.
So you have a lose of Dopamine which inhibits movement so this is why you see tremor |
|
|
PD
wiki style |
a degenerative disorder of the central nervous system. The motor symptoms of Parkinson's disease result from the death of dopamine-generating cells in the substantia nigra, a region of the midbrain; the cause of this cell death is unknown. Early in the course of the disease, the most obvious symptoms are movement-related; these include shaking, rigidity, slowness of movement and difficulty with walking and gait. Later, cognitive and behavioural problems may arise, with dementia commonly occurring in the advanced stages of the disease.
|
|
|
What are the main symptoms of PD?
|
Tremor
Bradykinesia Rigidity |
|
|
What kind of tremor will a PD pt have?
|
Tremor – pill rolling contractions. Often present at rest but disappear during purposeful movement
|
|
|
What is Bradykinesia?
|
Bradykinesia – decreased spontaneous movement, loss of normal associated movement, slow initiation of movement
|
|
|
What is Rigidity of PD due to?
|
Rigidity – due to increased muscle tone
|
|
|
What will a PD pt posture look like?
|
Posture – progressive stooped position
|
|
|
Are psychological changes associated with PD?
|
Psychological changes such as depression and dementia
|
|
|
What is the underlying MOA for PD pts?
|
Normal voluntary movement is controlled by a balance of dopaminergic and cholinergic nervous activity. In PD, there is a deficiency of dopamine, allowing cholinergic dominance
remember Cholinergic is stimulatory |
|
|
What are Parkinson varients?
|
It has become apparent that what has been called Parkinson’s Disease is not a single disorder.
Symptoms vary and response to drugs vary. |
|
|
What is Parkinsonism?
|
this is from wiki but read it****
neurological syndrome characterized by tremor, hypokinesia, rigidity, and postural instability.[1] The underlying causes of parkinsonism are numerous, and diagnosis can be complex.[2] While the neurodegenerative condition Parkinson's disease (PD) is the most common cause of parkinsonism, a wide-range of other etiologies may lead to a similar set of symptoms, including some toxins, a few metabolic diseases, and a handful of non-PD neurological conditions.[3] Its most common cause is as a side effect of medications, |
|
|
What are the 2 ways we can pharmacologically intervene to treat PD?
|
Decrease function of striatothalamic cholinergic pathway
Increase function of nigrostriatal dopaminergic pathway |
|
|
What is our first line tx for PD?
|
Levodopa
|
|
|
What is Levodopa?
|
immediate precursor of dopamine which will cross the blood brain barrier
|
|
|
What is the MOA of Levodopa?
|
Pharmacological properties – MOA is the conversion of l-dopa to dopamine in CNS, thus increasing dopamine in the basal ganglia
Dopamine will not cross the BBB BUT....L-dopa will --> once across the BBB converted into dopamine |
|
|
Diagram of L-dopa
|
|
|
|
What are the CNS changes due to Levodopa?
|
No change in muscle tone or movement in normals.
Bradykinesia and rigidity are reversed quickly; reversal of tremor requires continued therapy Changes in mood associated with PD are reversed; patients more alert and interested in environment. Dementia may not reverse |
|
|
What are the cardiovascular effects of Levodopa?
|
Cardiovascular
Asymptomatic (usually) orthostatic hypotension Dopamine stimulates both alpha and beta receptors Cardiac stimulation |
|
|
What are the Endocrine effects of Levodopa?
|
Endocrine
Dopamine important in regulation of anterior pituitary function Prolactin secretion inhibited Little change in growth hormone secretion |
|
|
What do you need to consider when taking Levodopa and Food?
|
Well absorbed orally but can be altered by:
- Rate of gastric emptying - pH of gastric fluids - Degradation by enzymes - Dietary protein |
|
|
Where is Ldopa metabolized?
|
95% of l-dopa is metabolized in the periphery to dopamine;
metabolism may be increased with prolonged therapy |
|
|
What can happen with long term exposure of ldopa and metabolism?
|
metabolism may be increased with prolonged therapy
|
|
|
What happens to the L-dopa metabolites?
|
Metabolites excreted in urine
|
|
|
What is Parcopa?
|
Parcopa – orally dissolving, immediate release dopa + carbidopa mixture is now available.
|
|
|
What are adverse SHORT term effects of L-dopa?
|
Dose dependent; tolerance may develop
GI – nausea, vomiting (80%) CVS – orthostatic hypotension (30%), cardiac arrhythmias |
|
|
What are LONG term effects of L-dopa?
|
Long term effects – severity correlates with the degree of clinical improvement, duration of therapy and dose. No tolerance develops
****Abnormal involuntary movements (dyskinesia) (80% after 1 year). Reduction in dosage required |
|
|
What is the difference between the LONG term efftects:
"On-Off" syndrome & "End of Dose" |
“On-Off” syndrome – oscillations in performance involving rapid changes from akinesia to dyskinesia (different from “end of dose”).
End of Dose: took drug a long time ago and have metabolized it all....so become frozen |
|
|
What are some important drug interactions you need to know fir L-dopa?
***Objective |
1. Pyridoxine
2. “Typical” antipsychotic drugs 3. MAO inhibitors 4. Anticholinergic drugs 5. Tricyclic antidepressants |
|
|
What do Pyridoxine (vitamin B6) interactions cause with l-dopa
|
increases peripheral conversion of dopa to dopamine
|
|
|
Typical” antipsychotic drugs are dopaminergic antagonists and thus counteract the effects of dopa
|
MAO inhibitors increase the effects of dopa, may lead to hypertensive crises, inhibits metabolism of L-Dopa….used to treat depression
|
|
|
Anticholinergic drugs may slow gastric emptying time and decrease absorption of l-dopa
|
Tricyclic antidepressants – may aggravate hypotensive symptoms
|
|
|
Next drug to treat PD
|
Carbidopa
|
|
|
What is Carbidopa
|
L-aromatic amino acid decarboxylase is responsible for the conversion of dopa to dopamine.
Its activity causes 95% of a dose of dopa to be converted to dopamine before entering the CNS. |
|
|
What is the MOA for Carbidopa?
|
Carbidopa is an inhibitor of the peripheral decarboxylase and allows greater amounts of dopa to enter the CNS. Only available in combination with l-dopa
so you increase the amount of drug to the brain carbidopa --> DOES NOT cross the BBB |
|
|
What are the advantages of Carbidopa?
|
Allows reduction in dopa dose
Nausea and vomiting are decreased Cardiac side effects decreased B6 Pyridoxine antagonism prevented |
|
|
Compare how available l-dopa and carbidopa are for tx.
|
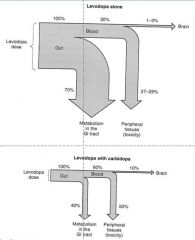
|
|
|
which drug is more available in the CNS?
|
Carbidopa
|
|
|
What are the adverse side effects of Carbidopa?
|
Increased central side effects of dopa
Early development of long term side effects possible Activation of COMT pathway |
|
|
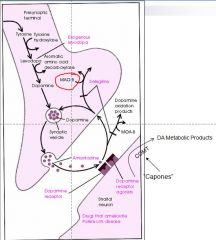
What is the COMT pathway?
|
In the prefrontal cortex, however, there are very few dopamine transporter proteins, and dopamine is inactivated instead by reuptake via the norepinephrine transporter (NET), presumably on neighboring norepinephrine neurons, then enzymatic breakdown by catechol-O-methyl transferase (COMT) into 3-methoxytyramine
|
|
|
What 2 drugs act as COMT inhibitors?
|
Tolcapone
& Entacapone Pneumonic: (Remember Al Capone and Chicago Organized Mob) |
|
|
What is the MOA of COMT inhibitors?
|
Pharmacological properties – drugs inhibit COMT, thereby increasing the duration of action of l-dopa and dopamine (COMT inactivates l-dopa and dopamine).
|
|
|
What is the difference between Tolcapone and Entacapone?
|
There is a difference in these drugs in that tolcapone is highly lipid soluble and reaches CNS. Entacapone does not
|
|
|
diagram of how Capones work (COMT inhibitors)
|

COMT --> depgrades dopamine in the synapase so Capones block COMT
|
|
|
What are adverse effects of COMT inhibitors?
|
Adverse reactions – diarrhea, bright yellow discoloration of urine, increased l-dopa side effects.
Increased amino-transferase activity (indication of hepatotoxicity) with tolcapone may require DC. Apparently not a problem with entacapone |
|
|
What is the preferred drug due to side effects:
Tolcapone or Entacapone? |
Entacapone
|
|
|
what are the clinical uses of the COMT inhibitors?
|
Clinical uses – adjunct to l-dopa in patients with stable PD and in patients with end of dose (“wearing off”) problems with l-dopa/carbidopa therapy.
|
|
|
What is Stalevo?
|
A combination of carbidopa + l-dopa + entacapone is now available (Stalevo).
|
|
|
End COMT inhibitors
|
Begin Dopamine Agonists
|
|
|
What are your dopamine agonists?
|
Ergot compounds which possess dopaminergic activity.
Bromocryptine (bro moe krip’ teen – Parlodel) is the prototype. |
|
|
What is the MOA of dopamine agonist?
|
Act by direct stimulation of dopamine receptor
Rapidly absorbed, effective levels reached quickly and persists 3-4 times longer than l-dopa May prove useful as adjunct to l-dopa therapy and allow decrease in dopa dosage. |
|
|
Are dopamine agonists used much today?
|
Not used too much anymore
LSD --> hallucinattions |
|
|
What are your Non-ergot DA Agonists
|
Ropinirole
& Pramipexole Direct stimulation of DA receptors in striatum |
|
|
What is the 1st line choice for PD?
|
Ropinirole
and Pramipexole |
|
|
What do the Non-ergot DA agonists do?
|
Pramipexole may also have a neuroprotective effect, slowing progression of PD
Produce less dyskinesia and lower incidence of repsonse fluctuation |
|
|
Diagram of Dopamine Agonists
|

|
|
|
Adverse effects
Non-ergot DA agonists |
Nausea, dizziness, somnolence, headache, hallucinations, impulse control problems****
Less dyskinesia and on-off syndrome Syncope or hypotension can occur early in treatment with ropinirole Pramipexole can cause sudden onset of sleep with no warning |
|
|
Non-ergot DA agonists
Use***EXAM!!!!!!!!!!! |
Used as initial therapy (without l-dopa) or as adjunctive therapy with l-dopa
|
|
|
What is another use of Ropinorole and Pramipexole?
|
Ropinorole and pramipexole have been approved for the treatment of restless leg syndrome. Other DA agonist may also be effective.
|
|
|
What if your PD pt just froze?
CANNOT MOVE.....what drug can you give him/her? |
Apomorphine
An old drug with a new use. Apomorphine is a non-ergot DA agonist recently approved for rescue treatment of PD patients with “off” episodes (freezing). Is given by SC injection Adverse effects include vomiting, orthostatic hypotension and syncope. |
|
|
This is an ANTIVIRAL drug found to be effective against PD.
|
Amantadine
|
|
|
Amantadine An antiviral agent found to be effective against PD.
MOA? |
Apparently acts by increasing dopamine release from intact dopaminergic neurons. Also blocks NMDA receptors (glutamate receptor).
Is effective quickly but for short time (6-8 weeks). Also used to control dyskinesias occurring with l-dopa therapy late in progression of disease. |
|
|
What is the disadvantage of Amantadine?
|
Limitation of amantadine --> only works a month or 2 and then has limited value
|
|
|
picture of Amantadine
|

|
|
|
What are the adverse effects of Amatadine?
|
Adverse effects – are mild and reversible and include:
Hallucinations, confusion, and nightmares Insomnia, dizziness, lethergy, slurred speech Long term use may result in livido reticularis |
|
|
What is Livido reticularis?
|
Livido reticularies -> see white streaks --> vasocontriction --> localized vasoconstriction and get discoloration of the skin
|
|
|
What is a drug that effects mainly the tremor of PD?
|
Anticholinergic drugs - used as adjunct to l-dopa therapy
|
|
|
Anticholinergic drug MOA
|
Pharmacological properties – these agents block the unopposed cholinergic effects in the basal ganglia of PD patients.
|
|
|
What are your Anticholinergic drugs
|
Trihexyphenidyl
& Benztropine |
|
|
Trihexyphenidyl and benztropine
what is main use? |
Decrease tremor
Little effect on rigidity and bradykinesia Generally have little peripheral effect, but may reduce some autonomic symptoms |
|
|
Trihexyphenidyl and benztropine
Adverse reactions |
CNS – confusion, delerium, somnolence, hallucinations
Peripheral – may produce cycloplegia, constipation, and urinary retention in certain patients |
|
|
When do you see PD?
|
Generally older pts have this disease
Most are in 50s and 60s who develop Don’t see symotopms till see 80% of nerves die |
|
|
What are MAO B Inhibitors
|
Selegiline
& Rasagiline |
|
|
MOA of for the MAO-B inhibitors
|
Pharmacological properties – drugs specifically inhibits MAOB. This decreases catabolism of DA
|
|
|
What is a benefit of Rasagiline?
|
Rasagiline may have neuroprotective effect. Slows progression of the disease
|
|
|
MAO B inhibitors
Adverse effects |
Nausea (10%), dizziness (7%), hallucinations, confusion, depression
Insomnia if taken late in the day (take early in day) Dose must be kept low (10 mg/day or less) to retain specificity for MAOB, otherwise adverse reactions associated with non-specific MAOs occur. Potential for hypertensive crisis |
|
|
MAO-B picture
|
|
|
|
What MAOB inhibitor can be used as transdermal patch for the tx of depression?
|
selegiline
|
|
|
GOAL of Rx for PD
|
No cure of underlying pathology (although gene therapy is being tested)
Drug + physiotherapy + exercise + psychological support → provide maximal symptomatic relief and permits a near normal lifespan. |
|
|
Management of PD pic
|

|
|
|
What is Huntington's Disease?
|
HD is a genetic disorder characterized by progressive chorea and dementia.
|
|
|
What is the Tx for Huntington's Disease?
|
Tetrabenazine
|
|
|
What does Tetrabenazine do?
|
Acts by depleting CNS monoamines (DA)
|
|
|
Adverse effects of Tetrabenazine
|
Adverse rxns – hypotnesion, sedation, depression.
|
|
|
make sure you understand this shit......
|
|

