![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
DDx of blood stained nappy
1. Red blood 2. Melaena |
1.
- Constipation with fissure (common) - Rectal polyps - Campylobacter/shigella/C. difficile - Intussusception (important to exclude) - CMPA |
2.
Oesophagitis secondary to GORD Duplication cyst |
|
|
What are the types of nappy dermatitis?
|
1. contact irritant
2. candidal infection 3. bacterial infection 4. seborrhaeic nappy rash 5. psoriatic nappy rash 6. erosive nappy rash (after diarrhoea) |
|
|
|
What is the management of erosive nappy rash?
|
Effective barrier cream e.g. orabase paste. No need for steroids or antifungals.
|
|
|
|
What is the management of contact irritant dermatitis?
|
- use superabsorbent nappies, change frequently
- barrier cream e.g. zinc and castor oil, lanolin - beware that superimposed infections are common - may need to add 1% hydrocortisone + antifungal, BD |
|
|
|
How do you differentiate between contact irritant dermatitis and candidal infection in nappy rash?
|
- contact irritant spares the creases, involves erythema and 'glazing' of skin, and has no satellite lesions
- candida is scaly/vesicopustular, involves creases with cheesy exudate, and has satellite lesions |
|
|

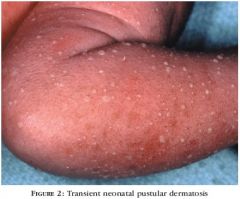
what rash is this
|
contact irritant dermatitis
|
|
|

what rash is this?
|
candida nappy rash - note satellite lesions, and involvement of flexor creases
|
|
|

what rash is this?
|
candida nappy rash - note cheesy exudate and involvement of flexor creases
|
|
|
|
describe seborrhoeic nappy rash
|
- salmon coloured
- does not have the usual yellowish plaques that seborrhaeic dermatitis usually has - especially involves creases - has poorly defined margins, unlike psoriasis |
|
|
|
what is the management of seborrhoeic nappy dermatitis?
|
1% hydrocortisone + anticandidal preparation BD/TDS
|
|
|
|
what are some examples of barrier creams?
|
zinc and castor oil cream, liquid paraffin 10% in zinc paste, Bepanthen ointment, Nappy Mate paste, Sudocrem.
|
|
|
|
what are some antifungal topical agents that can be used in nappy rash?
|
1. nystatin 100 000 units/g cream topically, 3 times daily
2. an imidazole cream (e.g. clotrimazole, ketoconazole) topically, twice daily. |
|
|
|
when steroid preparations are needed in nappy rash, what should be used/avoided?
|
hydrocortisone 1% is the preferred topical corticosteroid, but on occasions a slightly stronger preparation such as methylprednisolone aceponate 0.1% ointment may be required for short periods. Potent corticosteroids should be avoided as the nappy area is prone to atrophy, striae and gluteal granuloma.
|
|
|
|
what are the common causes of nappy rash?
|
irritant
candidiasis seborrhoeic dermatitis psoriasis miliaria atopic dermatitis |
|
|
|
what are some less common causes of nappy rash?
|
staph folliculitis, impetigo
strep perianal cellulitis or vulvovaginitis HSV tinea gluteal granuloma zinc deficiency Langerhans cell histiocytosis Kawasaki disease congenital syphilis |
|
|
|
what is the treatment for a staph nappy rash?
|
Mild/localised: mupirocin 2% ointment topically, 3 times daily for 7 days.
Widespread/severe: flucloxacillin 12.5 mg/kg orally, 6-hourly for 7 days |
for penicillin hypersensitivity: cephalexin, roxithromycin
|
|
|
what is the treatment for strep nappy rash?
|
phenoxymethylpenicillin 12.5 mg/kg orally, 6-hourly for 10 days
|
|
|
|
what is the management of herpetic nappy rash? (painful ulcers, vesicles, oedema - send a swab for confirmation)
|
conservative management unless severe, in which case admit and give IV aciclovir
|
|
|

|
candida nappy rash
|
|
|

|
candida nappy rash
|
|
|

|
candida nappy rash
|
|
|

|
psoriatic diaper rash
management - same as irritant diaper rash |
|
|

|
psoriatic nappy rash
|
|
|
|
ddx of oedema in neonate
|
idiopathic
prematurity erythroblastosis fetalis - hypoproteinaemia nonimmune hydrops congenital nephrosis Hurler syndrome |
|
|
|
ddx of pallor in neonate
|
anaemia
asphyxia erythroblastosis fetalis subcapsular haematoma of liver or spleen subdural haemorrhage transfusion (twin or fetal maternal) |
|
|
|
ddx of hair tuft over lumbosacral spine
|
ocult spina bifida
sinus tract tumour |
|
|

appears day 1-3
persists up to one week contains eosinophils involves trunk, face, extremities |
erythema toxicum
|
|
|

deeper, blue mass
can trap platelets and produce DIC |
cavernous haemangioma
|
|
|
more common in black neonates
contains neutrophils vesiculopustular chin, neck, back, extremities, palms, soles lasts 2-3 days |
benign pustular melanosis
|
|
|
|
ddx of vesicular rash in neonate?
|
erythema toxicum (benign)
pustular melanosis (benign) HSV staphylococcal skin infection |
|
|
|
ddx of skin fragility, extensibility with joint hypermobility
|
Ehlers Danlos syndrome
Marfan syndrome congenital contractural arachnodactyly other collagen synthesis disorders |
|
|

minute, profuse, yellow-white papules
forehead, nose, upper lip, cheeks |
sebaceous hyperplasia
|
disappear within 1st few wks of life
|
|

often on face, gingivae, midline of palate (Epstein pearls)
|
milia
|
exfoliate spontaneously
|
|

|
sucking blister from in utero sucking
|
resolves rapidly
|
|

|
sucking pad (callus)- intracellular oedema and hyperkeratosis
|
|
|
|
What is the usual time pattern of physiological jaundice?
|
Appears day 3
Peaks day 5-7 Resolves by day 14 |
|
|
|
What is the most likely cause of early (Day 1-2) jaundice?
|
Haemolytic jaundice, e.g. Rhesus, ABO
|
|
|
|
What are the likely causes of late (day 14+) jaundice?
|
Breast milk jaundice (common)
Conjugated jaundice (uncommon) Glucuronyl transferase deficiency (v rare) |
|
|
|
What are the common causes of jaundice on days 3-10?
|
Physiological, complicated/uncomplicated
G6PD deficiency |
|
|
|
For babies with physiological jaundice, what factors increase the risk of kernicterus?
|
Acidosis
Drugs e.g. sulphonamides, which displace bilirubin from albumin Hypoalbuminaemia Prematurity Bruising Cephalohaematoma Polycythaemia Chinese Delayed meconium Breast feeding |
|
|
|
Definition of severe jaundice
|
Term baby with SBR > 450
Haemolytic jaundice Preterm baby |
|
|
|
Features of kernicterus
|
Hypertonia progressing to opisthotonia
Seizures Death |
|
|
|
Histological features of kernicterus
|
Bilirubin staining of basal ganglia
|
|
|
|
Late sequelae of kernicterus
|
Sensorineural hearing impairment
Cerebral palsy Ataxia Choreoathetosis |
|
|
|
What is the age cutoff for TcB?
|
35 weeks
|
|
|
|
When should visual assessments of jaundice be performed?
|
q8-12 hours in the first 48hours of life
|
|
|
|
How is a visual assessment of jaundice performed?
|
Blanch the skin, observe for lemon yellow turning to deeper orange yellow
Kramer's rule: craniocaudal progress |
|
|
|
Describe the zones of jaundice as per Kramer's rule
|
1 - head/neck (SBR 100)
2 - thorax (SBR 150) 3 - pelvis, thighs (SBR 200) 4 - legs excluding feet, arms excluding hands (SBR 250) 5 - hands and feet (SBR > 250) |
|
|
|
When is visual assessment of jaundice unreliable?
|
Phototherapy - blanches skin
Darker skinned babies |
|
|
|
What are the indications for TSB?
|
1. TcB within 50micromol of phototherapy level
2. Any baby with jaundice < 24h 3. Any term baby with TcB > 250 4. Any preterm baby with TcB > 200 5. Any baby if there is doubt about degree of jaundice 6. Any unwell baby with jaundice 7. 24h after ceasing phototherapy, to look for rebound |
|
|
|
When should TSB be repeated?
|
12-24h if the TcB was below the phototherapy level
4-6h if the TcB was more than 30 above the phototherapy level |
|

