![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
|
Normal values for theses parameters at birth
- RR - HR - sBP & dBP - Weight - Glucose |
RR : 40-60 breaths/min
HR : 120-160 BPM when awake sBP : 50-80 mm Hg dBP : 30-40 mm Hg Weight : 2500-4500 g Glucose : >2.6 mmol/L (45 mg/dL) |
|
|
Classification of newborns by gestational age :
- Preterm - Term - Postterm |
- Preterm < 37 weeks
- Term 37-42 weeks - Postterm > 42 weeks |
|
|
Classification of newborns by birth weight :
- Small for gestational age (SGA) - Appropriate for gestational age (AGA) - Large for gestational age (LGA) |
SGA : 2 SD < mean weight for GA or <3rd percentile
AGA : within 2 SD of mean weight for GA LGA : 2 SD > mean weight or >97th percentile |
|
|
How can gestational age be determined after birth.
|
Gestational age can be determined after birth using Dubowitz/Ballard scores
- assessment at delivery of physical maturity and neuromuscular maturity. - higher score means greater maturity (increased GA) - -10 = 20 weeks; +50 = 44 weeks - ideal = 35-40 which corresponds to 38-40 weeks - only accurate +/- 2 weeks |
|
|
Causes of SGA
|
- Most common cause : idiopathic
- Maternal disease e.g. pre-eclampsia - Drugs, EtOH, smoking, TORCH - Chromosomal - Multiple pregnancy - Placental insufficiency |
|
|
Problems with pre-term newborns
|
- Respiratory distress syndrome, apnea of prematurity, chronic lung disease, bronchopulmonary displasia
- Feeding difficulties, necrotizing enterocolitis (NEC) - Hypocalcemia, Hypoglycemia, Hypothermia - Anemia, jaundice - Retinopathy of prematurity - Intracranial/ hemorrhage - Patent ductus arteriosus |
|
|
Problems with post-term infants
|
Hypoxia
Meconium aspiration Hypoglycemia |
|
|
Causes of SGA infants
|
Extrinsic causes
- placental insufficiency - poor nutrition - hypertension - multiple pregnancies - drugs - EtOH - smoking Intrinsic causes - potential infections (TORCH) - congenital abnormalities - syndromal - idiopathic |
|
|
Cause of LGA infants
|
- Maternal diabetes
- Racial or familial factors - Certain syndromes |
|
|
Problems with SGA infants
|
Perinatal hypoxia
Hypoglycemia, hypocalcemia, hypothermia Hyperviscosity, jaundice Hypomotility Patent ductus arteriosus |
|
|
Apgar Score
|

|
|
|
Drugs used in neonatal resuscitation
|
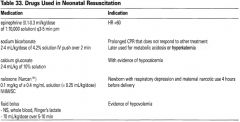
|
|
|
Problems with LGA infants
|
Birth trauma
Perinatal hypoxia Meconium aspiration Respiratory distress syndrome Transient tachypnea of newborn (TTN) Persistent pulmonary hypertension Jaundice, hypoglycemia, hypocalcemia, polycythemia |
|
|
Routine neonatal care
|
Performed in delivery suite
1. Erythromycin ointment - applied to both eyes for ophtalmia neonatorum (gonorrhea, chlamydia) prophylaxis 2. Vitamin K IM - to avoid hemorrhagic disease of newborn 3. Screening tests - Quebec : type I tyrosinemia, Phenycetonuria, congenital hypothrydoidism - Sickle cell anemia if at risk 4. If mother Rh negative : send cord blood for blood group, and direct antiglobulin test 5. If indicated : G6PD deficiency testing 6. if mother HBsAg positive : give HBIg and start hepatitis B vaccine series |
|
|
Characteristics of a depressed newborn
|
A depressed newborn lacks one or more of the following characteristics for a normal newborn :
- pulse > 100 BPM - cries when stimulated - actively moves all extremities - has a good strong cry Between 5-10% of newborn babies require assistance with breathing after delivery. |
|
|
Etiology of respiratory distress in the Newborn
|
Respiratory problems
- Respiratory distress syndrome / Hyaline Membrane disease - CNS depression - Meconium aspiration - Pneumoniae - Pneumothorax Anemia (severe) - Erythroblastosis fetalis - Secondary hydrops fetalis Maternal causes - Drugs / anesthesia - Diabetes mellitus - Pregnancy induced hypertension Congenital malformations/Birth injury - Nuchal cord Shock / Cyanosis / Congenital heart disease Other - Hypothermia - Hypoglycemia - Infection |
|
|
Important elements at maternal history
|
- Prenatal care
- Illnesses - Uses of drugs - Labour - Previous high risk pregnancies - Infections during pregnancy - Current infections - Duration of ruptured membranes - Blood type and Rh status - Amniotic fluid status - Gestational age - Meconium - Apgar scores |
|
|
When to assess Apgar scores
|
at 1 and 5 minutes
If < 7 at 5 minutes then reassess q5 minutes, until >7 do not wait to assign Apgar score before initiating resuscitation |
|
|
What's verified in the Apgar score?
|
Heart rate
Respiratory rate Tone Irritability Colour |
|
|
Initial resuscitation of a newborn
|
1- Anticipation : know maternal history, history of pregnancy, labour and delivery, prepare equipment
2- Steps to take for all infants (before ABCs) + Provide warmth : warm towels, dry the newborn (no wet towels) + Position and clear airway + Stimulate infant : rub back gently or flick soles of feet except if meconium present (suction first) + Assess breathing, heart rate and colour 3- Airway + If meconium is present and baby is vigorous (high apgar), suction mouth and nose after delivery of head + If meconium is present and baby is not vigorous : free flow O2, intubate and suction trachea + If meconium is absent, remove secretions by wiping mouth and nose with towel or gentle suction of mouth then nose 4- Breathing + if HR < 100 or apneic, apply positive pressure ventilation + PPV at rate of 40-60/min, 100% O2 with enough pressure to see visible chest expansion 5 - Circulation + if HR <60 after 30 sec of effective ventilation, start chest compressions + chest compressions at lower 1/3 of the sternum at 1/3 of the AP depth at a rate of 120 events/min (3 compressions : 1 ventilation) |
|
|
Chronic non bacterial perinatal infections
|
TORCH
Toxoplasmosis Others Rubella virus Cytomegalovirus, Chickenpox, Coxsackievirus HSV, HIV, HBV Erythema infectiosum (Parvovirus B19), EBV Syphillis |
|
|
Sepsis in neonates
- Risk factors - Organisms - Signs |
Early Onset (0-5 days)
- Vertical transmission : 95% present within 24 hours - Risk factors + Maternal infection : UTI, GBS positive, previous child with GBS sepsis or meningitis + Maternal fever, leucocytosis, chorioamnionitis + Prolonged rupture of membranes (> 18 hours) + Preterm labour - Pathogens : GBS, E. Coli, Listeria Late oset (5-28 days) - Acquired after birth - Most common in preterm infants in NICU (due to coagulase negative staph - Also in healthy, full-term - Same pathogens as early onset sepsis + Streptococcus, Meningococcus, Staphylococcus Signs of sepsis in neonates - No reliable absolute indicator of occult bacteremia in children <3 Mo, most consistent result has been WBC < 5 - Temperature instability (hypothermia/hyperthermia) - Respiratory distress, cyanosis, apnea - Tachycardia / bradycardia - Lethargy, irritability - Poor feeding, vomiting, abdominal distention, diarrhea - Hypotonia, seizures, confusion, lethargy, coma - Jaundice, hepatomegaly, petechiae, purpura |
|
|
Newborn Cyanosis
|
2 Major types
1) Peripheral cyanosis : can be normal transiently but may indicate sepsis, temperature instability 2) Central cyanosis (deoxygenated hemoglobin or abnormal hemoglobin) - Upper respiratory : choanal atresia, macroglossia, airway hypoplasia, laryngeal web/cyst, foreign body - Lower respiratory : pneumonia, meconium aspiration syndrome, pneumothorax, diaphragmatic hernia, AV fistula, pulmonary hypoplasia - Congenital heart disease, PPHN - CNS (asphyxia, seizure, narcotics, sedatives) - Myasthenia gravis, botulism - Polycythemia - Sepsis - Methemoglobinemia, Carboxyhemoglobinemia |
|
|
Management of newborn cyanosis
|
ABGs
Hyperoxic test to r/o CHD CXR |
|
|
Persistent pulmonary hypertension of the newborn (PPHN)
|
Clinical Presentation
- 2/1000 live births - Presents within 12 hours of birth with severe hypoxemia/cyanosis but relatively mild respiratory distress Pathophysiology - Due to persistance of fetal circulation as a result of persistent elevation of pulmonary HTN - R>L shunt through PDA, foramen ovale, intrapulmonary channels = decreased pulmonary blood flow and hypoxemia = further pulmonary vasoconstriction Risk factors - Asphyxia, MAS, RDS, sepsis, structural abnormalities (diaphragmatic hernia, pulmonary hypoplasia) - Primary PPHN occurs in absence of risk factors Investigations Heart U/S |
|
|
Treatment of PPHN
|
Maintain good oxygenation in at risk infants
O2 given early and tapered slowly, minimize stress and hypoxia, alkalinization, inotropes Mechanical ventilation, high frequency oscillation Nitric oxyde Extracorporeal membrane oxygenation used in some centers |
|
|
Clinical presentation of respiratory distress in the newborn
|
Tachypnea : RR > 60/min
Tachycardia : HR > 160/min Grunting, Intercostal indrawing, nasal flaring Duskiness, central cyanosis Decreased air entry Crackles on auscultation |
|
|
Differential diagnosis of respiratory distress
|
Pulmonary
- RDS - Transient tachypnea of the newborn - Meconium aspiration syndrome - Pleural effusions, pneumothorax - Congenital lung malformations Infectious - sepsis - pneumonia Cardiac - congenital heart disease - PPHN Hematologic - blood loss - polycythemia Anatomic -TE fistula - Congenital diaphragmatic hernia - Upper airway obstruction (choanal atresia, Pierre-Robin sequence, cleft palate) Metabolic - hypoglycemia - inborn errors of metabolism Neurologic - CNS damage - Drugs withdrawal syndromes |
|
|
Pathophysiology of respiratory distress syndrome
|
Surfactant deficiency --> poor lung compliance due to high alveolar surface tension and atelectasis --> decreased surface area for gas exchange --> hypoxia + acidosis --> respiratory distress
Surfactant decreases alveolar surface tension, improves lung compliance and maintains functional residual capacity. There is usually sufficient surfactant production by 36 weeks. |
|
|
Respiratory distress syndrome presentation
|
aka hyaline membrane disease
Presentation - Signs of respiratory distress (tachypnea, tachycardia, grunting, intercostal indrawing, nasal flaring, cyanosis, lung crackles) - Onset within first few hours of life, worsens over next 24-72 hours - Infants may develop respiratory failure and require ventilation CXR : decreased aeration and lung volumes, reticulonodular pattern throughout lung fields with air bronchograms, atelectasis; may resemble pneumonia, if severe can see white-out |
|
|
Respiratory distress syndrome risk factors
|
Prematurity (especiall if < 36 weeks)
Low birth weight Rare at term Maternal diabetes : insulin inhibits the cortisol surge necessary for surfactant synthesis C-section without labour Asphyxia, acidosis, sepsis, meconium aspiration Males > Females Hypothermia Second born twin |
|
|
Prevention of newborn respiratory distress syndrome
|
Steroid therapy for mothers (12 mg Q24H x 2 doses) who are at risk of preterm birth
Monitor Lecithin:sphingomyelin (L/S) ratio with amniocentesis, L/S > 2:1 indicates lung maturity Prophylactic surfactant often given to high risk infants (< 28 weeks) at birth |
|
|
Treatment of newborn respiratory distress syndrome
|
Supportive (O2, assisted ventilation)
Endotracheal surfactant administration |
|
|
Complications of respiratory distress syndrome
|
Bronchopulmonary dysplasia
Pulmonary air leaks (pneumothorax) Increased risk of chronic lung disease |
|
|
Pathognomonic sign of respiratory distress syndrome on CXR
|
"Ground glass" appearance of lungs
|
|
|
Transient Tachypnea of the Newborn (TTN)
Pathophysiology Risk Factors Presentation Treatment Prognosis |
AKA "wet lung syndrome" and respiratory distress syndrome type II
Pathophysiology Delayed resorption of fetal lung fluid --> accumulation of fluid in peribronchial lymphatics and vascular spaces --> tachypnea Risk Factors - full term or near term infant - no labour / short labour - C-Section (lungs are not compressed during passage through pelvic floor) - Diabetic mother / gestational weight > 4500 g - Maternal asthma - Male sex Clinical Presentation - Tachypnea within the first few hours of life, mild retractions, grunting, nasal flaring, without signs of severe respiratory distress - Usually resolves in 24-72 hours - CXR : fluid in fissures, increased vascularity, slight cardiomegaly è Treatment - Supportive Prognosis - full recovery expected within 2-5 days - in the past it was generally believed that TTN was a self-limiting condition which, once resolved, had no long-term sequelae. Current research suggests that children with TTN may be at increased risk of developing wheezing syndromes (such as asthma) in childhood. |
|
|
Meconium Aspiration Syndrome (MAS)
Pathophysiology Risk Factors Presentation Treatment Prognosis |
10-15% of all infants are meconium stained at birth; 5% of meconium stained infants get MAS
Usually associated with fetal distress in Utero or post-term infant + Clinical presentation - respiratory distress within hours of birth - small airway obstruction, chemical pneumonitis --> tachypnea, barrel chest with audible crackles - CXR : hyperinflation, streaky atelectasis, patchy and coarse infiltrates + Complications - Hypoxemia, hypercapnia, acidosis, PPHN, pneumothoarx, pneumomediastinum, pneumonia, sepsis, respiratory failure, death. + Treatment - supportive care, assisted ventilation - ventilated infants often require sedation - may benefit from surfactant replacement (surfactant function is inhibited by presence of meconium) - inhaled nitric oxyde, extracorporeal membrane oxygenation at some centres + Prevention - in utero : careful monitoring - after delivery of the head : suction oro / naspharynx - at birth : intubate and suction below cords if infant is depressed - note : presence of meconium staining alone is NOT and indication for tracheal suctioning. If the infant is vigorous, intubation and suctioning of lower airway is unnecessary. |
|
|
Causes of neonatal hyperbilirubinemia
|

|
|
|
Causes of neonatal jaundice by age
|

|
|
|
Etiology of hypoglycemia in newborns and presentation
|
Glucose < 2.6 mmol/L
Etiology - Decreased carbohydrate storage (premature, IUGR) - Infant of a diabetic mother : maternal hyperglycemia --> fetal hyperglycemia and hyperinsulinism --> hypoglycemia in the newborn infant because of high insulin levels - Endocrine : hyperinsulinism due to islet cell hyperplasia (Beckwith-Wiedemann syndrome), panhypopituitarism - inborn errors of metabolism : fatty acid oxidation defects, galactosemia Presentation : signs often non specific and subtle - lethargy - poor feeding - irritability - tremors - apnea - seizures |
|
|
Beckwith - Wiedemann syndrome
|
Hyperinsulinism dur to islet cell hyperplasia
|
|
|
Management of newborn hypoglycemia
|
- Identify and monitor infants at risk
- Begin oral feeds within first few hours of birth - If hypoglycemic, provide glucose IV (D10, D12,5) - if persistent hypoglycemia (past day 3), hypoglycemia unresponsive to IV glucose, and/or no predisposing cause for hypoglycemia, send the following "critical bloodwork" during an episode of hypoglycemia + insulin + cortisol + GH + beta-hydroxybutyrate + lactate + ammonia + free fatty acids + ABG Treat hyperinsulinism with glucagon and diazoxide |
|
|
Physiologic jaundice pathophysiology and presentation
|
Term infants : 2-3 days of life, resolution by 7 days of life
Pathophysiology - Increased hematocrit - Decreased RBC span - Immature glucuronyl transferase enzyme system (slow conjugation of bilirubin) - Increased enterohepatic circulation |
|
|
Risk factors for neonatal jaundice
|
Maternal factors
- Ethnic group (asian, native american) - Complications during pregnancy (diabetic mother, Rh or ABO incompatibility - Breast feeding Perinatal factors - Birth trauma (cephalohematoma, ecchymoses) - Prematurity Neonatal factors - Infection - Genetic factors - Polycythemia - Drugs - Difficulty establishing breastfeeding |
|
|
CHEAP TORCHES
|
CHEAP TORCHES
Chicken Pox / Shingles Hepatitis B Ebsterin-Barr Virus AIDS Parvovirus B19 Toxoplasmosis Other Rubella virus Cytomegalobirus / Coxsackievirus Herpes simplex virus Every STI Syphilis |
|
|
Breast feeding Vs Breast milk jaundice
|
Breast feeding jaundice is due to a lack of milk production and subsequent dehydration, leading to exaggerated physiologic jaundice.
Breast milk jaundice is caused by the presence of an inhibitor of glucuronyl transferase in breast milk. |
|
|
Signs of pathologic jaundice
|
Jaundice < 24 hours
Serum unconjugated bilirubin rises rapidly or is excessive for patient's age and weight: - >85 umol/L per day or 220 umol/L before 4 days of age Serum conjugated bilirubin >35 umol/L Pesistent jaundice lasting beyond 1-2 weeks of age |
|
|
Necessary investigations for pathologic jaundice
|
Unconjugated hyperbiilirubinemia
- Hemolytic work-up : CBC, blood group, peripheral blood smear, Coombs, Bilirubin - If baby is unwell : septic work up - G6PD screen, TSH Conjugated hyperbilirubinemia - Liver enzymes, Coagulation studies, serum albumin, ammonia, TSH, TORCH, septic work-up, galactosemia screening, metabolic screen, abdominal U/S, HIDA scan, sweat chloride |
|
|
Treatment of unconjugated hyperbilirubinemia
|
Goal : Preventing kernicterus
Breastfeeding does not need to be discontinued, ensure adequate feeds and hydration Get lactation consultant support, mother to pump after feeds 1 - Treat underlying cause 2- Phototherapy 3- Exchange transfusion Phototherapy - Insoluble unconjugated bilirubin is converted to excretable form via photoisomerization - Serum bilirubin should be monitored during and immediately after therapy (risk of rebound because photoisomerization reversible when phototherapy discontinued) - Contraindicated in conjugated hyperbilirubinemia : results in "bronzed" baby - Side effects : hypernatremic dehydration, eye damage, skin rash, diarrhea - Use published guidelines for initation of therapy Exchange transfusion - Prevents toxic effects of bilirubin removal from body - Indications : high bilirubin levels as per published graphs based on age, weeks gestation - Most commonly performed for hemolytic diseaes and G6PD |
|
|
Phototherapy contraindications and side effects
|
Contraindication : conjugated hyperbilirubinemia (causes bronzed baby because of a toxic metabolite)
Side Effects - Hypernatremic dehydration - Diarrhea - Eye damage - Skin rash |
|
|
Kernicterus
- Etiology - Clinical presentations - Prevention - Complications |
Etiology
- Unconjugated bilirubin concentrations exceed albumin binding capacity and bilirubin enters and is deposited in the brain resulting in permanent damage (often basal ganglia or brainstem) - Incidence increases as serum bilirubin levels increase above 340 umol/L - Can occur at lower levels in presence of sepsis, meningitis, hemolysis, hypoxia, hypothermia, hypoglycemia and prematurity Clinical Presentation - Up to 15% of infants have no obvious neurologic symptoms - Acute form : + first 1-2 days : lethargy, hypotonia, poor feeding, high-pitched cry, emesis, seizures + middle of first week : hypertonia, opisthotonic posturing, fever, bulging fontanelle, pulmonary hemorrhage - Chronic form : + hypotonia, delayed motor skills, extrapyramidal abnormalities, gaze palsy, MR, sensorineural hearing loss Prevention - Exchange transfusion Complications - Sensorineural deafness - Choreoathetoid cerebral palsy - Gaze palsy - Mental retardation |
|
|
Complications of kernicterus
|
Sensorineural deafness
Choreathetoid cerebral palsy Gaze palsy Mental retardation |
|
|
Biliary atresia in newborns
- Pathophysiology - Presentation - Diagnosis - Treatment |
Atresia of extra-hepatic bile ducts
Cholestasis and increased conjugated bilirubin after the first week of life Incidence : 1/10 000-15 000 live births Clinical Presentation - Dark urine, pale stool, jaundice (persisting > 2 weeks), abdominal distention, hepatomegaly Diagnosis - HIDA scan - Liver biopsy Treatment - Surgical drainage procedure - Hepatoportoenterostomy (Kasai procedure most successful if before 8 weeks of age) - Usually requires liver transplantation - Vitamins A, D, E and K, diet should be enriched with medium-chain triglycerides to ensure adequate fat ingestion |
|
|
Presentation of bleeding disorders in children
|
Oozing from the umbilical stump
Excessive bleeding from peripheral venipuncture/heel stick sites / IV sites Large caput succedaneum Cephalohematomas Prolonged bleeding following circumcision |
|
|
Causes of bleeding disorders in neonates
|
4 Major categories
1. Increased platelet destruction - Maternal ITP, SLE (autoimmune) - Neonatal alloimune thrombocytopenia (NAIT) - Infection - DIC - Drugs - Extensive localized thrombosis 2. Decreased platelet production/function - Bone marrow replacement - Pancytopenia - Fanconi anemia - Trisomy 13 and 18 3. Metabolic - Congenital thyrotoxicosis - Inborn error of metabolism 4. Coagulation factor deficiencies - Hemophilia A - Hemophilia B - Hemorrhagic disease of the newborn |
|
|
Neonatal alloimmune thrombocytopenia
|
Pathophysiology
- platelet equivalent of Rh disease of the newborn - occurs when mother is negative for human platelet antigen (HPA) and fetus is positive - developmental of maternal IgG antibodies against GPA antigens on fetal platelets Clinical features - petechiae, purpura, thrombocytopenia in otherwise healthy neonate - severe NAIT can lead to intracranial bleeding Diagnosis - Maternal and paternal platelet typing and identification of platelet alloantibodies Treatment - IVIG to mother prenatally, starts in second trimester; treat neonate with IVIG and trasnfusion of infant with washed maternal platelets or donor HPA negative platelets. |
|
|
Neonatal autoimmune thrombocytopenia
|
Pathophysiology
- caused by antiplatelet antibodies from maternal ITP or SLE - passive transfer of antibodies across placenta Clinical Presentation - similar presentation to NAIT, but bleeding usually less severe Treatment - steroids to mother x 10-14 days prior to delivery or IVIG to mother before delivery - IVIG to infant after delivery - transfusion of infant with maternal / donor platelets only in severe cases, as antibodies will destroy transfused platelets |
|
|
Hemorrhagic disease of the newborn
|
Cause by vitamin K deficiency --> PT and PTT are abnormal
Etiology - Neonates at risk of vitamin K deficiency because + vitamin K poorly transferred across the placenta + insufficient bacterial colonization of colon at birth (synthesize vitamin K) + dietary intake of vitamin K inadequate in breastfed infants 2 Types 1) early vitamin K deficiency bleeding - caused by maternal ingestion of oral anticoagulants, anticonvulstants or antituberculosis agents - presents with ICH within the first 24 hours of life 2) classical VKDB - occurs in infants who did not receive vit K at birth and are breastfeeding - presents between days 1 and 7 Prevention Vitamin K IM administration at birth to all newborns |
|
|
Necrotizing enterocolitis
|
Intestinal inflammation associated with focal or diffuse ulceration and necrosis
Primarily affecting terminal ileum and colon (1-5% of preterm newborns admitted to NICU) Pathophysiology - postulated mechanisms of bowel ischemia --> mucosal damage and enteral feeding providing a substrate for bacterial growth and mucosal invasion, leading to bowel necrosis or gangrene and perforation Risk factors - Prematurity - Asphyxia, shocks - Hyperosmolar feeds - Enteral feeding with formula (breast milk can be protective) - Sepsis Clinical Presentation - Distended abdomen - Increased amount of gastric aspirate/vomitus with bile staining - Frank or occult blood in stool - Feeding intolerance - Diminished bowel sounds - Signs of bowel perforation (sepsis, shock, peritonitis, DIC) |
|
|
Diagnosis of necrotizing entercolitis
|
Abdominal X-Ray : pneumonitis intestinalis (intramural air, hallmark of NEC), free air, fixed loop, ileus, thickened bowell wall, portal venous gas
|
|
|
Treatment of necrotizing enterocolitis
|
NPO (minimum 1 week), vigorous IV fluid resuscitation, NG decompression, supportive therapy
TPN Antibiotics (usually ampicillin, gentamycin +/- metronidazole if risk of perforation x 7-10 days) Serial abdominal X-Rays detect early perforation Peritoneal drain / surgery if perforation Surgical resection of necrotic bowel and surgery for complications |
|
|
Role of human milk in extremely low birth weight infants' risk of necrotizing enterocolitis or death
J Perinatol 2009; 29(1):57-62 |
A reduction in the risk of necrotizing enterocolitis or death among extremely low birth weight infants was associated with human milk feeding. A possible dose-dependant beneficial effect of HM is suggestive in extremely low birth weight infants.
|
|
|
Intraventricular Hemorrhage
|
Intracranial hemorrhage originating in the periventricular subependymal germinal matrix
Risk Factors - extreme prematurity - need for vigorous resuscitation at birth - pneumothorax - ventilated preterm infants - sudden increase in arterial blood pressure with volume expansion - hypotensive event - hypertension - RDS - fluctuating cerebral bllod flow - coagulopathy Clinical Presentation - many infants with IVH are asymptomatic - subtle signs : apnea, bradycardia, changes in tone or activity, altered level of consciousness - catastrophic presentation : bulging fontanelle, drop in hematocrit, acidosis, seizures, hypotension Screening Routine head ultrasound screening of all preterm infants <32 weeks gestation throughout NICU stay |
|
|
Management of interventricular hemorrhage and prognosis
|
Management of Acute Hemorrhage
- supportive care to maintain blood volume and acid-base status - avoid fluctuations in blood pressure and cerebral blood flow - follow-up with serial imaging Prognosis - outcome depends on grade of IVH - short-term outcomes for severe IVH : mortality, posthemorragic hydrocephalus or infarction - possible long-term major neurological sequelae - prognosis depends on hemorrhage severity - premature babies are also at risk of PVL (periventricular leukomalacia) |
|
|
Acrocyanosis
|
Transient mottling when exposed to cold; usually normal, particularly if premature
|
|
|
Vernix caseosa
|
Soft creamy white layer covering baby at birth
|
|
|
Slate-grey nevus of childhood
"Mongolia spots" |
Bluish grey macules over lower back and buttocks (may look like bruises); common in dark skinned infants
|
|
|
Capillary hemangioma
|
Raised red lesion, which increases in size after birth and involutes; 50% resolved by 5 years, 90% by 9 years
|
|
|
Erythema toxicum
|
Erythematous vesiculo-pustular rash, lesions disappear and reappear in minutes to hours, resolves by 2 weeks
|
|
|
Milia
|
Lesions 1-2 mm firm white pearly papules on nasal bridge, cheeks and palate; self resolving
|
|
|
Pustular melanosis
|
Brown macular base with dry vesicles, seen more commonly in african american infants
|
|
|
Angiomatous lesions (Salmon patch)
|
Transitory macular capillary hemangiomas of the eyelids and neck (Angel kiss)
Usually disappears with age |
|
|
Assessment of severity of dehydration in children
|
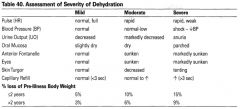
|
|
|
Common presentation of renal disease (reading)
|
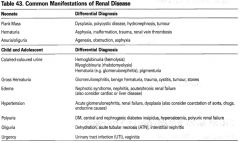
|
|
|
Assessment of severity of dehydration
|
Capillary refill
Blood pressure Anterior fontanelle Skin turgor Eyes sunken Heart rate Oral mucosa Output of urine |
|
|
Principles of treatment of rehydration
|
- Provision of maintenance daily fluid and electrolyte requirements
- Plus replacement of deficit fluids and electrolytes - Plus replacement of ongoing losses |

