![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
What are the 4 classifications of muscle dz?
|
- neurogenic
- NMJ - primary muscle dz - myopathies associated with systemic dz |
|
|
With an ATPase pH 9.8 stain, do Type I fibers stain light or dark? Type II?
|
light
dark |
|
|
In myopathic injury, what is seen re: light microscopy examination of fibers?
Neurogenic? |
random pattern of atrophic & hypertrophic fibers, both fiber types
group atrophy of type 1 and type 2. |
|
|
Selective type 2 atrophy of muscle fibers on light microscopy is evident of what?
Selective Type 1 atrophy? |
non-specific finding (disuse, corticosteroid therapy, polymyalgia rheumatica)
congenital myopathies and myotonic dystrophy. |
|
|
Endoymsial fibrosis is most commonly seen when the muscular degeneration is due to which etiology?
|
myopathies; prominent feature of DMD and Becker
|
|
|
The following characteristics are more associated with which etiology of pathologic muscle dz:
- Necrosis w/ myophagocytosis - regeneration - random variation in fiber size - increased central nuclei - endomysial fibrosis - fatty infiltration - fiber splitting - vacuolar changes - inclusions and accumulations |
myopathic
|
|
|
The following characteristics are more associated with which etiology of pathologic muscle dz:
- Atrophic, angulated fibers - Fiber type grouping - Group atrophy of both fiber types - Target fibers |
Neurogenic
|
|
|
What are some general categories (5) of myopathies?
|
dystrophies, inflammatory myopathies, metabolic caused myopathies, congenital myopathies, toxic and drug induced
|
|
|
Lambert-Eaton myasthenic syndrome affects which part of the muscular/nerve system?
How about myasthenia gravis? |
NMJ
NMJ |
|
|
What are some examples of neurogenic causes of muscle dz?
|
Dz of motor neurons
- spinal muscular atrophy - amyotrophic lateral sclerosis - charcot-marie-tooth dz dz of peripheral nerves/nerve roots dz of NMJ - myasthenia gravis - Lambert-Eaton myasthenic syndrome |
|
|
Which dz is characterized by an absence of dystrophin membrane protein due to an X-linked mutation in the gene for dystrophin?
|
DMD
|
|
|
What is the most common, most severe muscular dystrophy?
|
DMD, only affects males b/c X-linked.
|
|
|
21 month old boy presents with parents complaining of waddling gait, difficulty climbing stairs, and difficulty rising from the floor. Parents report that the child did not begin walking until ~18 months of age.
On PE, pseudohypertrophy of calf muscles is noted, as well as weakness/wasting of the proximal limb-girdle muscles that is worse in the lower limbs than the upper limbs. What is your dx? |
DMD
|
|
|
What is Gower's sign?
|
this weird way pts with DMD get off the ground due to muscle weakness..... almost looks like they're someone who is just 100% exhausted.
|
|
|
What is the prognosis for DMD?
|
wheelchair bound by age 12, intellectual impairment
--> profound muscle weakness, respiratory, and cardiac issues ... death in mid teens to late twenties. |
|
|
What is Becker Muscular Dystrophy?
|
milder form of DMD with later onset.
|
|
|
What are two inflammatory myopathies characterized by symmertrical, proximal muscle weakness which is often painful?
Are they more common in M or F? EMG change? |
Polymyositis/Dermatomyositis
2:1 male myopathic EMG changes |
|
|
Characterize Polymyositis.
In which age group is it prevalent? tx? |
30-60% of inflammatory myopathies
Autoimmune mediated disease secondary to defective cellular immunity Adults, age 40-60 Tx: steroids |
|
|
Characterize Dermatomyositis.
In which age group is it prevalent? -other associations? tx? |
Antibody mediated injury to microvasculature
Adults and children Characteristic skin rash Gottron lesions Association with malignancy Tx: steroids |
|
|
Which inflammatory myopathy is characterized by Gottron's papules and telangiectasias?
|
Dermatomyositis
|
|
|
Which inflammatory myopathy is characterized by lymphocytes invading a myofiber... what is essentially endomysial chronic inflammation?
|
Polymyositis
|
|
|
Which inflammatory myopathy is characterized by perifascicular atrophy, and perivascular inflammation (mixed B- and T-cell )?
|
Dermatomyositis
|
|
|
A deletion in Survival Moton Neuron (SMN) gene on crsm5 leads to which dz?
|
Spinal Muscular Atrophy (Werdnig-Hoffman dz)
|
|
|
Baby is brought into the clinic with parents complaining that child cannot control it's head, and cannot sit upright. On exam, there is marked hypotonia "floppy baby", proximal>distal weakness; however, facial muscles are spared. CK is normal, but denervation changes are seen on EMG.
dx? etiology? prog? finding on LM? |
Spinal Muscular atrophy (Werdnig-Hoffman dz)
Due to a degeneration/loss of anterior horn cells in the spinal cord Deletion in the Survival Motor Neuron gene (SMN) on chromosome 5 Respiratory problems leading to pneumonia & death before age 2 - Large groups of atrophic, round fibers - fascicular atrophy - fiber type grouping - Hypertrophy of type 1 fibers - increased connective tissue |
|
|
Re: PNS neurons, what causes "onion bulbs" of schwann cells?
|
recurring episodes of demyelination.
|
|
|
What is the most common hereditary neuropathy?
Acquired neuropathy in USA? World? |
Charcot-Marie-Tooth (CMT) dz.
Diabetic neuropathy Leprosy |
|
|
What is the most common subtype of peripheral neuropathy?
|
axonal (so named b/c axonal degeneration predominates in these dz) - dying back-type.
--> "distal axonal neuropathy" |
|
|
How can nerve conduction velocity (electrophysiological studies) help to differentiate b/t axonal type and demyelination type?
|
axonal = velocity near normal
demyelination type = velocity significantly decreased |
|
|
What are some clinical features of peripheral neuropathy?
Can these dz be selective for the types of fibers they affect (large myelinated vs small myelinated and unmyelinated)? |
muscle weakness, muscle atrophy, sensory loss, paresthesia, pain, and autonomic dysfunction
Yes (this would be PPTP vs PT, in the order given) |
|
|
Polyneuropathies often show what type of pattern, clinically?
|
glove and stocking
"length-dependent neuropathy" |
|
|
Name some causes of axonal neuropathy.
|
diabetes mellitus
alcoholism and nutritional uremia drugs/toxins amyloidosis systemic vasculitis paraneoplastic syndx infections idiopathic. |
|
|
What is the most common form (type of manifestation) of diabetic neuropathy?
- subtype? |
distal, predominantly sensory polyneuropathy.
- can also be autonomic, sensorimotor, mononeuroplathic, etc. though - distal axonal degeneration predominantes, but demyelination is present as well. |
|
|
How does alcoholic, uremic, and most drug related neuropathies present?
- subtype? |
distal sensorimotor polyneuropathy.
- distal axonal degeneration |
|
|
What is the definitive tx for uremic neuropathy?
|
dialysis/renal txplt
|
|
|
What typically causes vasculitis neuropathy in systemic vasculitis like with Churg-Strauss, Wegener's, polyarteritis nodosa, & microscopic polyangiitis? Is this also true of connective tissue dz (RA, SLE) and HIV infections?
|
nerve ischemia --> axonal neuropathy.
Yes, these dz can cause vasculitic neuropathy. |
|
|
Amyloid neuropathy can be a complication of which of the following?
- light-chain AL found with primary systemic amyloidosis - light chain AL found in MM - secondary amyloidosis (AA) How does this neuropathy often present (subtype)? |
both AL's.
small-fiber neuropathy |
|
|
What are the sorts (3) of immune-mediated demyelinateing neuropathies?
|
- acute inflammatory demyleinating polyradiculoneuropathy (AIDP)
- CIDP - anti-MAG IgM paraproteinemic demyelinating neuropathy |
|
|
What are 3 hereditary demyelinating neuropathies?
|
- CMT1 subtype of CMT dz
- hereditary neuropathy w/ liability to pressure palsies (HNPP) - Dejerine-Sottas syndrome |
|
|
What is the most common cause of Fuillain-Barre syndrome?
Pathogenesis? Pathologic/Clincal features? What does lumbar puncture typically show in Guillain-Barre syndx? |
AIDP
- often follows bacterial, viral, or mycoplasmal infections - PNS shows multifocal areas of demyelination, remyelination, onion bulbs, and some axonal loss. Demyelination is often accentuated in more proximal nerves and roots increase protein and *no* pleocytosis. |
|
|
Differentiate AIDP and CIDP.
Histological/clinical fx? |
Unlike AIDP, an antecedent upper respiratory or gastrointestinal infection is usually not reported in CIDP.
CIDP may occur sporadically or be associated with paraproteinemia, HIV infection, chronic active hepatitis, connective tissue disease, inflammatory bowel disease, or Hodgkin lymphoma. The nerves and roots show a chronic demyelinating neuropathy accompanied by chronic inflammatory infiltrates. The nerves may show numerous onion bulbs, owing to the recurring episodes of demyelination. |
|
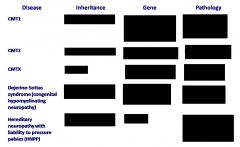
Fill in the chart, with special emphasis on CMT1, Dejerine Sotta, and HNPP.
|

|
|
|
72-yo man complains to his physicain of a 6m hx of progressive fatigue and leg cramps. he has also noticed twitching of the muscles on his chest (fasciculations) and difficulty lifting his left foot when he walks (foot drop). HE reports that on a few occasions he choked on food while swallowing. Cognitive fx appears normal, and the pt denies difficulty w/ bowel or bladder fx. PE shows bilateral diffuse muscle wasting in both upper and lower extremitites w/ prominent fasciculations in all muscle groups. Muscle tone is increased, and tendon reflexes are hyperreactive in all four extremities. Pt shows a positive Babinski's sign but sensory exam and coordination are normal. EMG shows denervation and fasciculations. What is the dx?
Characterize the general features of this dz. |
ALS
UMN & LMN sx eye & sphincter usually spared, as are sensory sx. There is typically no dementia or cerebellar or extrapyramidal dysfunction. |
|
|
Can the familial form of ALS be distinguished from the sporadic variant?
- is the familial form dom or recs? |
no.
- autosomal dominant. |
|
|
What gross anatomic changes are seen in ALS?
microscopic? |
degeneration or corticospinal or UMN and observable alterations of lateral pyramidal pathways of the spinal cord. Ventral roots atrophy secondary to loss of anterior horn LMNs. affected muscles are shrunken and pale.
loss of large motor neurons in the anterior horn of the spinal cord as well as the hypoglossal nucleus. This is accompanied by mild gliosis. - neurofilaments aggregate in axons --> spheroids |
|
|
What might be causing the pathology of ALS? Thus, what might be helpful as a tx?
**not that important** |
muscles *might* be getting damaged by glutamate.
- riluzole (inhib glutamate release) - mementine |
|
|
Describe the pathogenesis of myasthenia gravis.
What is often an effective tx? |
immunologic attack on the Ach receptor of the motor endplate. Antibodies attach to various receptor protein epitopes, thereby reducing the number of receptors.
thymectomy, in those pts with thymoma or hyperplasia of thymus. corticosteroids, methotrexate, and anti AChesterase. Plasmapheresis can also help in the short-term to \plasma antibodies. |
|
|
What are common clinical sx of myasthenia gravis?
|
- sx wax and wane
- weakness of extraocular muscles is typically severe and causes ptosis and siplopia. |
|
|
What is lambert-eaton syndrome?
What cancer is it often associated with? Pathogenesis? Tx? |
paraneoplastic disorder that manifests as muscular weakness, wasting, and fatigability of proximal limbs and trunk. Also termed myasthenic–myopathic syndrome
Small cell lung carcinoma evidence for a defect in ACh release @ nerve terminals. This dz can be transferred to mice by IgG from human pts. These pathogenic IgG target voltage sensitive Ca++ channels necessary for the release of ACh. responds to corticosteroids. |

