![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
15 Cards in this Set
- Front
- Back
|
What is the main diagnostic criteria for MI? |
Rise/fall troponins T/I with at least one value above 99th percentile upper reference limit + at least one: • Symptoms of ischemia • ECG changes • Imaging evidence of new loss of viable myocardium or new regional wall formation |
|
|
What is the difference between a STEMI and a non-STEMI, other than ECG change? |
Non-STEMI: sub occlusive thrombus of major vessel/ full occlusion minor vessel, only thrombolytics given, worse post-admission mortality, no Q, STREPTOKINASE NOT GIVEN
STEMI: full occlusive thrombus of major vessel, PCI given, SK given, transmural ischemia, Q waves |
|
|
Give 3 signs and 3 symptoms of acute MI. |
Signs: tachycardia, S4, low grade fever. Symptoms: chest pain (Levine’s sign), dyspnea, diaphoresis, palpitations, syncope, weakness. |
|
|
What would the investigatory blood sample of someone with acute MI show? |
Troponin T & I leak, leukocytosis, raised ESR CRP, AST, myoglobin, LDH, CK MB |
|
|
Name 3 complications of acute MI. |
3rd degree AV block, VSD, papillary muscle rupture + chordate tendinae rupture -> MR. (HF, ventricular aneurysm) |
|
|
Name 4 routes of thrombolysis taken to treat MI. Give their modes of action |
Aspirin (COX1 &2 inhibition prevents precursors TXA2 being synth i.e. prevents arachidonic acid ->PGG/PGH. TXA2 normally stimulates activation new platelets and mediates expression GP IIb/IIIa which binds fibrinogen )/clopidogrel (acts on ADP receptor of pt cell membranes, tirofiban does the same)
tPA infusion e.g. alteplase/reteplase/ bolus tenectaplase (serine protease catalyses plasminogen to plasmin)
LMWH/Fondaparinux heparin binds antithrombin III increasing its efficacy 1000fold, inactivating thrombin, Fonda = FXa inhibitor
Streptokinase fibrinolytic binds to plasminogen to activate more plasminogen |
|
|
Name 3 other drugs given to treat acute MI. |
BB (decrease risk cardiac rupture & arrhythmia)/ aspirin/ ACE-I (prevents damaging remodelling, decreases LV dysfunction) |
|
|
Name a circumstance when you can give an implantable defib post AMI as both primary and secondary prevention. |
1° prevention • AMI >4 weeks previously • LV ejection fraction <30% and QRS >120msec • LV ejection fraction <35% and non-sustainedVT on Holter 2° prevention • Late cardiac arrest VT/VF • Sustained VT with syncope • Sustained VT and LV ejection fraction <35% |
|
|
What are pathological Q waves? |
Small q waves normal in most leads, deeper is normal in III & aVR. Pathological if >1mm wide, >2mm deep, >25% QRS, leads V1-3. Normally seen as a left to right depolarisation of interventricular septum. Pathological = full thickness death of myocardium, act as windows to see the other side of the heart where depolarisation away from electrode. |
|
|
What are risk factors for MI? |
Age, male, family history – MI in 1st degree relative <55. Smoking hypertension DM hyperlipidemia obesity sedentary lifestyle. |
|
|
What are symptoms of MI? |
Intense and unrelenting 30-60m squeezing burning aching pain, retrosternal pain up to neck shoulder jaw & ulnar aspect left arm, nausea, sweating, dyspnoea, palpitations, fever |
|
|
What are signs in MI? |
Distress, anxiety, increased HR, arryhthmia, inc BP, inc RR, lateral apex beat displacement, dyskinesis, palpable S4 because decreased LV contractility, could be HF signs |
|
|
What is the Ddx of MI? |
Angina, pericarditis, myocarditis, PE |
|
|
What is given prehospital in acute MI setting? |
Aspirin (inhibits COX, reduces synthesis of TXA2 and therefore pt aggregation), Metcloperamide(dop receptor antagonist, antiemetic), morphine (periph vasodilation, venous pooling, decrease preload) |
|
|
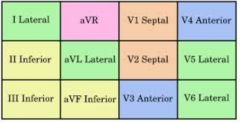
Which ECG leads are anterior, septal, inferior and lateral, thus when ST elevated, indicate region of ischemia? |
|

