![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
100 Cards in this Set
- Front
- Back
- 3rd side (hint)
village; rural area culley
|
农村
nóng cūn |
nóng cūn
|
|

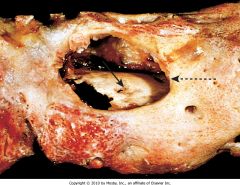
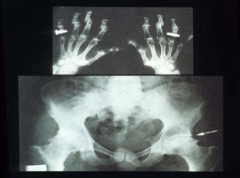
What is shown? Who is most commonly affected by this disease?
|
• Avascular Necrosis of bone
• Often due to fracture in elderly • In young boys (3-10 yo) its called Legg-Calve Perthes disease |
|
|
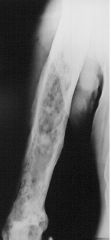
What disease is shown? Who is commonly affected? What complications are these patients at risk for?
|
Paget's disease of the bone
• Typically ♂ > 50 yo • At risk for high-output heart failure and osteosarcoma |
|
|
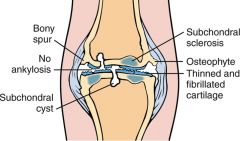
What disease process is shown? What are the distinguishing factors?
|
Osteoarthritis
• Most important feature is the degenerated cartilage |
|
|

What signs are pictured? At the DIP and at the PIP? What disease can this be seen in?
|
DIP: Heberden's nodes
PIP: Bouchard's nodes Seen in osteoarthritis |
|
|

What disease process is shown? What are the (3) characteristic signs seen?
|
Rheumatoid Arthritis
• Ulnar deviation • Boutonniere deformity • Swan neck deformity |
|
|

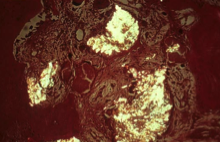
What disease process is shown? What is one of the key characteristics pictured?
|
Rheumatoid arthritis
• Pannus (granulation tissue that releases cytokines that destroy articular cartilage) formation |
|
|
|
• Autosomal dominant
• Pathology is due to defective synthesis of Type I collagen • Signs: Fractures at birth, blue sclera, deafness • Tx: Bisphosphonates (↑ bone mineralization) |
Osteogenesis imperfecta
|
|
|
|
What is the 1º defect in osteogenesis imperfecta? What is its inheritance?
|
• Defective synthesis of Type I collagen
• AD inheritance |
|
|
|
• AD
• Mutation in FGF-R gene (gene mutations ↑ with paternal age) • Impaired proliferation of cartilage at the growth plate |
Achondroplasia
|
|
|
|
Clinical findings of this disease include: normal sized head & vertebral column, shortened arms & legs, normal growth hormone & insulin growth factor-1 levels
|
Achondroplasia
|
|
|
|
The clinical findings seen in achondroplasia is due to what? Which is the result of what gene mutation?
|
• Impaired proliferation of cartilage at the growth plates
• Due to mutation of the FGF-R gene. |
|
|
|
AD or Autosomal recessive (severe)
• Deficiency of osteoclasts • Normal balance of osteoblasts making bone & clasts breaking down bone is disrupted favoring increased bone formation • Overgrowth and sclerosis of cortical bone "too much bone" |
Osteopetrosis
|
|
|
|
What is the 1º defect in osteopetrosis? What is the inheritance? What is the Tx?
|
• Balance of osteblasts & clasts is disrupted, favoring ↑ bone formation.
• Inheritance can be AD (less severe) or Recessive (severe) • Tx: bone marrow transplant |
|
|
|
What are the clinical findings of osteopetrosis?
|
•Pathological frax • Anemia (bone marrow is replaced) • Visual & hearing loss (cranial nerve compression) |
|
|
|
What is the most common site of infx in osteomyelitis of children?
What is the most common route of spread? |
• Tibia & Fibula
• In children: hematogenous spread |
|
|
|
What is the most common bug that causes osteomyelitis?
|
• Staph aureus
|
|
|
|
Osteomyelitis in the vertebral column after TB infxn is called?
|
• Potts disease
|
|
|
|
Is osteomyelitis: devitalized bone is called ______
• Reactive bone formation in the periosteum is called ______ • An area draining the infected area is called _____ |
• Sequestrum (devitalized bone)
• Involucrum (newly formed bone) • Sinus tract |
|
|
|
Treatment for osteomyelitis due to staphylococcus aureus (in neonates) is:
|
• 3rd generation cephalosporin (ceftazisime) & vancomycin parenterally for 2 weeks
• Continue on oral abx until CRP has normalized (usually ≥ 1 more week) |
|
|
|
Treatment for osteomyelitis in kids (must cover staphylococcus aureus and/or group A strep) is:
|
• Vacomycin (+ Nafcillin if in an area w/ < 10% MRSA) parenterally for 2 weeks
• Continue on oral abx until CRP has normalized (usually ≥ 1 more week) |
|
|
|
Most comon metabolic abnormality of bone. More common in ♀ than ♂.
• ↓ Bone mass & density. • Radiograph shows a washed out appearance. |
Osteoporosis
|
|
|
|
Osteoporosis can be caused by ___ in estrogen and ____ in cortisol/corticosteroid use.
|
↓ in Estrogen. ↑ in cortisol/corticosteroid use
|
|
|
|
What are the most common clinical findings associated with osteoporosis?
|
• Compression fractures of the vertebral bodies
• Colles fracture of the distal radius • Dowager's hump |
|
|
|
What is test is the best for the dx of osteoporosis?
|
• Dual photon absorptiometry (Bone density scan)
|
|
|
|
What is the treatment for osteoporosis?
|
• First line: Bisphosphonates
• Calcitonin inhibits osteoclasts • Calcium & vitamin D supplements |
|
|
|
A complication of an subcapsular fracture that disrupts the blood supply to the head of the femus is ___?
|
• Avascular necrosis
|
|
|
|
Aseptic necrosis of the femoral head
• Occurs in boys ages 3-10 years • Presents with pain in the knee or a limp |
Legg-Calve Perthes disease
|
|
|
|
Aseptic necrosis of the ossification centers in children
|
Osteochondrosis
|
|
|
|
• Affects physically active boys 11-15 yo.
• Painful swelling at the tibial tuberosity • Inflammation of the proximal tibial apophysis at insertion of the patella tendon |
Osgood-Schlatter's disease
|
|
|
|
• ♂ > 50 yo.
• Targets pelvis, skull (enlarged), femur • Early phase of osteoclastic resorption of bone • Late phase of ↑ osteoblastic bone formation |
Paget's disease of the bone
|
|
|
|
What disease is characterized by ↑ serum alkaline phosphatase (normal Ca++ and phosphorus)
• Production of thick, weak bone (mosaic bone) |
Paget's disease of the bone
|
|
|
|
Pts is a 50 yr old male. Complains of "bone pain" and noticed that he can't wear his hats (they are too small). What disease does he have?
|
Paget's disease of the bone
|
|
|
|
What are the risks associated with Paget's disease of the bone? What is the Tx?
|
• Pathological fractures
• ↑ risk for osteosarcomas • ↑ risk for high output heart failure (due to arteriovenous connections in vascular bone) • Bisphosphonates & Calcitonin |
|
|
|
Bone tumor: characterized as an outgrowth of bone (exostosis) capped by benign cartilage
• ♂ 10-30 yo (solitary or multiple) • Most comonly at the metaphysis of the distal femur • Most common benign tumor |
Osteochondroma
(Benign) |
|
|
|
Tumor characterized by being multiple or solitary
• Equal distribution ♂ = ♀ • Most often locaed in the medulla in the small tubular obnes in the hands & feet |
Enchondroma
(Benign) |
|
|
|
Bone tumor usually in the facial bones
• Usually middle-aged ♀ |
Osteoma (Hiserote)
(Benign) |
|
|
|
Tumor that appears on radiographs as having a radiolucent focus surrounded by sclerotic bone
• Nocturnal pain relived by aspirin • Usually found in the cortex of the proximal femur • 10-20 yo ♂ |
Osteoid osteoma
(Benign) |
|
|
|
Tumor usually locaed at the epiphysis of the distal femur or proximal tibia
• Histology shows reactive multinucleated giant cells that resemble osteoclasts (neoplastic mononuclear cells) • Usually in 20-40 yo ♀ |
Giant cell tumor
(Benign) |
|
|
|
Tumor that appears on radiographs as having a radiolucent focus surrounded by sclerotic bone
• Nocturnal pain relived by aspirin • Found in the *vertbrae* • 10-20 yo ♂ |
Osteoblastoma
(Benign) |
|
|
|
Malignant tumor that often metastasizes to the lungs
• Usually found in the pelvic bones/proximal femur • 30-60 yo ♂ |
Chondrosarcoma
|
|
|
|
• Malignant tumor: radiographic findings "sunburst appearance" (spiculated pattern from calcified malignant osteoid)
• Codman's triangle (tumor lifting the periosteum) • Often metasteses to the lung |
Osteogenic sarcoma
|
|
|
|
• Bimodal incidence peaks: 10-25 yo ♂ & those w/ h/o Paget's disease (usually ♂ > 50 yo)
|
Osteogenic sarcoma
|
|
|
|
This is the most common 1º bone tumor
• Most often located in the metaphysis of the distal femur or proximal tibia |
Osteogenic sarcoma
|
|
|
|
Risk factors for Osteogenic sarcoma are:
|
Paget's disease, familial retinoblastoma, irradiation, fibrous dysplasia
|
|
|
|
• Small round cell bone tumor
• Radiographs shows "onionskinning" appearance around bone (periosteal rxn) |
Ewing Sarcoma
|
|
|
|
• Malignant bone tumor
• Usually located in the pelvic girdle, diaphysis and metaphysis of the proximal femur or rib • 10-20 yo ♂ |
Ewing Sarcoma
|
|
|
|
Classification of synovial fluid: Non-inflammatory
Seen in: OA, neuropathic joint |
Group I
|
|
|
|
Classification of synovial fluid: Inflammatory
• Seen in RA, gout |
Group II
|
|
|
|
Classification of synovial fluid: Septic
• Seen in Lyme disease, disseminated gonoccocemia |
Group III
|
|
|
|
Classification of synovial fluid: Hemorrhagic
• Seen in Trauma, hemophilia A & B |
Group IV
|
|
|
|
• Non-inflammatory joint disease
• Occurs ♂ = ♀ •Usually > 65 yo • Most common sites: Femoral head, knee, cervical & lumbar vertebrae |
Osteoarthritis
|
|
|
|
What joint disease is characterized by progressive degeneration of the articular cartilage? What joints are most commonly affected?
|
Osteoarthritis
• Weight bearing joints: femoral head, knee, cervical & lumbar vertebrae |
|
|
|
What joint disease shows cytokines that activate metalloprotineases that cause degradation of proteoglycans and collagen in the joint?
|
Osteoarthritis
|
|
|
|
In osteoarthritis what can be seen at the joint margins? What are joint mice?
|
• Reactive bone formation can occur (osteophytes)
• Joint mice are fragments of articular cartilage that break free into the joint space |
|
|
|
What joint disease eventually leads to bone rubbing on bone (what is this term called) but NO ankylosis (fusion) of the joint? In severe cases there may be formation of ____ (fibrous synovial tissue) that covers the articular surface.
|
• Eburnation
• Osteoarthritis • Pannus |
|
|
|
What joint disease is characterized by pain, aggravated by activity, Herberden's nodes(enlargement of the ___ jonts), Bouchard's nodes (enlargement of the ___ jonts), and sometimes degenerative disk disease?
|
• Osteoarthritis
• Herberden's nodes (enlargement of the DIP joints) • Bouchard's nodes (enlargement of the PIP joints) |
|
|
|
This joint disease occurs most often in 30-50 yo ♀ and has an association with HLA-DR4
|
Rheumatoid Arthritis
|
|
|
|
The pathology of this disease is:
• B and T cells are activated leading to damage of synovial cells • Synovial cells express an antigen that triggers B cells to produce an auto-Ig • The IgM autoantibody that has specificity for the Fc portion of IgG. • The auto-antibody and IgG form immunocomplexes (type III hypersensitivity) • Immunocomplexes activate the complement system to produce C5a, a chemotactic agent for neutrophils and other leukocytes to enter the joint space. • Chronic synovitis and pannus formation eventually occur • Pannus (granulation tissue): releases cytokines that destroy articular cartilage • Repair by fibrosis causes fusion of the joint (ankylosis) |
Rheumatoid Arthritis
|
|
|
|
What is pannus?
|
Pannus is granulation tissue that is formed within the synovial tissue by fibroblasts and inflammatory cells. ALWAYS seen in RA often seen in late-stage OA
|
|
|
|
What joint disease shows the Swan neck deformity (which is?) and Boutonniere deformity?
|
Rheumatoid Arthritis
• Swan neck deformity: Flexion of the DIP joint & extension of the PIP joint |
|
|
|
How is Rheumatoid arthritis both a type III and type IV immune-mediated process?
|
Type IV: B & T-cells are activated leading to the damage of synovial cells
• Type III: Synovial cells express an antigen that triggers B-cells to produce rheumatoid factor (RF). RF is an IgM autoIg that has affinity for the Fc potion of the IgG --> IgG and RF join together to from immune complexes (Type III rxn) |
|
|
|
What disease causes ulnar devation of the hands and prominent swelling of the 2nd & 3rd metacarpophalangeal joitns?
|
Rheumatoid Arthritis
|
|
|
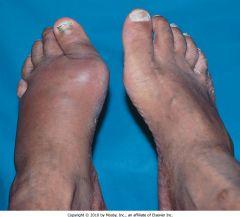
What disease is pictured? Specifically what is this called? What is it due to?
|
Gout
Podagra Due to the build up of monosodium urate crystals in the joint |
|
|

What disease is pictured? What specific condition is pictured? What is this caused by?
|
Gout
Tophi in the soft tissue in the joints of the hand Caused by the build up of monosodium urate crystals in the joints |
|
|

What is shown? What disease is this a feature of?
|
"Pencil in cup deformity"
Characteristic of psoriatic arthritis |
|
|
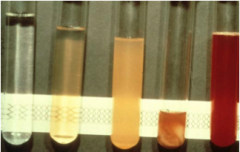
What is shown? Describe the tubes from L to R.
|
Synovial fluid tubes
From left to right #1 normal #2 noninflammatory (e.g., osteoarthritis) #3 inflammatory (e.g., rheumatoid arthritis) #4 septic (e.g., gonococcal septic arthritis), #5 hemorrhage (e.g., trauma, hemophilia A) |
|
|
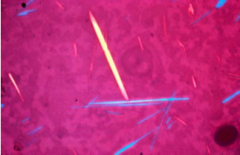
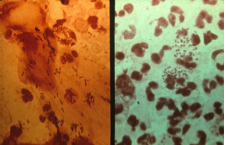
What is shown? In what disease does this occur?
|
Synovial fluid crystals w/ red filter in place
(1) Crystals are monoclinic (needle shaped) and could be either monosodium urate or calcium pyrophosphate, (2) if crystal is yellow when parallel to the slow ray of the compensator, it is monosodium urate and defines negative birefringence, (3) if crystal is blue when parallel to the slow ray of the compensator, it calcium pyrophosphate and defines positive birefringence |
|
|
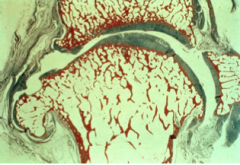
What disease is shown? What does the blue show? Red?
|
Blue stains cartilage and red bone, note how the articular cartilage is worn down and fibrillated in areas (perpendicular cracks), note the osteophyte at the margin of the joint
|
|
|
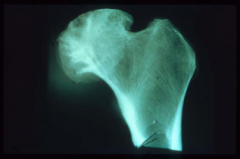
What disease process is shown?
|
Osteoarthritis
X-ray of head of femur removed at surgery, note the subchondral bone cysts beneath the surface |
|
|

What disease process is shown? What are the two types of nodes called?
|
Osteoarthritis:
Note the enlargement of the DIP (Heberden's nodes) and PIP joints (Bouchard's nodes), enlargements represent osteophytes |
|
|
What disease is shown? How is this apparent?
|
Osteoarthritis
Note x-ray of hands and OA in the DIP and PIP joints, note the narrow joint space in the femoral joint and sclerotic changes |
|
|
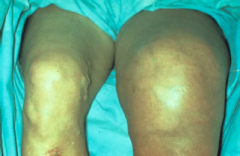
What is shown?
|
Charcot (neuropathic) joint
Note enlarged knee on your right (patient left knee) |
|
|

What disease is shown?
|
Rheumatoid arthritis (RA) note the enlarged MCP joints
|
|
|

What disease is shown? What are the distinguishing characteristics?
|
RA
Note symmetrical involvement in both hands with enlarged MCP joints and ulnar deviation |
|
|

What deformity is shown? What disease is this seen in?
|
• Boutonniere deformity of digit - note extension of DIP joint and flexion of PIP joint
• RA |
|
|

What deformity is shown? What disease is this seen in?
|
• Swan-neck deformity of digit - note flexion of DIP joint and extension of PIP joint
• RA |
|
|

What is shown? Seen in what disease?
|
• Rheumatoid nodules on extensor surface of forearm, example of fibrinoid necrosis (same lesions seen in acute rheumatic fever)
• RA |
|
|

What is shown? In what disease?
|
• Podagra: note inflamed first metatarsophalangeal joint (big toe)
• Gout |
|
|

What disease is pictured?
|
• Gout
• Note large tophus on malleolus and along margin of the foot, sign of chronic gout, composed of crystalline material (H and E shows multinucleated giant cell reaction to the MSU crystals) |
|
|
What is shown? Characteristic of what disease?
|
• Polarization of tophus showing MonoSodium Urate crystals
• Gout |
|
|
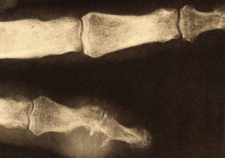
What disease is shown?
|
• Gout
• X-ray of digit showing erosive joint disease in bottom digit |
|
|

What sero-negative spondyloarthropathy could be shown here?
|
• Reiter's syndrome
• Patient with non-infectious conjunctivitis, previously had Chlamydia trachomatis infection and then developed conjunctivitis and arthritis (HLA B27 positive) |
|
|

What sero-negative spondyloarthropathy is shown? What are the common features?
|
• Psoriatic arthritis
• Note disabling arthritis of the hands • Nail pitting is commonly present (not present in photo) |
|
|

What seronegative spondyloarthropathy is shown?
|
Septic arthritis due to disseminated gonococcemia Note the hot knee and the pustule on the wrist
|
|
|
What sero-negative spondyloarthropathy is shown?
|
• Septic arthritis
• Note the gram negative diplococci in the neutrophil |
|
|

What disease is shown? What is notable in the top image? The bottom?
|
Scleroderma
• Tight facial features & telangiectasias on the skin • Raynaud's phenomenon |
|
|

What is disease? What is notable around the eye? The hand? What diagnostic test can be done?
|
Dermatomyositis
• Heliotrope (purplish discoloration around the eyes) pathgnomonic • Gottron's patches are noted over the PIP joints and the • Diagnostic test: muscle biopsy shows a lymphocytic infiltrate, CK levels are always increased |
|
|
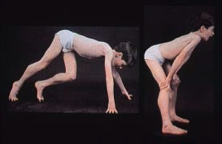
What disease is pictured? What maneuver? What protein is defective?
|
• Duchenne's muscular dystrophy
• Gower's maneuver (the child is pushing himself up from the down position) • SXR disease with deficiency of dystrophin • Note the pseudohypertrophy of the calf muscles |
|
|
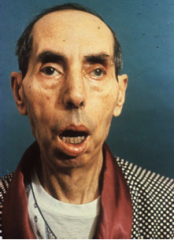
What disease is pictured? What is its inheritance? What else is notable about its inheritance?
|
• Myotonic dystrophy
• AD disorder • Triplet repeat (problem with anticipation - disease gets worse in future generations) • Note balding head and sagging face, patient's cannot relax their grip on something, cardiac disease/cataracts/ testicular atrophy are also present |
|
|
|
Describe type I muscle fibers
|
• Slow twitch (red) fibers
• Slow contraction but repetitive • Do not fatigue easily • Example: paraspinal muscles • Rich in mitochondira, myoglobin, oxidative enzymes • Weak in ATPase enzymes. mne: One slow fat red ox |
|
|
|
Describe type II muscle fibers
|
• Fast twitch white fibers
• Fast contraction but fatigue easily • Specialized for fine skilled movement • Poor in mitochondria, myoglobin, oxidative enzymes • Rich in ATPase enzymes Ex: Extraocular muscles, muscles in the hand mne: Two skinny white fast breasts |
|
|
|
What determines fiber type of a muscle?
|
Innervation
|
|
|
|
What muscle disorder is X-linked recessive and is the result of an absence of dystrophin?
|
• Duchenne's muscular dystrophy
|
|
|
|
What disease is characterized by:
• Symptoms appearing at 2-5 yo • Due to progressive degeneration of type I and type II fibers • Infiltration of muscle tissue by fatty tissue |
• Duchenne's muscular dystrophy
|
|
|
|
When do symptoms appear in Duchenne's muscular dystrophy? What muscles are affected? What are two key signs?
|
• Symptoms appear 2-5 yo (usually boys)
• Weakness & wasting of pelvic muscles • Gower's maneuver (child using hands on knees to stand) & pseudohypertrophy of calf muscles |
|
|
|
What are the lab findings in Duchenne's muscular dystrophy? What test is used to make the diagnosis?
|
• ↑ Serum CK at birth
• Serum CK progressively declines as muscle degenerates • ♀ carriers have ↑ levels of CK • Muscle biopsy is used to make diagnosis |
|
|
|
What muscle disorder is AD and is the result of sever atrophy of Type I fibers?
|
• Myotonic dystrophy
|
|
|
|
Myotonic dystrophy is the result of atrophy of type I fibers. This is due to what genetic disorders? What is unique about its inheritance?
|
• AD trinucleotide repeat (CTG) on long arm of chromosome 19
• Disorder shows anticipation |
|
|
|
What are some clinical features of Myotonic dystrophy?? What is the disease a result of?
|
• Facial muscle weakness (sagging face)
• Percussion and grip myotonia (unable to relax muscles after a sustained grip) • Frontal balding • Testicular atrophy • Cardiac involvement (conduction defects) |
|

