![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
Osteoblast |
Bone forming cell. |
|
|
Osteocyte |
Mature bone cell surrounded by bone matrix. |
|
|
Osteoclast |
Large, multinucleated cell that breaks down bone. |
|
|
Callus |
A mass of connective tissue that connects to the ends of a broken bone. |
|
|
Anatomical Position |
Position acquired when one stands erect with feet facing forward, upper limbs hanging at sides, and palms facing forward with thumbs to outside. |
|
|
2 principal agents in bone matrix and how they affect properties of bone tissue. |
(A) Hydroxyapatite and (B) Collagen. (A) Gives bones hardness and compressive strength. (B) Gives bones some flexibility and tensile strength. |
|
|
Bone cell that is completely surrounded by bone matrix. |
Osteocyte ("mature bone cell"). |
|
|
Bone cell that has more than one nucleus. |
Osteoclast. |
|
|
If you are looking at bone tissue through a microscope and see no osteons, is it compact or cancellous bone? |
Cancellous. |
|
|
(A) Kind of bone tissue that contains trabeculae. (B) Often found in spaces between trabeculae. |
(A) Cancellous. (B) Red bone marrow. |
|
|
(A) Term for layers of bone tissue that form an osteon. (B) Term of layers of bone between osteons. |
(A) Concentric Lamallae. (B) Interstitial Lamallae. |
|
|
Canaliculi |
Microscopic passageways in bone through which extensions of osteocytes run. |
|
|
6 reasons bone must be continually remodeled. |
1) Cancellous bone tissue often needs to be remodeled into compact bone tissue. 2) Bones increase and decrease in mass based on the stress they experience. 3) Bone is remodeled in order to re-shape bone as needed. 4) Bone is remodeled to repair broken bones. 5) Bone is remodeled to replace worn collagen/hydroxyapatite. 6) Bone is remodeled to regulate calcium levels in the body. |
|
|
Why doesn't the epiphyseal plate get thicker as the bone grows? |
Cartilage is ossified at the same rate at which it is added. |
|
|
On which side of the epiphyseal plate does tissue ossify? |
Diaphysis end. |
|
|
If long bone's epiphyseal plates have become epiphyseal lines, is there anyway that a bone can grow? |
Yes, but only in width. |
|
|
Appositional bone growth. |
When osteoblasts lay a new bone matrix on the surface of a bone. |
|
|
Order process that occur when bone is repaired according to sequence in which they occur: A) External callus is removed by osteoclasts, and cancellous bone is remodeled if needed. B) Hematoma forms. C) Callus is ossified. D) Callus forms. |
B, D, C, A. |
|
|
(A) Purpose of external callus. (B) Purpose of internal callus. |
(A) To stabilize bone while it is being healed. (B) Ossifies to become new bone tissue. |
|
|
(A) Gland that secretes calcitonin. (B) Gland that secretes PTH. |
(A) Thyroid Gland. (B) Parathyroid Gland. |
|
|
Effects of (A) Calcitonin and (B) PTH on the bone cells. |
(A) Decreases activity of osteoclasts. (B) Stimulates more activity by osteoclasts. |
|
|
What does a large increase in Calcitonin levels of the body tell you about the calcium level in a person's body? |
The blood calcium level is too high. |
|
|
Gland that secretes Growth Hormones and it's effect on bone tissue. |
Anterior Pituitary Gland; Stimulates tissue growth by increasing osteoblast activity. |
|
|
Effect sex hormones have on bone growth. |
Stimulates osteoblast activity, causing rapid bone growth; Causes epiphyseal plates in long bones to ossify, stopping growth ( at least in length of long bones). |
|
|
3 major types of joints in body and the type associated most with movement. |
Fibrous, Cartilaginous, and Synovial. Synovial. |
|
|
Purpose of articular cartilage in a Synovial Joint. |
Cushions ends of bones with "hard plastic" finish. |
|
|
Purpose of Synovial Fluid in a Synovial Joint. |
Lubricates joint; Supports chrondocytes in articular cartilage; Shock absorber. |
|
|
What produces Synovial Fluid? |
Synovial Membrane. |
|
|
6 Major types of Synovial Joints in order of DECREASING range of motion (assume pivot joints offer more mmotio than hinge). |
Ball-and-Joint, Saddle, Ellipsoid, Pivot, Hinge, Gliding (Plane). |
|
|
Motion exhibited on following: A) Standing on tiptoe. B) Straightening arms at elbow. C) Twirling lower limb in air in circle. D) Turning hands so palms point down. E) Lifting arms from sided to horizontal to ground. |
A) Plantarflexion. B) Extension. C) Circumduction. D) Pronation. E) Adduction. |
|
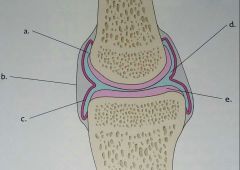
Synovial Joint. |
A) Bursa B) Fibrous Capsule C) Synovial Membrane D) Joint Cavity filled with Synovial Fluid E) Articular Cartilage. |
|
|
Hematoma |
Mass of blood that confines a limited space. |

