![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
12 Cards in this Set
- Front
- Back
|
Caries - factors |
1) Key Oral Microorganisms |
|
|
What evidence is there that caries is an infectious disease? |
1) Gnotobiotic animal studies (Sterile animals, causative relationship) 2) Human epidemiology studies - Cross-sectional (Correlation) - Longitudinal (Causation) |
|
|
Microorganisms that cause caries |
Streptococcus mutans: Gram +ve cocci, causative + associative, form adhesins S. Sobrinus Lactobacillus: Gram +ve rod, implicated in advanced caries Bifidobacterium: Gram +ve rod, implicated |
|
|
Challenges faced when finding out microbial aetiology of caries |
1) Disease occurs at sites with natural, diverse microbiota 2) Pathogen found in healthy sites in small numbers 3) Difficult to correlate microbiota to enamel status 4) Lesions can remineralise 5) Pathogenic traits non specific (can't differentiate) 6) Multifactorial nature of caries |
|
|
What role do other microorganisms apart from S.mutans play? (See next flashcard for A.Naeslundii) |
S.Mitis + S.Oralis: Acidogenic Veillonella Spp. Gram -ve, anaerobic, uses lactic acid -> proprionate/acetate Salivarius: Urea + H20 -> Ammonia + CO2 |
|
|
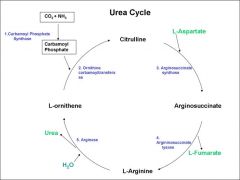
A.Naeslundii converts arginine to ammonia: what are the steps for the urea cycle |
|
|
|
Timeline of microorganisms |
Nursing bottle caries: Mutans streptococci + Lactobacilli Root Surface Caries: Early studies: Actinomyces SPP. Later studies: Mutans Streptococci + Lactobacillus Recent studies: Actinomyces Spp., Mutans Streptococci, gram -'ve rods, Actinomyces israelli |
|
|
Diet of bacteria |
In health: Bacteria live off glycoproteins - long time to break down + easily buffered In caries: Fermentable sugars, frequent exposure to biofilm, rapidly metabolised, slow buffering |
|
|
Characteristics of cariogenic bacteria |
Rapid sugar transport + acid production Acidurity (acid tolerance) EPS - Sticky polymers (adhesins) IPS - Storing excess sugar as glycogen The main characteristics of cariogenic bacteria are rapid sugar transport, high acid production and high acid tolerance. |
|
|
Hypotheses relating plaque to caries |
1) Specific plaque hypothesis Specific microorganisms in the plaque lead to caries 2) Non-Specific plaque hypothesis All bacteria do different things which have a net effect 3) Ecological plaque hypothesis (lecturer prefers this) Balance between bacteria + sugar, aetiology of plaque doesn't not monospecific. Environmental regulation of gene expression |
|
|
Disease is preventable/controllable by: |
1) Direct inhibition of the organisms that cause disease 2) Maintenance of a natural balance of microorganisms with non out-competing each other 3) Interference with factors causing damaging shifts in microbiota (fermentable sugars = <acid, ecology of microorganisms changed -> caries. |
|
|
How can you control dental caries |
1) Plaque control brushing, flossing, dentists 2) Fluoride To form fluoroapatite, helps remineralise, acidify cell interior, inhibit IPS synthesis, reduces glycolysis 3) Sugar substitutes Bulking agents: xylitol, sorbitol, intense sweeteners Saccharin 4) Antimicrobial/antiplaque agents: Toothpastes + mouthwashes, chlorhexidine, 5) Replacement therapy: Dairy strains: exclude cariogenic bacteria, S.Salivarius: bacteriocin producing strains, GM S.Mutans: Don't produce acid, exclude other S.mutans 6) Vaccinations: SlgA, IgA, neutrophils. Vaccines (untested on humans) 7) Passive immunisation: Coating surfaces with antibodies, reduces MS colonisation, safe + acceptable, non-invasive procedure. |

