![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
Truly acid fast vs partial
|
Acid fast organisms retain their stain & resist decolorization with HCl
Partially acid fast (nocardia) resist decolorization by H2SO4 but lose it after HCl |
|
|
Why is it bad to spit in public
|
mycobacteria! have lots of lipid in their cell walls and can live forever in spit
and it's gross |
|

media?
|
Lowenstein-Jensen agar
for mycobacteria |
|

|
Tb
"Buff-colored and heaped" |
|
|
What is MOTT
|
Mycobacteria other than TB
(used to be called atypical mycobacteria) |
|
|
How do we classify mycobacteria
|
Runyon system
4 groups based on pigment in light, dark, and growth rate (not TB) |
|
|
Runyon system
|
I: Photochromogens. turn yellow after light exposure.
II: Scotochromogens. Always yellow. III: Non-photochromogens. Always beige. IV: Rapid growers: Grow within 7 days |
|
|
Examples in each Runyon class?
|
I: Photochromogens: M kansasii, M. marinarum, M. simiae, M szulgai
II: Scotochromogen: M. gordonae, M. scrofulaceum III: Non-photo: MAI, M. haemophilum IV: M. fortuitum, M. abscessus, M. chelonei |
|

Which mycobacteria is scotochromogen (always yellow) at 37C but photochromogen (yellow only after light) at 25C?
|
M. szulgai
|
|
|
T/F: Some strains of MAI can be pigmented.
T/F: M. kansasii can be I, II, or III. |
True, most often in AIDS patients.
(MAI is normally considered a Runyon III NON-PIGMENTED) True. though it is usually I. |
|
|
Proper specimen type for sputum or urine for mycobacteria?
|
3-5 early morning specimens
|
|
|
What is the problem with gastric samples for mycobacteria?
|
Acidic. Must neutralize the pH in the lab.
fyi these samples are mostly in kids |
|
|
Steps of specimen processing in mycobacteria
|
1. Decontamination (must kill contaminating bacteria, by raising pH to 8.6)
2. Buffer (Return to pH 7) 3. Centrifugation 4. Slide prep 5. Agar choice |
|
|
How are specimens decontaminated? What is different in CF patients?
|
15 minutes only:
NaOH: raises the pH + NACL (n-acetylcystein) breaks up the mucus in CF: oxalic acid is used due to pseudomonas |
|
|
What speed do you centrifuge mycobacteria to make the pellet?
|
3000 x
|
|
|
2 main agar types for mycobacteria?
|
Lowenstein-Jensen (green) egg based
STERILIZE BY INSPISIDATION Middlebrook agar: clear, synthetic, can do susceptibilities |
|
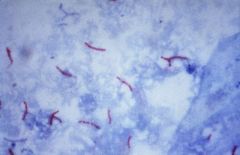
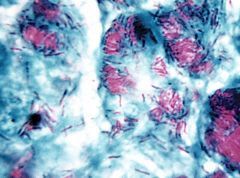
What 2 stains could this be?
|
Zeehl-Nielsen (old method - used heat)
Kinyoun: cold stain, uses phenol to drive stain into AFB. Both stain RED |
|
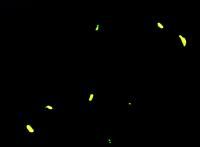
What stain is this?
|
Auramine rhodamine stain. Fluorescent. stains orange-y.
|
|
|
T/F: PCR amplification of mycobacteria can be used for both diganosis of disease and monitoring treatment effect.
|
False. Used for diagnosis. NOT for treatment - dead DNA can hang around and a patient can be cured but have a + PCR for up to 6 months
|
|
|
What temperature do we incubate mycobacteria?
Bacteria? Fungi? |
37C
bacteria @ 35 fungi at 30, or 25 (room temp) |
|
|
How long do we have to keep mycobacteria cultures?
|
6-8 weeks
|
|
|
What are the classic tests to ID TB?
|
Niacin accumulation + (must be taken from LJ agar! due to eggs)
Nitrate reduction + |
|
|
How to ID M Tb vs M bovis?
|
TCH (T2H) growth seen in M tb but not M bovis
M bovis is Niacin + but nitrate - (tb is +/+) |
|
What is the name of the type of growth that Tb shows in colonies?
|
Cording factor
Forms rope-like colonies on Middlebrook Due to very high lipid content in Tb |
|
|
Does Tb grow in NAP?
|
NO. all mycobacteria grow in NAP except TB (this is a silly question on an automated test, but has been asked on boards)
|
|

|
Barnsdale ulcer
M. ulcerans painless boil --> ulcer --> avasc coag necrosis |
|
|
Cavitary lesion in the lung
Positive AFB smear Niacin -, nitrate + |
M. kansasii!
Photochromogen (yellow > light) Clinically mimics Tb Tb is Niacin+ and nitrate +, and not a chromogen |
|
|
Swimming pool granuloma
No growth at 37C; growth at 30C |
M. marinum
(skin lesions like colder temps - grows at 30C) PHOTOCHROMOGEN Traumatized skin exposed to water (pools, fish tanks) and can mimic sporotrichosis with spread up the arm in lymphatics |
|
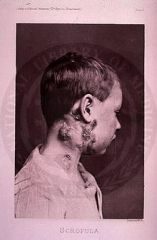
Original cause of scrofula (Mycobacterial cervical lymphadenitis)
|
M scrofulaceum
SCOTOCHROMOGEN (now scrofula is usually caused by TB) |
|
|
Egg nest colony on Middlebrook agar?
|
M. xenopi
scotochromogen grows in hot water |
|
|
Positive AFB in stool
|
MAC (avium * intracellulare complex)
AIDS and old ladies that smoke Disseminated Dx wtih DNA probe **usually a non-photochromogen but in AIDS it can have yellow color |
|
|
Rapid growing AFB (3-5d) that is arylsulfatase positive
|
M. fortuitum/chelonea complex
Found in environment |
|
|
Sporotrichoid spread
|
M. marinarum (swimming pool granuloma)
M. fortuitum/chelonae complex (rapid growers) |
|
|
Mycobacteria that is always a laboratory water contaminant
|
M. gordonae
|
|
|
Mycobacteria that is weakly associated with Crohn's disease
|
M. paratuberculosis
|
|
|
Subcutanous painful nodules in AIDS patients; organism requires heme to grow
|
M. haemophilum
|
|
|
Mycobacteria that can grow at 52C
|
M. thermoresistible
|
|
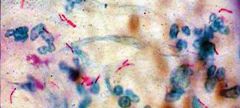
|
M. leprae
acid fast "cigar packets" |
|
|
Stain classically used for M. leprae and rhodococcus?
|
Fite stain
|
|
|
Animal reservoir of M. leprae
|
Armadillos
(colder body temperatures; M. leprae likes 27-30C, which is why it commonly involves the extremities) |

