![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back

You receive a proficiency test unknown in your microbiology lab. You are told the specimen is from a wound, so you
plate the specimen onto your four standard agars. Pictured are the colonies on MacConkey agar. Based on these findings, you perform an indole test and find that it is positive. What is the MOST LIKELY organism? a. Citrobacter freundii b. Klebsiella pneumoniae c. Pseudomonas aeruginosa d. Klebsiella oxytoca e. Proteus |
D. The colonies pictured are growing on MacConkey agar and are pink, which indicates that they are lactose
positive. Of the choices, only the Klebsiella and C. freundii are lactose positive. The colonies are mucoid, which is most characteristic of Klebsiella species due to their capsule. Differentiation between K. pneumoniae and K. oxytoca can be made by testing for indole. K. pneumoniae is negative for indole while K. oxytoca is positive. Klebsiella are gramnegative rods carried in the nasopharynx and the bowel and are a frequent cause of urinary tract infections. |
|

You isolate a Staphylococcus aureus on a specimen from a wound. You test for Erythromycin susceptibility and find
that the organism is resistant. You perform a D-test disk diffusion test to evaluate clindamycin inducible resistance. Based on the results pictured, can you treat this patientʼs infection with clindamycin? a. No. The discs are too close together and therefore the test is not valid b. No. The zone of resistance around the clindamycin disc indicates that the bacteria is resistant to clindamycin c. No. Because there is no zone of inhibition around the erythromycin disc, the test is not applicable d. No. The flattening of the clindimycin zone of inhibition near the erythromycin disc indicates the organism is resistant to clindamycin e. Yes. The size of the zone of inhibition surrounding the clindamycin disc indicates that the bacteria is susceptible to clindamycin |
D. D Zone Test for Inducible Clindamycin Resistance in Methicillin Resistant Staphylococcus Aureus (MRSA)
|
|

You receive a cultured specimen on a MacConkey plate. Based on the growth pictured, you perform an oxidase
test, which is positive. What is the BEST organism identification for this specimen? a. Proteus mirabalis b. Enterobacter cloacae c. Pseudomonas aeruginosa d. Klebsiella pneumoniae e. Escherichia coli |
C. Based on the picture, the organism growing on the plate is lactose negative. Of the choices, the only
organisms that fall into this category are Pseudomonas and Proteus. Differentiation can be made by an oxidase test, which is positive with Pseudomonas and negative with Proteus. Pseudomonas is a Gram-negative rod that is slightly curved and has one or more flagella. The organisms are lactose non-fermenters on MacConkey agar, oxidase positive and catalase positive. Pseudomonas aeruginosa is known to cause folliculitis in association with swimming pools and whirlpools, “swimmers ear”, as well as infections in patients with cystic fibrosis. |
|
|
You receive plates from a respiratory specimen that exhibit no growth on a blood agar plate and growth of small
gray colonies on a chocolate plate. You perform a gram stain, which reveals small, pleomorphic gram-negative rods. Based on these results you conclude that this organism is a Haemophilus species. To further subtype the organism, you test for factor requirements and hemolysis. The next day, you examine the plate and based on the growth, you determine the organism is H. influenzae. What growth pattern most closely resembles the expected findings for this organism? a. Growth and hemolysis, does not require factor X, does not require factor V b. Growth and hemolysis, requires both factors X and V c. Growth and hemolysis, does not require factor X, requires factor V d. Growth but no hemolysis, requires both factors X and V e. Growth but no hemolysis, does not require factor X, requires factor V |
D. Haemophilus influenza type b is one of the leading causes of bacterial meningitis worldwide, especially in
young unvaccinated children. Infection with Haemophilus can also cause cellulitis, pericarditis and pneumonia. Pneumonia is typically caused by non-type b strains, most commonly serotype f. Haemophilus is a gram negative rod. Differentiating species can be accomplished by testing for factor requirements and observing hemolysis. All Haemophilus species isolated from humans require factor V. H. influenzae does not show hemolysis on blood agar and requires factor X. An alternate method for testing for factor X requirement is the porphyrin test. In addition, Haemophilus is one of the few organisms that show satellite growth around a streak of Staphylococcus aureus. |
|
|
In preparation for an upcoming laboratory inspection, you are reviewing your quality control procedures in the
microbiology department. You have a list of atypical bacteria-antibiotic resistance profiles that are posted and should alert the technicians to perform confirmatory testing. Which of the following bacteria-antibiotic resistance combinations is INCORRECT and should prompt retesting by another method to confirm resistance? a. Proteus resistant to cefazolin b. Klebsiella resistant to ampicillin c. Enterobacter resistant to ampicillin and cefazolin d. E. coli resistant to no antibiotics e. Serratia resistant to ampicillin, cefazolin and cefuroxime |
A. Strains of Proteus are resistant to nitrofurantoin but are susceptible to the remainder of the drugs that are
commonly tested. The other microorganism-drug combinations are expected patterns of resistance. |
|
|
Which spiral bacterium has hooks at both ends?
a. Leptospira b. Borrelia c. Treponema d. Brachyspira e. Helicobacter |
A. All of the choices are spiral bacteria, but only Leptospira has hooked ends. Leptospira is a tightly coiled,
right-hand spiraled bacteria. Infection of humans occurs most commonly via direct contact with infected animals through cuts on the skin or via the conjunctiva. Most infections have a mild clinical course and resolve while recognized infections present with sudden onset of fever, chills and myalgia. The minority of cases present with jaundice, acute renal failure, pulmonary hemorrhage and cardiac arrhythmias, known as Weilʼs disease. |
|
|
You finalize a report from a skin wound as no growth after 5 days. The clinician calls and he is concerned that the
specimen was not cultured correctly, as he was certain there was adequate material upon collection. He states that the patient had an abscess on the thigh and upon drainage, there was 25ml of purulent fluid expressed from the lesion. Following the drainage, a swab culture was taken for microbiology. The clinician sent the swab for gram stain, aerobic and anaerobic cultures. Your BEST response to address the clinicianʼs concern is: a. Occasionally organisms just do not grow and we cannot explain why. Ask the clinician to send another swab and the lab will repeat the cultures. b. A swab should only be used if no other type of specimen can be submitted and in that case, one swab should be submitted for each type of culture c. Swabs never contain adequate material and should not be used for culturing specimens in the microbiology laboratory d. Occasionally organisms just do not culture and we cannot explain why. Tell the clinician you will reculture the specimen from the original swab e. Tell the clinician you will allow the plates to incubate for another 3 days to see if there will be delayed growth and then issue an amended report at that time |
B. Preferred specimens for microbiologic culture include fresh tissue, fluid, exudates and instrumentation (i.e.
screws, plates, catheter tips). A specimen should be submitted to microbiology on a swab only when there is no availability of other types of specimens. Material submitted on a swab often yields an inadequate amount of material for culture. To increase the likelihood of having enough material for culture on a swab, one swab should be submitted for each type of culture the clinician desires. For example, one swab should be submitted for each of the following: Gram stain, aerobic culture and anaerobic culture, for a total of three swabs. |
|
|
You receive a respiratory specimen in the laboratory that is labeled bronchial washing and has been obtained by
bronchoscopy. As standard procedure in your lab, you culture the specimen to a blood and buffered charcoal yeast extract plate. On the third day, you examine the plates and notice colonies growing that you would describe as having a ground-glass appearance. You perform a Gram stain and see tiny gram-negative rods. There is no growth on the blood plate. What is the MOST LIKELY organism growing on the BCYE plate? a. Neisseria gonorrhoeae b. Mycoplasma pneumoniae c. Moraxella catarrhalis d. Burkholderia cepacia e. Legionella pneumophilia |
E. Legionella is a fastidious, slow growing organism. Buffered charcoal yeast extract should be used to allow
for the growth of the Legionella organism. The cultures must be observed for 7 days due to the slow rate of growth of this organism. L. pneumophilia is the most common organism and colonies have a ground-glass appearance with iridescent edges. Gram stain of the organism reveals tiny gram-negative rods. Hospital acquired Legionella most often originates in the water distribution system and environmental studies should be performed in these cases. |
|
|
You isolate an Enterococcus faecium from a urine specimen. Standard susceptibility testing is performed. What is
the MOST IMPORTANT antibiotic pattern to look for initially? a. Vancomycin resistance b. Clindamycin inducible susceptibility c. Aztreonam susceptibility d. Trimethoprim-sulfamethoxazole susceptibility e. Methacillin resistance |
A. Vancomycin or penicillin is typically combined with an aminoglycoside for the treatment of an enterococcal
infection. Recently, there is an increased incidence of organisms with acquired antimicrobial resistance to vancomycin. In the lab, it is important to test Enterococcal species for resistance to vancomycin. |
|
|
A urine specimen from a middle aged female is received in the lab and grows small white colonies on sheep blood
agar that are coagulase negative and positive for catalase. The Gram stain reveals Gram-positive cocci in clusters. The organism is plated onto a Mueller-Hinton agar and a Novobiocin disc is placed onto the plate. The next morning, the plate is examined and shows no zone of inhibition. What is the MOST LIKELY organism growing on this plate? a. Staphylococcus epidermidis b. Staphylococcus aureus c. Staphylococcus saprophyticus d. Staphylococcus lugdunensis e. Staphylococcus haemolyticus |
C. Many of the different species of Staphylococcus can be differentiated by simple testing. The coagulase
negative Staphylococcus organisms include S. epidermidis and S. saprophyticus. While both organisms are catalase positive, differentiation can be made using Novobiocin. S. saprophyticus is resistant while S. epidermidis is sensitive. |
|
|
Small white colonies are growing on a blood agar plate. You are suspicious of Staphylococcus aureus and attempt
to confirm the diagnosis with a catalase and coagulase. The catalase is positive but the coagulase is negative. Despite the result of the coagulase, you are still highly suspicious that the organism is S. aureus. You set up a tube coagulase test to investigate. After 4 hours, you note a firm clot in the tube. You continue incubation and check the tube after 24 hours and notice the clot has dissolved. Your control tubes have appropriate reactions. What is the BEST interpretation of this tube coagulase test? a. The specimen is not S. aureus, as the clot should not form before 4 hours b. The specimen is not S. aureus, as a formed clot should not dissolve before 24 hours c. The specimen is S. aureus, as any clot in the tube within the 24 hours is a positive test d. The specimen is S. aureus, as the clot must form before 4 hours and dissolve before 24 hours e. This test is invalid because a clot formed before 4 hours |
C. The tube coagulase test is the definitive test for coagulation. The tube test detects both free and bound
coagulase. The tube coagulase test is positive if any clot forms in the tube at any time during the incubation period. Some clots may develop quickly, especially within the first 4 hours. With time, the clot can lyse if the organism produces fibrolysin. This is important to remember, as tubes should no only be checked after 24 hours. The tubes should be checked at 4 hours and if no clot has yet formed, the tubes should incubate to 24 hours and be rechecked. A positive and negative control should be run with the test. The slide coagulase test detects only cell-associated clumping factor, also know as bound coagulase. |
|
|
You identify a Klebsiella pneumoniae on a plate from a respiratory specimen. To test the sensitivities for the
organism you use an automated minimum inhibitory concentration (MIC) device. The sensitivity results are ready the next morning and you review the report before sending out the final results. The report shows that the organism is sensitive to all antibiotics. What is your MOST APPROPRIATE next step? a. Finalize the report with the given sensitivities and send the report to the clinician b. Leave the sample on the automated MIC device for another 24 hours to give the machine more time to evaluate the sensitivities c. Finalize the report, stating that the organism is resistant to Ampicillin, despite the MIC results, since you know that all Klebsiella are intrinsically resistant d. Replate, incubate and repeat you initial tests that were used to identify the organism as Klebsiella pneumonia e. Repeat sensitivities with an alternate method, such as Kirby Bauer disc diffusion |
E. Ampicillin is a β-lactam antibiotic, for which Klebsiella species are intrinsically resistant. Klebsiella
organisms are typically sensitive to all other antibiotics. This result is most likely inaccurate, and should not be reported without rechecking the results. Leaving the specimen on the automated MIC device is not effective and will not yield correct results. The best approach for an automated MIC result of a Klebsiella organism that does not show resistance to Ampicillin is to manually check the sensitivity, by a method such as Kirby Bauer disc diffusion. Some labs will also repeat the sensitivities on the automated MIC device. |
|
|
You receive a call from the clinician regarding the previous case. She wants to know if the organism is sensitive to
TE. You tell her the zone of inhibition is within the sensitive range but there is mixed growth on the plate. She asks if the sensitivity is valid, since there is mixed growth. What is your BEST response? a. The mixed growth invalidates the sensitivity result for TE b. The organism is sensitive to TE and can be reported as such, despite the mixed growth c. The mixed growth can cause a false increase in the zone of inhibition for TE and should not be reported as sensitive d. The mixed growth can cause a false decrease in the zone of inhibition for TE and the result can confidently be reported as sensitive e. The organism is most likely sensitive to TE despite the mixed growth but the sensitivity should be performed again on a pure culture |
E. This picture is an example of mixed growth. A report should not be finalized when mixed growth is seen.
Growth of colonies within the clear zone typically indicates mixed growth, and colonies showing mixed growth should be subcultured, reidentified and retested. Occasionally, this picture can indicate mutant organisms growing in the clear zone, which will eventually become resistant to the antibiotic. For staphylococci and enterococci only, growth within the zone of inhibition around an oxacillin or vancomycin disc is indicative of resistance. |
|
|
You receive a blood agar plate and notice small white colonies surrounded by a zone of hemolysis. You suspect
the organism growing on the plate is a Streptococcus and you confirm your suspicion with Gram stain and negative catalase and negative coagulase tests. You type the Streptococcus and find that it is a Lancefield group B Streptococcus. What are the identified organism and the typical response to penicillin? a. Streptococcus agalactiae, resistant to penicillin b. Streptococcus pyogenes, resistant to penicillin c. Streptococcus agalactiae, sensitive to penicillin d. Streptococcus pyogenes, sensitive to penicillin e. Streptococcus bovis, resistant to penicillin |
C. Streptococcus agalactiae is Lancefield group B while S. pyogenes is Lancefield group A and S. bovis is
Lancefield group D. Of the two answer choices for S. agalactiae, C is the best choice. Streptococcus organisms are universally sensitive to penicillin, which is the drug of choice in these infections. Susceptibility testing is typically not performed, unless the patient has a penicillin allergy. S. agalactiae can be acquired by a newborn at birth, from vaginal colonization, which can result in an early onset of pneumonia and sepsis or a late onset of meningitis (associated with serotype III). Adults infected with S. agalactiae can present with meningitis (serotype II). Other manifestations include endocarditis, arthritis and urinary tract infection. |
|
|
Culture plates are made from the blood culture specimen of a 35-year-old man who clinically appears septic. The
following day you examine the plates and notice small translucent glistening colonies growing on the Chocolate agar. You perform a Gram stain and see abundant gram-negative cocci in pairs and are suspicious of Neisseria. To identify the organism, you decide to culture the colonies to another media and/or perform additional tests. Which of the following results is LEAST LIKELY to be helpful? a. Indole positivity b. Growth on Modified Thayer Martin media c. Butyrate esterase disk negativity d. Oxidase positivity e. Catalase positivity |
A. The major differentials in this question include Neisseria, Moraxella and Acinetobacter. Thayer Martin is a
useful way to selectively grow all three of these organisms and eliminate other less common diplococci organisms. Acinetobacter can be eliminated from the differential by performing the oxidase and catalase, which would both be negative. Both Moraxella and Neisseria are positive for oxidase and catalase. Moraxella can be differentiated from Neisseria by performing a butyrate esterase disk test (Catarrhalis test disk), which has a positive blue color change for M. catarrhalis and no color change for Neisseria. |
|
|
After confirming that the organism is Neisseria, you are asked to determine if the species is gonorrhoeae or
meningitidis. You decide the best method for differentiating is by testing for fermentation of different sugars. Which of the following patterns would be INDICATIVE of N. meningitidis? a. Glucose negative, lactose negative, maltose positive, sucrose negative b. Glucose positive, lactose negative, maltose negative, sucrose negative c. Glucose positive, lactose negative, maltose positive, sucrose positive d. Glucose positive, lactose negative, maltose positive, sucrose negative e. Glucose negative, lactose negative, maltose negative, sucrose positive |
D. Once you determine that the organism is Neisseria species, differentiation between N. gonorrhoeae and N.
meningitides can be made by examining acidification properties with different carbohydrates. N. gonorrhoeae acidifies only glucose (G, gonorrhoeae and glucose) while N. meningitides acidifies both glucose and maltose (M and G, in maltose and glucose and meningitides). N. meningitidis most commonly is present in the CSF and the blood, causing meningitis and sepsis. |
|
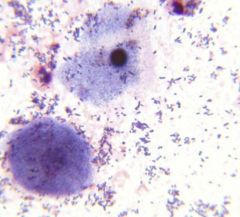
A clinician calls for a preliminary report on a wound specimen. As the resident on microbiology, you are asked to
review the Gram stain made from the specimen. Based on the image, what is the MOST APPROPRIATE interpretation of this stain? a. Gram positive rods in chains are present, issue a preliminary report b. The specimen is under-decolorized and should be repeated before giving the clinician an interpretation c. The specimen was inappropriately collected, ask the clinician to recollect the specimen d. The Gram stain was over-decolorized and should be repeated before giving the clinician any information e. In preparation of the Gram stain, saffarin was never placed onto the slide |
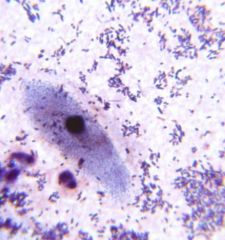
B. In evaluating a Gram stain, epithelial cells and/or white blood cells are built in controls that will help you
discern that the process was performed appropriately. In a Gram stain, epithelial cells/ WBCʼs should stain pink. If the stain is under-decolorized, as in this case, the epithelial cells are blue. These cells are not as useful in interpreting over-decolorization, as they will be pink in both appropriately decolorized and over-decolorized specimens. If saffarin was not used, there would be no evidence of pink coloration and the epithelial/ WBCʼs would be colorless. |
|

A patient is admitted to the hospital and the clinician orders a nasal swab to screen for methicillin resistant
Staphylococcus aureus (MRSA). The swab is received in the microbiology laboratory and is plated onto a CHROMagar MRSA plate. Based on the growth you see in the image, you perform a latex agglutination test, which is positive. The BEST interpretation of this specimen is: a. The growth indicates that the organism is a methicillin resistant Staphylococcus aureus b. The growth, not the color, indicates that the organism is Staphylococcus aureus and that it is sensitive to methicillin c. The color of the organisms indicate that the organisms growing on the plate are methicillin resistant Staphylococcus aureus d. The color of the organisms indicate that the organisms growing on the plate are methicillin sensitive Staphylococcus aureus e. The color of the organism growing on the plate is suggestive of growth of a red pigmented Serratia species |
Answer: C. CHROMagar MRSA is a qualitative method to detect nasal colonization by methicillin resistant S. aureus.
This test is only a screening test that is performed on anterior nares swab specimens. CHROMagar is a selective and differential medium that incorporates cefoxitin and specific chromogenic substances to detect MRSA. Growth alone does not confirm that the organism is methicillin resistant S. aureus. The mauve-colored colonies confirm methicillin resistant S. aureus. If the organisms are not pink, the growth is not methicillin resistant S. aureus. Organisms other than MRSA can grow and produce a blue or green color, white or no color at all. Coagulase positivity can then be confirmed. Serratia should not grow on this selective media. |
|

While examining the plates from a wound specimen that came from the operating room, you identify tiny, white
creamy colonies that appear to be yeast, mixed with some larger white colonies. You notice that the plates were cultured late the previous evening, but you do not want to delay your identification and susceptibility another day. You decide to carefully isolate only the larger colonies and perform disc diffusion susceptibility testing on a Mueller-Hinton plate. Based on the image, what is the BEST interpretation of this test? a. Based on the growth of small colonies within the zone of inhibition, the organism is susceptible to TE b. Based on the growth of small colonies within the zone of inhibition, the organism is resistant to TE c. The growth of small colonies within the zone of inhibition indicates that there is mixed growth d. The growth of small colonies within the zone of inhibition indicates that the organism has a delayed resistance to TE e. The growth of small colonies within the zone of inhibition indicates that the organism has delayed susceptibility to TE |
C.
|
|

A urine specimen from a middle aged female in received in the microbiology laboratory. You notice on the patientʼs
history that her chief complaint is urinary tract infection symptoms with alkaline urine. You examine the blood agar plate and see >100 k/ml of pinpoint smooth whitish-gray colonies growing on the aerobic blood agar plate. There is no growth on the MacConkey plate. You decide to make a Gram stain and notice that as you try to pick a colony from the plate, the colony is very sticky and difficult to sample. While you wait for the Gram stain to dry, you perform a catalase, which is positive. Examination of the Gram stain reveals small slightly curved Gram positive rods. Based on the Gram stain and other findings, what is the MOST LIKELY diagnosis? a. Staphylococcus saprophyticus b. Corynebacterium urealyticum c. Escherichia coli d. Enterococcus fecalis e. Stenotrophomonas maltophilia |

7a: B., 7b: D. C. urealyticum is one of the more frequently isolated clinically significant Corynebacterium species in
clinical specimens, often responsible for urinary tract infections. Gram stain reveals Gram positive, slightly curved rods. C. urealyticum is catalase positive and strongly urease positive. C. urealyticum urine splitting capability results in alkaline urine and the formation of struvite crystals, which have the easily identifiably “coffin-lid” appearance. Colonies tend to be sticky when sampling from agar and are therefore difficult to remove. Cystine crystals are hexagonal. Tyrosine crystals are needle like. Calcium oxalate crystals are square with a three dimensional point and resemble envelopes. Urate crystals are small, clear, rounded circular objects often with striations radiating from the center. |

