![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back
|
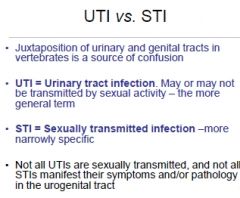
Compare STIs & UTIs (4)
|
|
|
|
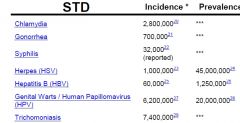
Name the THREE most common STIs world wide
|
|
|
|
Name the THREE most common STI's in the USA
|

|
|
|
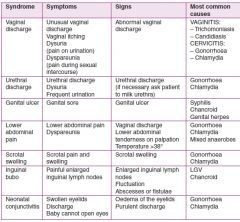
For the following Syndromes, describe the Symptoms, Signs & Most Common causes for
1. Vaginal Discharge (4, 1 & 4) 2. Urethral discharge (3, 1 & 2) 3. Genital Ulcer (1, 1 & 3) 4. Lower Abdominal Pain (2, 1 & 3) 5. Scrotal swelling (2, 1 & 2) 6. Inguinal bubo (1, 3, & 2) 7. Neonatal conjunctivitis (3, 2 & 2) |
|
|
|
Definition of SEX
|
1. MUST BE EXPLICIT
|
|
|
More than 340 million news cases of what STI's in Men & Women between (15-49rs old) (4)
|
1.Spyhillus, Gonorrhea, Chlamydia & Trichomoniasis
2. Blacks |
|
|
STIs Disproportionately effect
1. Gender (2) 2. Age group (2) 3. Race 4. 15-24yr olds are ___Sexual Active Population & _____All new STDs |
1. Women, Infants of Infected mothers
2. Adolescents & Young Adults 3. Communities of Color 4. 1/4 & 1/2 |
|
|
Names the Organisms that have gone from GIT to STD (3)
|
1. Giardia labilia
2. Amoeba 3. Shigella |
|
|
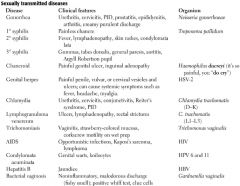
Name the Clinical Features & Organism for the following:
0. Gonorrhea (7 & 2) 1. 1⁰ Syphilis (1 & 1) 2. 2⁰ Syphilis (4 & 1) 3. 3⁰ Syphilis (5 & 1) 4. Chancroid (2 & 1) 5. Genital Herpes (6 & 1) 6. Lymphogranuloma venereum (4 & 3) 7. Trichomoniasis (4 & 1) 8. AIDS (3 & 1) 9. Condylomota acuminata (2 & 2) 10. Hepatitis B (1 & 1 11. Bacterial vaginosis (5 & 1) |
|
|
|
Pelvic Inflammatory Disease
1. TWO bugs & difference 2. Symptoms (2) 3. Symptoms may also include (4) |
1. Chlamydia trachomatis (subacute, often undiagnosed) & Neisseria gonorrhea (acute)
2. Chandelier sign (cervical motion tenderness), Purulent cervical discharge 3. Salpingitis, Endometeritis, Hydrosalpnix & Tubo-Ovarian abscess |
|
|
Name anaerobic gram -ve bacteria that can lead to female genital tract infections (2) Found in abcsesses
|
1. Prevotella bivia & Bacteriodes fragilis (common in abscesses)
|
|
|
Nicnames for Gonorrhea
|
Clap
The Drip Piss of Fire Bacterial Urethritis |
|
|
Compare the following Bacterial Infections across Pathogen & Signs & Symptoms
1. Gonorrhoea (1 & 5) 2. Chlamydia (1 & 5) 3. Syphillus (1 & 3) 4. Chancroid (1 & 2) 5. Granuloma inguinate or Donovanosis (2 & 3) |

|
|
|
N. gonorrhea
1. Resevoir 2. Tramsmitted by 3. RARE transmission 4. Infection ↑ |
1. Asymptomatically Infected Individual
2. Sexual contact 3. Formite 4. likeley hood of AIDS infection |
|
|
Gonorrhea
1. Peaked in 2. Currently 3. More common in |
1. 70S
2. Descreasing 3. Men |
|
|
Gonorrhea
1. Male symptoms (2) Restricted to Women 2. Site of Infection 3. Symptoms (3) 4. Disseminated infection often occur 5. 40% patients w/ Gonorrhea have |
1. Purulent Urethral discharge & dysuria (urethra)
2. Cervix 3. Vaginal dischrage, Dysuria & Abdominal Pain 4. Females 5. Chlamydia |
|
|
Neisseria gonorrhoeae Characteristics
1. Gram 2. Motile 3. Spore 4. Other (3) 5. Name Virulence factors (5) |
Gram-ve diplococci, non motile & non spore forming
4. Oxidase +ve, fstiduos & outer surfeace has multiple antigens 5. Pili, Opa, Por protein, LOS & Iron binding proteins |
|
|
Neisseria gonorrhoeae
Pathogenesis 1. Attaches to via Pili (3) 2. MoA Pili 3. Role of Opa 4. Role of LOS (1) 5 .Other VFs |
1. Columnar epithelium, Distral Urethra & Cervix
2. Antigenic variation by DNA rearangement 3. Opaque colony attachement 4. Induces TNFα 5. Por protein & Iron Binding Protein |
|
|
Neisseria gonorrhoeae
1. Organisms multiply where 2. Thus, large #s 3. Spread in females to cervix via 4. Seeding my a occur (common in what patients) 5. Chronic infections can causes (3) |
1. In Situ in huge numbers
2. Secreted by both men & women 3. Urethral or Uterine Contractions 4. Blood (complement defecient) 5. Scarring/Strciture of fallopian tube or Urethra |
|
|
Neisseria gonorrhoeae DIAGNOSIS
1. Men 2. Women (3) |
1. Gram-ve diplococci in SYMPTOMATIC men
2. Isolation on media for 24hrs. Thayer Martin, Chocolate II Agar & Oxidase -ve + colonies |
|
|
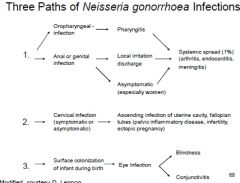
Describe the THREE pathways for N. gonorrhoeae Infections
|
|
|
|
Neisseria gonorrhoeae
1. Treatment limited to 2. What is the Gonococcal Isolate Surveillance Project |
1 .cephalosporins
2. Monitors durgs used to treat Neisseria gonorrhoeae |
|
|
Chlamydia trachomatis epi
1. Most common 2. Most cases still go 3. Sever impact on (2) 4. Infection |
1. Reported notifiable disease
2. Undiagnosed 3. Youg & Minority WOMEN 4. ↑ Risk of HIV infection |
|
|
Chlamydia trachomatis
1. Transmission to Newborn baby during 2. 50% risk for 3. 20% risk |
1. Labor
2. Conjuctivitis 3. Infection of lung |
|
|
Chlamydia. The biovar is associated with
1. A, B, Ba & C 2. D-k 3. LGV1-3 |
1. Agent of Trachoma
2. Conjuncitivitis, Infant Pneumonaie & Urogenital disease 3. Lymphogranuloma venereum |
|
|
Chlamydia trachomatis. CLinical Presentation
1. Ussualy 2. If present, symptoms (2) d.t (2) 3. 40% of Untreated women develop 4. Leading to (3) 5. Male complications |
1. Asymptomatic
2.Nonspecific:Vaginal dscharge & burning on urination (diredt distruction of cells, host inflammatory response) 3. PID 4. Infertility, Ectopic Pregnancy & Chronic Pelvic Pain 5.Epididymitis & Urethritis (both rare) |
|
|
Chlamydia trachomatis. Characterestics
1. Infectious form 2. Noninfectious form 3. Type of bacteria 4. Entry via (2) |
1. Elementary bodies
2. Reticulate Bodies 3. Obligate intracelullar parasite 4. Abrasions/Laceration |
|
|
Chlamydia trachomatis
Key difference vs. Gonorrhea in males (2) |
1. Enlarged scrotum & mucus discharge( large volume)
|
|
|
Chlamydia trachomatis Pathogenesis
1. Receptos for EB (6) 2. Immunity |
1. Mucus membrane of Urethra, Endocervix, Endometrium, Fallopian Tubes, Ano-REctum, Respiratory Tract & Conjunctivae
2. NOT long lasting |
|
|
Chlamydia trachomatis
1. Two types of tests (2) 2. Screening recommended for |
1. Swab or Nuclear probe (if available)
2. Sexually active women under 26 yrs old or Women with new sexual partners |
|
|
Chlamydia trachomatis
1. Screening & Treatment reduce what by 50% 2. Reducing impact Chlamydia trachomatis also requires |
1. PID
2. Reducing incidence in males |
|
|
Chlamydia trachomatis
8 step life cycle of Chlamydia |

|
|
|
Treponema pallidum (aka Syphillus)
1. 1⁰ & 2⁰ epi? 2. Transmission via 3. Curable at what stage 4. Genital Ulcers |
1. ↓ in the 90s, then ↑2000-07
2. Direct contact w/ 1⁰ & 2⁰ lesions 3. 1⁰ & 2⁰ 4. ↑ likelihood of HIV transmission |
|
|
Treponema pallidum 1⁰ Stage
1. Develops post infection (4) 2. Incubation period 3. Disappears w/ treatment after 4. W/O treatment 5. % of cases that resolve 6. Diagnosis |
1. Hard, painless but Sensitive CANCRE (ulcer), w/ Thin Greyish crust
2. 9-90 days 3 1 week 4. 4-12 weeks 5. 75% 6. DARKFIELD microscopy |
|
|
Treponema pallidum 2⁰ Stage
1. Develops post infection (4) 2. Incubation period 3. Disappears w/ treatment after |
1. Maculopapular Rash (palms & soles), CONDOLYLOMA LATA, & Flue like symptoms
2. 2-8 weeks after Ulcer 3. |
|
|
Treponema pallidum 3⁰ Stage
1. Inucbation 2. key Symptoms 3. CNS (3) 4. Cadiovascular 5. Hypersensitive granulomatous reaction (2) |
1. 15-20 yrs
2. Stromal Haze, Hutchinson's Teeth & Diffuse CHRONIC inflammation 3. Dementia, Meningitis & Hallucination 4. Thoracic Aortic Aneurysm (Obliterative endarteritis of Vaso Vasorum) 5. Destructive to Visera or Mucocutaneous AReas |
|
|
Congenital Infection of Treponema pallidum
1. Transmission 2. Most cases (2) 3. Effects seesn |
1. Uterine & Placental Membrane
2. Spontaneous or Septic Abortions 3. SADDLE NOSE, stromal haze & Hutchinson's Teeth |
|
|
Treponema pallidum Characteristics
1. Type of bacteria 2. Motility 3. Replication 4. Pathogen 5. Other (3) 6. VFs (2) |
1. Tightly coiled spirochetes, w/pointed straight ends.
2. 3 flagella @ each end 3. Slow & NOT in cell free cultures 4. Obligate Human pathogen 5. Fastitduous & Outermembrane w/ NO LPS or PORINS 6. Hyalurinadase & Fibronectin |
|
|
Treponema pallidum PATHOGENESIS
1. Host's response to pathogen 2. Promotes adherence 3. Spreading factor? via? 4. Protects vs. Phagocytosis |
1. Tissue destructin & Lesion (2)
2. Outer membrane 3. Hyaluronidase via. Perivascular Infiltration 4. Fibronectin |
|
|
Treponema pallidum 1⁰ Stage Pathogenesis
1. Enters tissue? Via? 2. Multiplication 3. Symptoms (2) 4. Disseminate via |
1. Subepithelial via Skin Breach
2. Slow 3. Endarteritis & Granulomas 4. Lymph & Bloos |
|
|
Treponema pallidum PATHOGENESIS
2⁰ Stage 3⁰ Stage (2) |
2⁰- Evasion of the immune system
3⁰ - Chronic inflammation, damage to CNS |
|
|
Treponema pallidum diagnosis
1. Issue 2. Testing (2) |
1. Fastiduous: HIGHLY SENSITIVE organism
2. DARKFIELD microscopy & serology |
|
|
Treponema pallidum
1. Screened (2) 2. Treatment |
1. MSM w/ anually & Pregnant Women prenatal screenign
2. Penicillin vs. neurosyphillus |
|
|
Haemophilis ducreyi
1. Causes 2. Enhances transmission of 3. Geographic spread (4) 4. Accounts for what % of Genital Ulcer diseases in these regions |
1. Chancroid (painful ulcer of genital region
2. ↑HIV 3. Predominant in Tropics (also Africa, Asia & Latin America 4. 20-60% |
|
|
Haemophilis ducreyi:
1. Clinical Presentation (3) 2. Incubation 3. Also have in 25% of cases 4. Difference vs. Syphillus |
1. Soft chancre, chancroid & PAINFUL Genital ulcer
2. 5-10days 3. Spontaneous rupturing buboes 4. Chancre: No greyish crust & Faint Red rimd |
|
|
Haemophilis ducreyi
1. Characterestics (2) 2. Pathogen 3. other |
1. Gram -ve rod (coccobacilli)
2. ExtracellularObligate Human anerobe 3. Fastiduous |
|
|
Haemophilis ducreyi
Pathogenesis 1. VF responsibe for resisting phagocytosis 2. VF responisble for tissue destruction |
1. Outer Membrane Serum Resistance Protein
2. CYTOLETHAL DISTENDING TOXIN (CDT) & Hemolysin |
|
|
Haemophilis ducreyi
0. Stain 1. Diagnosis (3) 2. Culture 3. Accuracy of clinical diangosis |
0. Gioneten Violet Simple Stain
1.Antigen detection, Serology & Genetic Amplifcation 2. not easily accesible 3. 30-80% |
|
|
Haemophilis ducreyi
1. AB used for treatmen |
1. erythrmycin
|
|
|
Compare Chancroid & Syphillus across
1. Chacnre (2) 2. Pain 3. Diagnosis |

|
|
|
Bacteria Vaginosis/Vaginitis
1. Describe 2. Discharge (4) 3. Other symptoms 4. MOST COMMON 5. Having BV can |
1. Normal BALANCE of bacteria DISRUPTED & replaced by overgrowth
2. Fishy odor, thin, white or gray 3. Often ASYMPTOMATIC 4. In Women of CHILD BEARING age 5 ↑ HIV Infection risk. |
|
|
Bacteria Vaginosis/Vaginitis
1. Under Microscope 2. Differentiates vs. 3. What bacteria is ↓ed 4. pH |
1. CLUE cell
2. Candidasis & Trichomanis 3. Lactobacilli 4.pH >4.5 |
|
|
Describe Thrichomoniases & Candidiasis across
1. Bug 2. Symptoms |

|
|
|
Candida Albcians
0. Layman name 1. 75% of who have @ least 1 occurrence 2. Characterestics (3) 3. Normal flora of 4. Commensuals (3) |
0. Yeast Infection
1. ADULT WOMEN 2. Oval, yeast form w/ PSEUDOHYPHAE 3. GIT 4. Vagina, Urethra & Skin under |
|
|
Candida Albcians
1. Discharge 2. At risk conditions (3) 3. Pathogenic path way 4. In other parts of the body |
1. Thick cottage cheese like discharge which is odorless.
2. Pregnancy (hormonal disturbance) Diabetes & Use of Broad spectrum Antibiotics 3. pH sensing pathway 4. Oral thrush in Mouth & affects finger nail |
|
|
Trichomoniasis
1. Common 2. Site of Infection in Women 3. In Men 4. Transmission (2) 5. Region 6. Inflammation ↑ |
1. In young sexually active Women
2. Vagina 3. Urethra 4. Sexual & Formite 5. Tropical & Worldwide 6. Risk of Infectionr |
|
|
Trichomoniasis
0. Trichomonas vaginalis is a 1. Most women are 2. Incubation 3. Vaginal discharge 4. Clinical presentation (4) 5. pH |
0. Protozoan
1. Commonly asymptomatic 2. 5-28 days 3. Frorthy 4. Cervix has "STRAWBERRY" appearance", Itching, Burning & Painful urination 5. pH>4.5 |
|
|
Trichomonas vaginalais
0. Smear for Microscopy (2) 1. Identification on Microscopy (3) 2. Other diagnostic techniques (3) 3. Treatment |
0. Vaginal or Urethral discharge
1. Parasite w/ 4 flagella, w/ Membrane responsible for motility 2. Serologic tests, Nucleic Acid Probe & Culture 3. Metronidazole |
|
|
Compare the following Viral STIs across PATHOGEN responsible & Symptoms & Signs:
1. AIDS (1 & 5) 2. Herpes Genitalis (1 &2) 3. Genital Warts & Cervical Cancer (1 & 4) 4. Viral Hepatitis (1 & 5) 5. Cytomegalovirus (1 & 3) 6. Molluscum contagiosum (1 & 3) |

|
|
|
HHV-1 & HHV-2 EPIDEMIOLOGY
1. Most genital Herpes caused by 2. Transmission 3. HHV-1 &-2 Can be found in 4. Virus may be also released 5. Genital Herpes is common in 6. Epid history 7. More common in |
1. HHV-2
2. By close contact & Sexual Contact via Mucosal membranes or Breaks in the skin 3. Ulcers that virus cause 4. Between OUTBREAKS 5. USA in adults & Adolescents 6. ↓ of the past Century 7. Women (1 in 4) than Men (1 in 8) |
|
|
HHV-1 & HHV-2: Clinical PRESENTATION
1. Most individuals 2. 1⁰ Symptom? (4) Where (3) With? (2) 3. What happens when Blisters break 4. Long to heal 5. Subsequent outbreaks when (2) 6. Type 7. Site of Genital hepres in women 8. |
1. Present NO symptoms
2. 1 or More FEVER Blisters or COLD sores & VESICULOPAPULAR lesions around Genitals/Rectum/Mouth (Itching & Vaginal Discharge 3. Tender Ulcers 4. 2-4 Weeks 5. Weeks, Months 6. Severity ↓es with Age & Time 7. Vulva 8. Penile Shaft |
|
|
HHV-1 & -2
1. Shape, Structure 2. Envelope 3. Nucleic Acid 4. Baltimore Class 5. Characterestic 6. Share (3) 7. Encode enzymes that provide |
1. Lage Icoasahedral
2. ds DNA 3. Envelope 4. Class I 5. UBIQUITOUS 6. Antigenic determinants, Tissue Tropism & Disease symptoms 7. good ANTIVIRAL targets |
|
|
Baltimroe I virus Review
1. NA 2. Unique Characterestics |
1. ds DNA
2. Immediate Early, Early & Late Protien |
|
|
HHV-1 & HHV-2: PATHOGENESIS
1. Initially infect & replicate in Viruses are 2. Lytic in? Causing? 3. Persistent in (2) 4. Latent in |
1. Mucoepithelial Cells
2. Most cells. COWDRY type A IBs & Synctia 3.Lymphocytes & Macrophages 4. Neurons |
|
|
HHV-1 & HHV-2: PATHOGENESIS
1. Virus blocks effects of? 2. Preventing? 3. Escapes? (2) Via? 4. Recurrence occurs d/t |
1. IFN
2. CD8 T-cell recognition of Infected cells 3. Antibody Neutralization & Clearance BY Going into hiding |
|
|
HHV-1 & HHV-2. Predilction for
1. HHV-1 only (6) 2. HHV-2 only (2) 3. Both (4) |

|
|
|
HHV-1 & HHV-2: DIAGNOSIS
1. Test 2. Between outbreaks |
1. Sample of Ulcer
2. Serology |
|
|
HHV-1 & HHV-2
1. Cure 2. Treatment 3. Suppression therapy can |
1. NO CURE
2. Antiviral medications (enzymes) 3. Reduce Transmission |
|
|
Condyloma
1. LATA 2. ACUMINATUM |
1. 2⁰ SyphiLLus
2. HPV 6 & 11 |
|
|
Ayclovir
1. DOES not work vs. what Herpes (2) 2. Works vs what Herpes (2) 3. Why? |
1. HHV-4 & HHV-5
2. HHV 1-3 3. Presence of viral THYMIDINE KINASE |
|
|
Human Papillomavirus (HPV)
1. Most common 2. Lifetime Culmative risk of Acquring a form of HPV 3. Low risk realated to 4. High risk related to (2) 5. What other cancers has it been related to 6. Very rarely transmitted? Reults in (2) 7. 16 & 18 Responsible for what % of Cervical cancer 8. 6 or 11 Genital warts |
1. #1 VIRAL STI
2. 80% 3. Condyloma ACUMINATA 4. Dysplasia & Cervical Cancer 5. 305 of Head/Neck cancers 6. Vaginal delviery leadin to Warts & Voice box on child 7. 70% 8. 90% |
|
|
HPV
1. name the Other high risk types |
1. 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73 & 82
|
|
|
HPV General Symptoms
1. Infections 2. Incubation |
1. Often asymptomatic
2. Weeks/Months/Years 3 |
|
|
HPV 6 & 11
1, Condylomata ___ 2. Warts appear where? As (7) 3. in women (4) 4. In Men (4) 5. Femal age group 6. Male Age group |
1. ACUMINATA
2. Bumpsin genital area, raised or flat, single or multiple, small or large, sometimes CAULIFLOWER 3. Vulva, Vagina, Anus, Cervix 4. Penis, Scrotum, Groin or Thigh 5. 20-24yrs old 6. 25-29 years old |
|
|
HPV 16 & 18
1. Main Cancer in females 2. Other cancers (4) 3. HPV is more like to turn to cancer in the mouth, then |
1. Cervix
2. Vulva, Vagina, Anus & Penis 3. Smoking & Alcohol |
|
|
HPV -16 & 18 PATHOGENESIS
1. Enters skin via 2. Targets 3. Oncoproteins & Target GEnes |
1. Mircoabrasions
2. Basal Layer Eptithelium 3. E6 → p53 & E7 →pRb |
|
|
HPV Diagnosis
Geneital Warts 1. Diagnosed by 2. What is used to identify Flat warts 3. Cervical changes identified by 4. What is better |
1. Visual inspection
2. Acetic Acid 3. Pap Smear 4. HR-HPV detection tests (PCR or NA hybrdiization) |
|
|
HPV
1. L1 → 2. L2 → 3. E6 → (2) 4. E7 → |
1 & 2 Site of Vaccination (Both are Cpasid proteins)
3. →p53 & Telomerase 4. pRb |
|
|
HPV Screeningn
1. Before 30 2. After 30 |
1. Everyone has it: UNECESSARY
2. High risk subtype |
|
|
HPV Screening Guidlines
1. Start @ what age? 2. Screen every 2 years when? 3. At 30 screen every 3 years if 4. Negative if (3) 5. Annual screening if (4) 6. Stop screening at 60 or 70 if (3) 7. Stop screenig also if (2) |
1. 21 yrs of Age
2. 21-29 3. Negative 4. Negative CYTOLOGY 3 prev. paps, NIELM & Negative HR & HPV tests in 1 year & no history of High Grade lesions 5. Immunocompromised, History of CIN II, III or Cancer or Exposure to DES in utero 6. 3 prior normal smeasrs or no hsitroy of ABNORMAL screening in last 10 years 7. Hysterectomy for benign diseae w/ no hist history of Abnormal pap smeasr |
|
|
HPV Vaccinate
GARDASIL 1. Vs.types 2. Vs. protein 3. For girls & boys 4. why boys Cervavix 5. Only 6. Both are what type of vaccine 7. # of DOSES |
1. 6, 11, 16 & 18
2.L1 & L2 3. 9-26 4. prevent transmission 5. 16 & 18 6. Prophylactic 7. 3 |
|
|
Name the Top Three causes of Children born with long term congenital defects
|

|

