![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
15 Cards in this Set
- Front
- Back
|
When a bipolar lead (+ end and - end) is recording electrical potential in the heart. What will cause a greater (larger) recording.
Current moving parallel to the + end or perpendicular to the + end. |

The leads only detect current moving parallel to them.
If current is running perpendicular it won't detect anything. |
|
|
The general path of ventricular depolarization
|

|
|
|
Where to the precordial leads measure?
|

|
|
|
Describe the events which are occurring for the waves on an EKG:
- P Wave - QRS Wave - T Wave |
P Wave = Atrial depolarization
QRS = Ventricular depolarization, Atrial repolarization (can't see) T Wave = Ventricular repolarization |
|
|
For Sinus Rhythm:
What is the normal BPM for the heart? What is considered tachycardia? What is considered Bradycardia? |
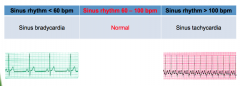
Normal: 60-100
Tach- Over 100 Brady- Under 60 |
|
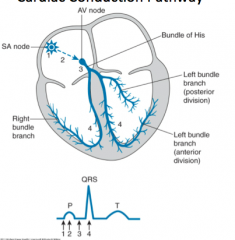
Label The conduction pathway of the heart in this diagram
|
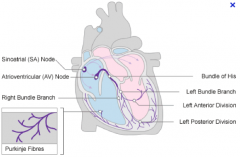
|
|
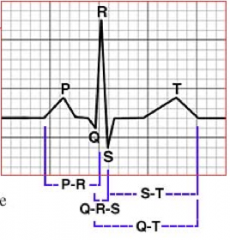
In ECG:
1. What is represented by the P-R interval? And what is a normal time? 2. What does the QRS interval represent? And what is the normal time interval? 3. What does the Q-T interval represent? And what is the normal time interval? 4. What is represented with an ST segment? What are 2 ST abnormalities and what do they mean? |
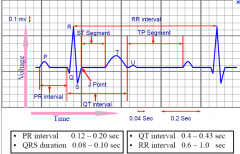
1. PR - Represents Atria depolarization and delay in AV junction (thus allowing atria to contract before ventricles)
Time: 0.12-0.20 s or 3-5 small boxes 2. QRS - Ventricular depolarization. Time: Less then 0.10 s or 2.5 small boxes 3. QT - Is the first ventricular depolarization to the last ventricular re-polarization. SHOULD vary with heart rate (faster shorter interval) Time: Use corrected QT = (QT)/[squareRoot of R interval)] - Should be less then 0.44s Rough Rule: Less then 1/2 of R-R interval 4. ST - Contraction of the ventricles ST Elevation - May be a Myocardial Infarction ST Depression - Hypokalemia or unstable angina |
|
|
What are causes of a shortened PR interval?
long PR interval? |
high catecholamine states
preexcitation syndrome (e.g. WPW) junctional rhythm First degree block |
|
|
What are the causes of a wide QRS?
|
0.10 - 0.12 - incomplete BBB
> 0.12 - BBB ventricular ectopic rhythm severe hyperK toxic drug effect |
|
|
The ECG evolution of an STEMI
and why is there ST elevation? |
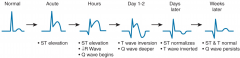
The ST elevation is because that portion of the myocardium repolarizes faster
|
|
|
Match the ECG leads with what area of the heart they are monitoring:
A) V1, V2 B) Lead 1, aVL, V5, V6 C) Lead 2, Lead 3, aVF D) V3, V4 i) Inferior ii) Anterolateral iii) Anteroapical iV) Posterior V) Anteroseptal |

A.) V1, V2 = Anteroseptal
B.) L1, aVL, V5,V6 = Anterolateral C.) L2,L3, aVF = Inferior D.) V3, V4 = anteroapical Posterior is usually leads V7-V9 (rarely used) |
|
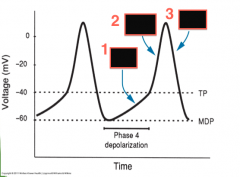
In the action potential of a pacemaker cell, what ions are responsible for the voltage changes see in the diagram?
|
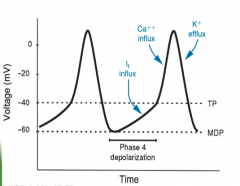
1. If or Pacemaker current/Funny Current (slower Na+ channels)
2. Calcium influx 3. Potassium efflux TP = Threshold potential MDP = Maximum diastolic potential |
|
|
In regards to Pacemaker cells describe the changes that occur to pacemaker current (If) and Threshold Potential (TP) during 1) sympathetic stimulation and 2) parasympathetic stimulation?
|
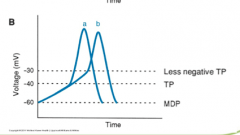
1) Sympathetic stimulation causes increased pacemaker current (If) and brings the TP to a more negative value (Thus will generate an action potential at a more negative potential).
With increased (If) it causes more Na+ to flow into the cell and will depolarize it faster to hit TP sooner thus increase heart rate. Example (Beta adrenergic 1 stimulation) increases HR. 2) Parasympathetic stimulation - Causes a reduction of (If) and thus take longer to depolarize cell to TP. Also increases TP to a more positive (Less negative) threshold so cell needs to depolarize more to fire and action potential. Result: Decreases HR, slower AP formations. In diagram A is normal and B is Parasympathetic stimulation |
|
|
In regards to a Pacemaker cells that has a Cardiac Myocyte as a neighbour what will the electrical effect be on 1) The Pacemaker cell 2) The Myocyte
|
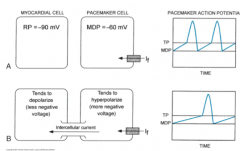
1) The Pacemaker cells will become hyper-polarized (taking negative charge from the myocyte which has a lower resting membrane potential)
2) The myocyte will become more depolarized as it takes charge from the less negative pacemaker cell. Note: Because they are neighbours they have gap junctions which allow ion (electric) travel between the cells. Thus pacemaker cells NOT neighbouring with myocytes tend set the pace because will not have the hyper-polarization effect and can hit their TP earlier and generate the action potential …… Clear as mud. |
|
|
For a patient who has a fixed conduction block a common way to correct conduction is to insert an electrical by-pass tract to conduct the signal pass the blockage area.
What artifact would you pick up on an ECG in a patient with this by-pass tract? Note: By-pass tract can also be called an accessory pathway |

A Delta Wave at start of QRS complex!
|

