![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
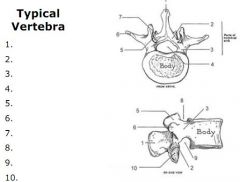
1. Spinous process
2. Lamina 3. Pedicle 4. Vertebral foramen 5. Superior articular facet 6. Transverse process 7. Inferior articular facet 8. Superior notch (foramen for spinal nerves) 9. Inferior notch (foramen for spinal nerves) 10. Same as 7 |
|
|
Which part of bone is more prone to the loss of sex hormones characteristic in osteoporosis, and why?
|
The trabeculae have a much higher turn over and so are more susceptible to weakening than the cortical bone
|
|
|
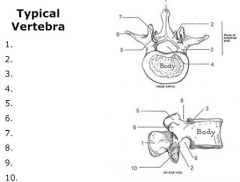
What are the two functions of the lamina?
|
|
|
|
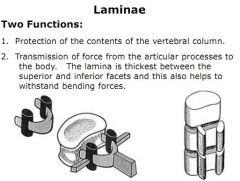
List 4 features distinguishing a cervical vertebrae from any other.
|
1. Small transverse processes with tubercles providing attachments for scalene muscles
2. Foramen transversarium for cervical arteries and veins 3. Bifid spine on all bar C7 4. Slightly curved bodies with neurocentral articulations |
|
|
What feature is prominent on the second cervical vertebrae?
|
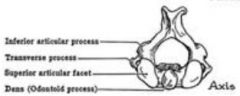
The odontoid process (dens)
|
|
|
What is a key feature of the thoracic vertebrae which others cannot boast, and how do these features vary from T1-12?
|
Articulations with the ribs.
T1-10 has 2 articulations with the vertebral body, and 1 with the transverse process T11 and 12 has 1 articulation with the body, and 1 with the transverse process |
|
|
How could you distinguish a lumbar vertebrae?
|
Negatively. No foramen transversarium and no articulations with ribs.
|
|
|
What passes through the pelvic sacral foramen?
|
Anterior rami of sacral plexus
|
|
|
Roughly describe the degrees of movement available in spine in flexion/extension, lateral flexion and rotation, assigning movement to particular areas where relevant.
|
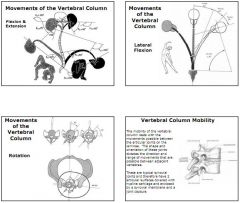
Flexion (forward) - involves lumbar (60⁰) thoracic (105⁰) and cervical (40⁰)
Extension (back) - involves lumbar (35⁰) and cervical (60⁰) only Lateral - involves lumbar (20⁰), thoracic (20⁰) and cervical (35⁰) Rotation - involves thoracic (35⁰), cervical (50⁰) and head (10⁰) Remember - thoracic not involved in extension, and lumbar not involved in rotation. Factors affecting mobility related to orientation and shape of articular facets making up the synovial joints. |
|
|
What is a key feature of the thoracic vertebrae which others cannot boast, and how do these features vary from T1-12?
|
Articulations with the ribs.
T1-10 has 2 articulations with the vertebral body, and 1 with the transverse process T11 and 12 has 1 articulation with the body, and 1 with the transverse process |
|
|
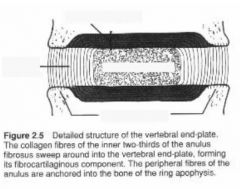
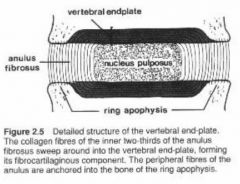
Describe the three components of vertebral discs and explain how they receive nutrients. Explain 'creep' and morning stiffness.
|
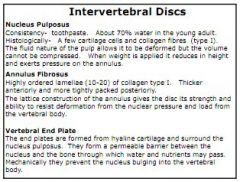
1. Nucleus pulposus - Liquid aspect, deformable but not compressable
2. Annular fibrosus - Proteoglycans and type 1 collagen fibres, controls deformity by mediating forces. Fibres arranged in different orientations. 3. Outer vertebral end plate of hyaline cartilage, permeable to allow passage for nutrients. No blood supply to the disc, so nutrients and waste moved when compression drives fluid out, and at rest when fluid is taken up. 'Creep' is the slow loss of fluid during continuous compression. Morning stiffness due to compression driving out fluid accumulated in the joints at night. |
|

What are the three main ligaments of the spinal cord? Describe their attachments and fibres.
|
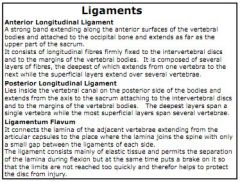
1. Anterior longitudinal - lies against the vertebral bodies and is wide. Superficial fibres are long, covering 2-3 segments, deep fibres are short.
2. Posterior longitudinal - lies in the vertebral column, against the posterior surface of the vertebral bodies. Is narrow. Also has superficial and deep fibres. 3. Ligamentum flavum - lies between the laminae and the articular capsules of the neighbouring vertebra. Contains lots of elastin. Also note the supraspinous ligaments at the tip of the vertebral spines, and the intertransverse ligamanets between the transverse processes (especially in the lumbar region). |
|
|
|
|
|
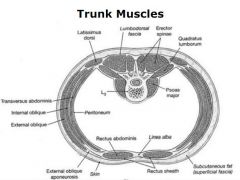
Name the superficial or extrinsic, intermediate and deep posterior trunk muscles.
|
Extrinsic (superficial);
Trapezius Latissimus dorsi Serratus posterior Intermediate; Erector spinae, consisting of Spinalis (2-3 segments) Longissimus (6 segments) Iliocostalis Deep; Transverso-spinae: Rotatores Mutifidus Semispinalis |
|
|
What important anatomical feature helps transverso-spinalis and the capitus and cervicus muscles play a key role in movement?
|
Full of proprioceptive fibres, which allow complex movements to follow a simple movement of the neck.
|
|
|
Describe how the exit of spinal nerves changes down the vertebral column and why this happens. Know where the spinal cord ends.
|
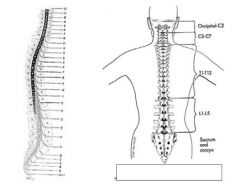
C1-7 exit roughly horizontally
C8 onwards go increasingly vertical Spinal cord ends at L1/2, corda equina carries spinal nerves down below this. |
|
|
What 3 changes occur to the vertebrae as you go down the column?
|
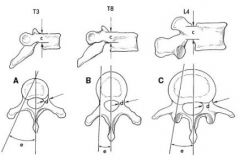
Firstly the vertebrae get bigger as you go down, to take greater load.
The pedicle region gets thicker. The angle to the transverse processes gets larger too. |
|

What is this fracture, how would it be caused and how would you treat it typically?
|
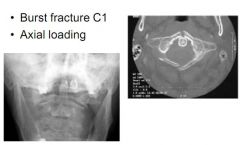
A Jefferson fracture is a C1 burst, due to axial load (falling on head).
It is typically stable if there is no displacement, so would be treated conservatively with a brace. |
|
|
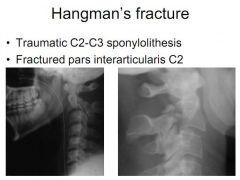
What is a Hangman's fracture classically?
|
|
|

What is this fracture and which is the most difficult to treat?
|

An Odontoid Peg fracture. Type 2 in the middle is the hardest to treat if displaced.
|
|

What is this lower neck fracture known as?
|
Clay Shovellers.
|
|
|
Briefly describe a unilateral facet joint dislocation.
|
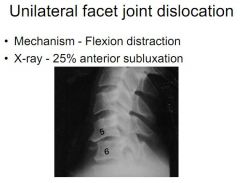
Caused by flexion distraction and presenting with 25% anterior subluxation
|
|
|
Describe a bilateral facet joint dislocation.
|
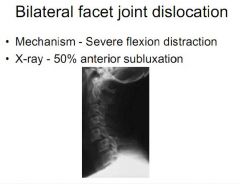
Also caused by flexion distraction, presenting with 50% anterior subluxation.
|
|
|
What are the two types of compression fractures and what might cause them?
|
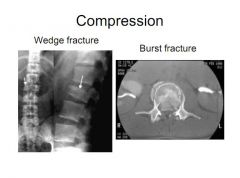
Wedge fracture, common in osteoporosis, with a compression of one aspect of the disc causing a wedge shape.
Burst fracture more common with compression force, can cause displacement. |
|
|
Describe a management course for a suspected neck trauma patient.
|
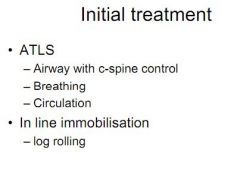
Advance Trauma Life Support
1. Airway with c-spine 2. Breathing 3. Circulation 4. In-line immobilisation, log roll 5. Palpate on log roll 6. Neuro assessment |
|
|
Describe some tests to assess neurological function.
|
C5 - shoulder abduction
C6 - arm flexion/wrist extension C7 - wrist flexion/finger extension C8 - finger flexion T1 - finger abduction L1/2 - thigh abduction L3/4 - knee extension L5/S1 - knee flexion L5 - hallux extension S1 - hallux flexion |
|
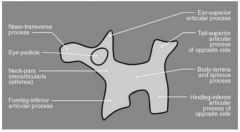
Describe how Scotty Dog can be used in neck trauma.
|

If Scotty Dog can be drawn, the area is intact. The various aspects indicate where a problem may be if Scotty Dog cannot be drawn.
|
|
|
What is Denis' classification?
|
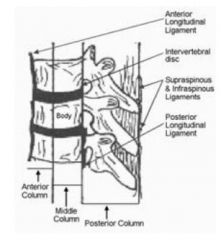
Divides the spine into three sections:
1. The anterior column features the anterior half of the body of the vertebrae 2. The middle column features the posterior half of the body of the vertebrae 3. The posterior column features the spinous processes, ligaments, laminae and posterior articulations. |
|
|
Define a stable injury and indicate management.
|

Conservative management with a collar/halo traction if potentially unstable
|
|
|
Define an unstable injury, and indicate management.
|
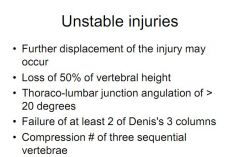
Management with surgery to fuse or fix vertebrae
|
|
|
Describe the development of the spine in terms of curvatures.
|
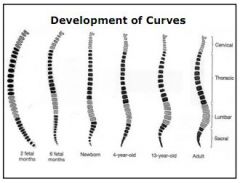
Begins with a kyphosis in the womb, developing with a small lordosis in the cervical region and another at the lumber region at birth.
By adulthood, you have a cervical and lumber lordosis, and a thoracic kyphosis. |
|
|
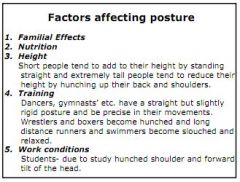
What factors affect posture?
|
|
|
|
Describe some of the issues with a forward and backward tilted pelvis.
|
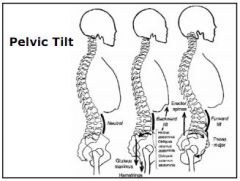
Forward - enhanced lumbar lordosis, weakened abdominals, tight erector spinae and psoas major.
Backward - shortened glutes and hamstrings, stretched and weakened abdominals |
|
|
Which muscles help to maintain good posture?
|
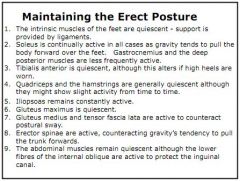
Quiescent:
Feet, Gastrocnemius, Tib Ant, Qauds and Hammy, Glut Max, Abdo Active: Ligs in feet, Soleus, Iliopsoas, Glut Med and TFL, Erector Spinae and Internal Oblique |
|
|
What is postural sway and when it is more pronounced?
|
Constant shifting of centre of gravity and activation and inactivation of muscles to maintain posture.
More prominent in the young and old and when eyes are shut. |
|
|
Distinguish flat back, hollow back and sway back and give their causes.
|

Flat - lost lumbar lordosis, knees flexed when standing
Hollow - increased lumbar lordosis due to large abdomen and flexed hips. Weight on heels. Sway - increased lumbar lordosis due to increased pelvic tilt, knees back and tensed hard. Most common. |
|
|
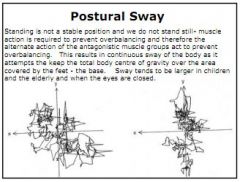
Describe the mechanisms used to help support the body during locomotion.
|
Erectness of trunk achieved by erector spinae, external and internal oblique and the gluteus medius and minimis
Bone strength from trabecular pattern (compromised post menopause by loss of oestrogen) Menisci in the knee joint The valgus angle of the hip moves the knee in to the centre of gravity and help it straighten The arches in the feet help transfer weight from static to dynamic phases |
|
|
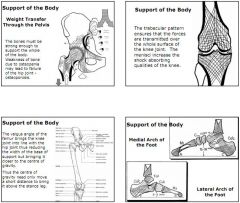
Describe the phases of the gait cycle.
|
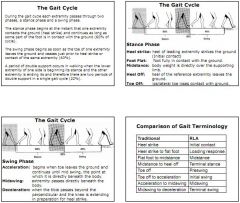
Stance phase:
Heel strike Foot flat Midstance, body weight over the foot Heel off Toe off Swing phase: Acceleration Midswing Deceleration |
|
|
What are some of the ways in which the gait cycle can be measured?
|
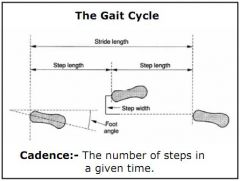
Time and distance:
Cadence Stride length (x2 steps) Step length (x1 step) Step width Foot angle |
|
|
Describe how the body moves during the gait cycle.
|

The body moves forwards throughout, but fastest during double support
The trunk twists as the arms swing in an opposite direction to the legs The trunk also rises and falls approx 50mm, highest at midstance or midswing |
|
|
Describe the actions of the hip, knee and ankle joints during a stance phase
|
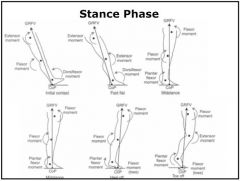
At heel strike the hip is flexed, the knee extended and the ankle dorsiflexed with toe off ground
As the leg moves to floot flat, the ankle plantarflexes till the foot is flat, the knee remains extended, the hip begins to extend At midstance, the hip is neutral, the knee is extended and the ankle begins plantarflexion At heel off, the hip is still extending, the knee is beginning to flex and the ankle is in plantarflexion At toe off, the hip is extended, the knee is flexed, and the ankle is still plantarflexing |
|
|
Describe the degree of rotation required in the hip, knee and ankle joints during the swing phase.
|

The hip flexes 30⁰ and the knee 60⁰
|
|
|
List the action of the various muscles during the gait cycle.
|
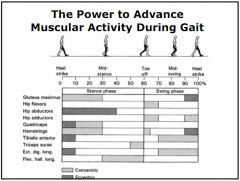
Heel strike:
Hip abductors, Quads, Hamstrings, Tibialis Anterior and Extensor Dig Longus Midstance: Hip abductors, Flexor Halluces Longus Toe off: Hamstrings, Hip adductors, Hip flexors Heel strike: Gluteus maximus, hip adductors, hamstrings, Tibialis anterior and extensor digitorum longus |
|
|
What changes would you expect to see in the gait of a young baby, and an elderly person?
|
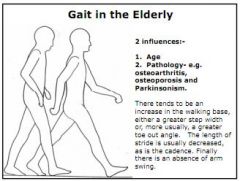
Young baby: Wider base, flat foot, extended knees, no arm swinging, external rotation, quicker cadence
Elderly person: Greater toe out angle (normally 7⁰), shorter stride, slower cadence, no arm swing |
|
|
How does gait alter on stairs and in running?
|

On stairs, instead of a heel strike you land on the anterior portion of the foot. There is a 'pull up' phase, with the knee extensors holding weight and all joints flexed. Then the ankle plantarflexors drive through midstance and toe off.
In running there is no double support, a much longer 'flight phase' and Ground Reaction Force is around 250% of body weight, compared to 70-120% in normal walking. |
|
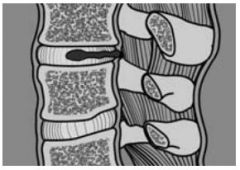
What has happened here?
|
Herniation of the Nucleus Palposus due to weakness in Annular fibrosus
|
|
|
What is a typical site for a spondylolisthesis and how is it treated?
|
L4/5. Usually treated with a screw fix.
|
|
|
How would you test the extensor halluces longus and what would it tell you?
|
Push against big toe and ask patient to dorsiflex.
This tests the anterior rami of L5/S1 |
|
|
Where do the nerves of the cauda equina arise, and what is cauda equina syndrome and what is it's classic symptom?
|
Cauda equina arises at L1-5 and S1-5.
With CES you classically get 'saddle anaesthesia' - bladder and bowel dysfunction when sat down on a saddle of a bike or horse |
|
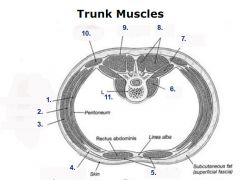
Label the bits
|
|
|
|
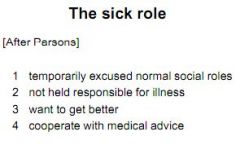
What is the sick role?
|
|

