![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
In the fasted state, what happens with glucagon?
|
Goes up.
|
|
|
In the fasted state, what happens with epinephrine?
|
Goes up.
|
|
|
In the fasted state what happens with insulin?
|
Decreases
|
|
|
Triglyceride breakdown requires the stimulation from what molecules?
|
Glucagon
Epinephrine |
|
|
What are the generalized sequence of events that occurs with triglyceride breakdown?
|
1. Intracellular cAMP INCREASES and ACTIVATES protein kinase A.
2. Phosphorylation and activation of hormone sensitive lipase. 3. Degradation of triglyceride to free fatty acids and glycerol. |
|
|
Post degradation of triglycerides, what happens to FFA and glycerol in the fasted state?
|
Both will diffuse into blood, where FFA will bind to serum albumin. Glycerol is soluble.
|
|
|
In the liver, glucagon and epinephrine stimulate WHAT to form WHAT products for what process?
|
Beta Oxidation
Ketones and Glycerol Gluconeogenesis |
|
|
What must happen for hormone sensitive lipase to act?
|
Phosphorylation of perilipin
|
|
|
What is perilipin?
|
Protein that coats the lipid droplets in adipocytes
|
|
|
What happens to the majority of the FFA that are mobilized from adipocytes to be taken up by the liver?
|
In the liver, 60% of FFA is repackaged into lipoproteins and sent back to the adipocytes
|
|
|
Glycerol
|
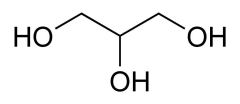
What is this?
|
|
|
Addition of each fatty acid on a glycerol requires what kind of energy expenditure?
|
Two high energy bonds (total of 6 ATP)
|
|
|
T/F - In the fasted state, adipose release just enough FFA for metabolism.
|
F - In the fasted state, adipose releases more FFA than is needed for metabolism.
|
|
|
Describe the actions oof the liver with extra FFA in the fasted state. x 3
|
1. Liver RE-ESTERIFIES the fatty acids into triglycerides.
2. PACKAGES the lipid into lipid protein. 3. SECRETES it into bloodstream. |
|
|
Repackaging FFA ensures what two things?
|
1. Adequate energy supply
2. Homeostasis of serum lipids in blood |
|
|
Describe the steps in fatty acid transport to mitochondria. x 4
|
1. Formation of fatty acy-CoA.
2. Transfer to carnitine to form fatty acyl-carnitine 3. Facilitated diffusion via acyl-carnitine/carnitine transporter. 4. Transfer back to CoA inside mitochondria. |
|
|
Where would you find Carnitine Acyltransferase I?
|
On the cytoplasmic face of mitochondria.
|
|
|
Where would you find Carnitine Acyltransferase II?
|
Inside the mitochondria.
|
|
|
What is the overall point in transferring fatty acid to mitochondria?
|
To degrade the long fatty acyl-CoA in to Acetyl CoA. Then, feed Acetyl-CoA into the TCA and make ATP in ETC
|
|
|
Usually, Beta oxidation of 1 saturated FFA molecule will produce how many Acetyl-CoA's?
|
Eight
|
|
|
Usually, Beta oxidation of 1 saturated FFA molecule will lead to how many CO2's?
|
16 CO2
|
|
|
Usually, Beta oxidation of 1 saturated FFA molecule will lead to how many electrons?
|
64 e-
|
|
|
What is the major point of beta oxidation?
|
Fatty acids get cleaved to make Acetyl-CoA
|
|
|
What is needed for beta oxidation of monoUNSATURATED fatty acid?
|
An isomerase to convert the cis bond to trans.
|
|
|
What is needed for beta oxidation of polyUNSATURATED fatty acid?
|
Need a reductase and an isomerase.
|
|
|
"When life gives you propionyl-CoA, make".....what?
|
A TCA intermediate (Succinyl CoA)
|
|
|
When do you get the three carbon molecule, propionyl CoA?
|
It is the final product in odd-chain fatty acids.
|
|
|
How does biotin play a role in odd chain FA beta oxidation?
|
Takes propionyl-CoA and converts it a four carbon intermediate via carboxylation.
|
|
|
Under low glucose levels, the brain uses what for food?
|
ketones
|
|
|
Which ketone is responsible for bad breath?
|
acetone
|
|
|
Ketones are produced from what molecule and where specifically?
|
Acetyl CoA
Hepatocyte mitochondria |
|
|
Describe the general steps in ketone formation in the liver during a fasted state.
|
1. Gluconeogenesis removes oxaloacetate from TCA.
2. Oxaloacetate removal SLOWS down TCA causing accumulation of acetyl-CoA. 3. Acetyl-CoA is then used to make ketones. |
|
|
Loss of insulin in IDDM patients, is due to a loss of what and where?
|
Beta cells in the pancreas.
|
|
|
Accumulation of ketones in blood can lead to what?
|
ketoacidosis
|
|
|
Ketoacidosis can alter what?
|
Heme functions
Oxygen transport |
|
|
What are the presentations of Carnitine deficiency? x 4
|
1. Hypoketotic Hypoglycemic Encephalopathy.
2. Cardiomyopathy 3. Myopathy 4. GI Dysmotility |
|
|
What parts are effected by Carnitine deficiency? x 3
|
1. CNS
2. Skeletal muscle 3. Cardiac muscle |
|
|
B12 Deficiency causes an accumulation of what molecules? x2
|
Methylmalonyl-CoA
Homocyteine 5-MethylTHF |
|
|
B12 deficiency can cause the same kind of anemia as what other disorders? x2
|
1. Oroticaciduria I
2. Oroticaciduria II |
|
|
Acyl CoA Dehydrogenase deficiency affects what enzymes? x3 from worst symptoms to least.
|
1. VLCAD (Very Long Chain Acyl CoA Dehydrogenase)
2. MCAD (Medium Chain Acyl CoA Dehydrogenase) 3. SCAD (Short Chain Acyl CoA Dehydrogenase) |

