![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
|
Major forms of cancer treatment |
-Surgery -Radiotherapy -Chemotherapy |
|
|
Advantages/Disadvantages of Chemotherapy |
Advantages Able to eliminate micrometastases away from site of origin
Disadvantages -Lacks selective toxicity: cytotoxic to normal cells, especially those undergoing rapid proliferation Bone marrow, lymphoid system, hair roots, oral and GI epithelia, skin |
|
|
General toxic side effects of anti-cancer drugs |
-Suppresses bone marrow and immune system -Causes nausea and vomiting -Oral and GI ulceration, and diarrhoea -Hair fall out (alopecia) -Germ cells --> sterility/teratogenicity? -potential carcinogen |
|
|
Principle of Cell Kill |
1. AC drugs kill cells according to first order kinetics -A given dose kills a constant fraction of cells (repeated half-lives)
2. For most drugs, dose is proportional to cell kill I.e. the higher the dose, the greater the log cell kill |
|
|
Log cell kill |
Log kill 1 = 90% kill Log kill 2 = 99% Log kill 3 = 99.9% etc.
Minimum useful % kill is log kill 3 (99.9%) |
|
|
Clinical Milestones |
10^13 cells: Death (10kg tumour cells) 10^12 cells: Advanced disease 10^9 cells: 1 g tumour (minimum detectable) 10^6 cells: 1mg tumour (not detectable; clinical recovery) 10^3 cells --> 10^0 cells: chemotherapy must be maintained well after clinical recovery, or relapse will occur |
|
|
Actual vs. Theoretical Cell Kill |
-Theoretically should be straight downward slope -In reality, slope is much less and cell kill is jagged (has ups and downs) |
|
|
Reasons for lesser cell kill |
Toxicity Due to bone marrow suppression, treatment may have to be delayed to allow RBC count recovery
Drug resistance Nearly always develops (intrinsic or acquired)
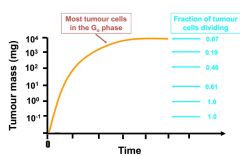
Tumour growth characteristics -Constant log cell kill obtained with population of biochemically homogeneous cells -Solid tumour is a mixture of 2 main cell types: actively dividing cells, and quiescent cells (Go) |
|
|
Gompertzian Tumour Growth Curve |
|
|
|
AC Drugs: Action During the Cell Cycle
Cell-Cycle Specific (CCS) Agents |
-Act during a specific phase of cell cycle -Go cells appear to be unaffected
Antimetabolites: Methotrexate Antimicrotubules: vinca alkaloids Podophyllin alkaloids: etopside |
|
|
AC Drugs: Action During the Cell Cycle
Cell-Cycle Nonspecific (CCNS) Agents |
-Kill both dividing and Go cells but dividing cells usually more sensitive
Alkylating agents: cyclophosphamide Anthracycline antibiotics: doxorubicin Platinum drugs |
|
|
AC Drugs: Mechanism of Action
Alkylating Agents |
E.g. cyclophosphamide, platinum drugs
-Act by transferring alkyl groups to cellular constituents such as DNA, RNA and protein |
|
|
AC Drugs: Mechanism of Action
Antimetabolites |
E.g. methotrexate
-Inhibits DNA synthesis: similar structure to endogenous molecules (folates, purines and pyrimidines) required for nucleic acid synthesis |
|
|
AC Drugs: Mechanism of Action
Toposiomerase Interactive |
E.g. etopside
-Induces DNA damage by inhibiting topoisomerase action: nuclear proteins responsible for DNA's topology |
|
|
AC Drugs: Mechanism of Action
Antimicrotubule Drugs |
E.g. vincristine
-Induces metaphase arrest by disrupting microtubules and mitotic spindle |
|
|
AC Drugs: Mechanism of Action
Hormonal Agents |
E.g. anti-oestrogens for breast cancer, anti-androgens for prostate cancer
-Less toxic than other drugs |
|
|
AC Drugs: Mechanism of Action
Targeted Therapies |
E.g. Transtuzumab (Herceptin) for HER-2 positive breast cancer
-Targets specific molecules involved in cancer progression |
|
|
Mechanisms of Resistance |
1. Enhanced expression or alteration of target -Methotrexate and dihydrofolate reductase
2. Increased production of glutathione (GSH)- inactivates the drug and aids in elimination Alkylating agents, platinum drugs
3. Increased repair capacity DNA damage Alkylating agents, platinum drugs
4. Increased expression of P-glycoprotein efflux pump -Pumps drugs out of cell -Multidrug resistance: vinca alkaloids, taxanes, anthracyclines |
|
|
Combination Chemotherapy |
-Overcomes resistance
1.) Must be active alone against the tumour
2.) Must have differing mechanisms of action
3.) Should have different toxicity profiles if possible
4.) Use maximum tolerated dose at the outset- initial aggressive therapy |
|
|
Chemotherapy Indications |
-Readily curable: testicular cancer (85%), Hodgkin's disease (85%), etc.
-After surgery and radiotherapy: micrometastatic disease in other organs may be eradicated; may enhance local killing by radiotherapy
-Pallation: Cure may not be possible, but may improve survival symptoms |

