![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
80 Cards in this Set
- Front
- Back
|
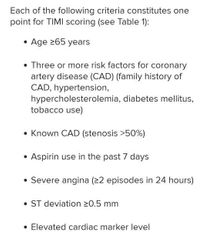
TIMI score |
|
|
|
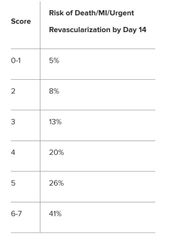
TIMI score interpretation |
|
|
|
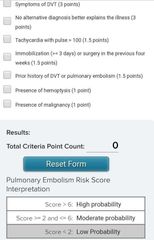
Pulmonary embolism Wells score |
|
|
|
Ferrous sulphate elemental iron content |
65mg (dried) 60mg |
|
|
Ferrous gluconate elemental iron content |
35mg |
|
|
Ferrous fumarate |
65mg |
|
|
Risk assessment according to dose for iron toxicity |
<20mg/kg - asymptomatic 20-60mg/kg - GI symptoms only 60-120mg/kg - potential for systemic toxicity >120mg/kg - potentially lethal |
|
|
Indications for desferrioxamine in iron poisoning |
Iron levels > 90 micromol/L at 4-6 hours
Shock Severe metabolic acidosis Altered mentation Signs of systemic toxicity |
|
|
How do you work out the amount of elemental iron ingested? |
•ferrous sulfate (dried) — divide dose by 3.3 •ferrous sulfate (heptahydrate) — divide dose by 5 •ferrous gluconate — divide dose by 9 •ferous fumarate — divide dose by 3 •ferric chloride — divide dose by 3.5 •ferrous chloride — divide dose by 4 |
|
|
What is the desferrioxamine test? |
Collect urine, put into specimen container and keep. Give a dose of desferioxamine IMI. a few hours later, collect another specimen of urine and compare to the first. If it has become red/pink, then your test is positive and the patient has ingested a large amount or iron and needs to be treated. |
|
|
What is an aura? (migraine) |
Neurological deficit within 1 hour of onset of headache - usually last 5-20 minutes. Mostly visual disturbances "fortification spectra" (zig zag lines that gradually spread from peripheral to central vision) |
|
|
Acute management of migraines |
Paracetamol 1g 4-6-hourly or Aspirin 1000mg + Metoclopramide 10mg Not opiates - will worsen |
|
|
Migraines prophylaxis |
1. Sodium valproate 2. Propanalol 3. Topiromate 4. Amitryptiline 5. Tryptans - not available here |
|
|
Management of tension headaches |
Amitryptiline 10-75mg nocte |
|
|
Abortive management of cluster headaches |
Inject sumatriptan or 100% oxygen |
|
|
Prophylactic management of cluster headaches |
Verapamil (calcium channel blocker) Prednisone Lamotrigine |
|
|
Initial investigation in GCA |
ESR |
|
|
4 prerequisites to diagnose idiopathic intracranial hypertension |
1. Clinical features only due to raised ICP 2. No focal neurology 3. CT - no mass or ventricular obstruction 4. Normal CSF |
|
|
Management of idiopathic intracranial hypertension |
Monitor vision and visual fields If change, need surgery to shunt CSF or just decompress the optic nerve sheath If no change, could do repeat LPs, drugs (steroids, acetazolamide, furosemide) or surgery to shunt |
|
|
Why is a headache from a SOL worse on waking? |
High ICP due to recumbency High carbon dioxide due to respiratory depression Decreased CSF absorption at night |
|
|
Clinical features of hypernatraemia |
Fatigue Headache Nausea and vomiting Confusion Seizures Coma |
|
|
Dominant hemisphere cortical lesions |
Dysphasias Nominal dysphasia Dyslexia Dysgraphia Dyscalculia Agnosia (ask to write something) |
|
|
Non-dominant hemisphere cortical lesions |
Geographical agnosia Dressing apraxia Contructional apraxia Hemi-neglect |
|
|
Cerebellar dysfunction - damage to midline structures (vermis) |
Disturbance of equilibrium with unsteadiness on standing, walking, sitting (truncal ataxia) Broad-based, reeling gait Eye closure does not affect balance (negative Romberg) Vestibular tests may be impaired |
|
|
Cerebellar dysfunction - damage to hemispheric structures |
Ipsilateral impaired limb coordination Ataxia - gait unsteady towards the sign of the lesion Dysmetria - finger nose Dysdiadokinesia Intention tremor Rebound phenomenon - outstretched arm swings excessively when displaces Pendular reflexes - leg swings back and forth when knee jerk |
|
|
Cerebellar dysfunction - affecting cerebellar connections to vestibular nuclei |
Nystagmus |
|
|
Symptoms of anaemia |
General - weakness, lethargy, visual disturbances (severe can get retinal haemorrhages) CVS - palpitations, chest pain, heart failure, intermittent claudication Resp - SOB |
|
|
Clinical signs of anaemia |
General - conjunctival pallor, tachycardia, bounding pulses, floe murmurs, cardiac failure Iron-def - koilonychia Haemolytic, megaloblastic - jaundice Chronic haemolysis - splenomegaly Sickle cell - leg ulcers Megaloblastic - loss of proprioception and vibration Thalassemia - bone deformities like maxillary hyperplasia |
|
|
Pencil cells |
Iron-deficiency anaemia |
|
|
Spherocytes on blood film |
AIHA Hereditary spherocytosis |
|
|
Target cells on blood film |
Liver disease Haemoglobinopathies |
|
|
Tear drop cells on blood film |
Bone marrow infiltration Fibrosis |
|
|
Polychromasia |
Reticulocytosis |
|
|
Investigations to consider in anaemia |
FBC Blood film Reticulocyte count Haemolytic screen - unconjugated bilirubin, haptoglobin, LDH, Coombs Hb studies - electrophoresis BM biopsy Iron studies, B12 and folate Parvovirus PCR |
|
|
IV iron |
Venofir - give multiple doses over a few weeks Cosmofer - replace iron stores completely, watch for anaphylaxis |
|
|
Anaemia + dementia |
Think about B12 deficiency Often with jaundice - big cells haemolyse in bone marrow |
|
|
Causes of B12 deficiency |
Vegan diet Malabsorption - terminal ileum issue (Crohns, UC, colectomy, iliectomy) - stomach (not enough IF, gastrectomy, chronic gastritis so no parietal cells, pernicious anaemia = autoantibodies against intrinsic factor) - elderly (polypharmacy) |
|
|
Anaemia, jaundice, splenomegaly |
Think haemolysis - sudden Hb drop with no bleeding |
|
|
SLICC clinical criteria for SLE |
Need 4/17 criteria, at least one clinical and one immunological OR biopsy-proven lupus 1. Acute cutaneous lupus - malar rash, bullous, TEN, maculopapular, photosensitive OR subacute cutaneous lupus - nonindurated psoriaform and/or annular polycyclic lesions that resolve without scarring 2. Chronic cutaneous lupus - classic discos rash, localised (above neck), generalised (below neck), hypertrophic (verrucous), panniculitis, mucosal OR discoid lupus/lichen plans overlap 3. Non-scarring alopecia 4. Oral or Nasal ulcers 5. Joint disease - synovitis involving two or more joints OR tenderness in two or more joints with at least 3o minutes of morning stiffness 6. Serositis - pleurisy for more than one day, pleural effusions, pleural rub OR typical pericardial pain for more than one day, pericardial effusion, pericardial rub, pericarditis 7. Renal - UPCR > 0.5 OR RBC casts 8. Neurological - seizures, psychosis, mononeuritis multiplex, myelitis, peripheral or cranial neuropathy OR acute confusional state 9. Haemolytic anaemia 10. Leukopaenia OR lymphopaenia 11. Thrombocytopaenia |
|
|
SLICC lab criteria for SLE |
1. ANA + 2. Anti-ds DNA + 3. Anti-Sm + 4. Antiphospholipid Ab + 5. Low complement (low C3 and C4) 6. Direct Coombs positive (with no Haemolytic anaemia) |
|
|
What is the commonest cause of erythema nodosum? |
Sarcoidosis |
|
|
Anion gap |
Na - (Cl + HCO3) Normal 7-13 |
|
|
Osmolar gap |
Osmolality (measured) - osmolality (calculated) Normal <10 |
|
|
Serum osmolality |
2(Na + K) + glucose + urea |
|
|
Brown-Sequard |
Hemicord syndrome Ipsilateral UMN lesion, position and vibration loss Contralateral pain and temperature loss Caused by stab wound |
|
|
LMN lesion in nucleus + loss of pain and temperature bilaterally |

Anterior cord syndrome Caused by anterior spinal artery occlusion |
|
|
Central cord syndrome |
Preserved position, vibration, touch Loss of pain, temperature in affected dermatomes Caused by syringomyelia (cyst in spinal cord), neoplasm |
|
|
Tabes dorsalis |
Wasting of posterior column secondary to demyelination and atrophy of posterior roots of spinal nerve Tertiary syphilis |
|
|
What does vitamin B12 deficiency affect in the spinal cord? |
Posterior columns Pyramidal tracts With dementia, peripheral polyneuropathy, subacute combined degeneration of the cord |
|
|
Features of delirium |
Acute Fluctuating - agitated at night, drowsy during the day Rapid functional decline Poor attention/concentration Disorientated to place and time Cannot interpret sensory stimuli (cannot decipher at the hospital) May have hallucinations but more often illusions Tremor and myoclonus in severe encephalopathy |
|
|
Tender hepatomegaly |
Viral Hepatitis Congestion Budd chiari Abscess Primary sclerosing cholangitis HCC |
|
|
Pulsatile liver |
TR HCC (venous hum) |
|
|
Irregular hepatomegaly |
HCC Early cirrhosis |
|
|
Stigmata of chronic liver disease |
Palmar erythema Dupytren's contracture Gynaecomastia Spider naevi Testicular atrophy |
|
|
How do LFTs look in alcoholic liver disease? |
Raised GGT Reverse ratio AST raised more than ALT (2:1 ratio) |
|
|
Outline management of cirrhosis |
Ascites - restrict sodium, diurese with spiro and lasix, give albumin whenever get rid of >5L, paracentesis Encephalopathy - restrict protein, lactulose Infections - vaccinate Bleeding varices - do endoscopy, maybe band, or carvedilol (12.5mg BD for C-P A, 6.25mg BD for C-P B or C) Avoid NSAIDs and ACE-Is |
|
|
Which drugs cause thyrotoxicosis? |
Lithium Amiodarine |
|
|
Who gets toxic multinodular goitr? |
Elderly Iodine deficient |
|
|
Thyroid acropachy |
Clubbing Painful finger and toe swelling Periosteal reaction in limb bones Graves disease |
|
|
What is the major side effect of carbimazole? |
Agranulocytosis - take infection very seriously |
|
|
DDx diffusely enlarged goitre |
Physiological Graves Hashimoto thyroiditis Subacute thyroiditis (de Quervain - painful) |
|
|
Nodular goitre |
Multinodular goitre Adenoma Carcinoma |
|
|
When should you consider investigating Conns? |
Hypertension with hypokalaemia (RAS is more likely, though) Refractory hypertension despite >2 drugs Hypertension <40, especially in women |
|
|
DKA triggers |
Infection Non-adherence MI Drugs - chemo, anti-psychotics Pancreatitis Surgery |
|
|
What is always present in motor neuron disease? |
Fasciculations Otherwise mixed UMN and LMN signs |
|
|
Approach to peripheral neuropathy |
Infectious - HIV, GBS Autoimmune - SLE Metabolic - diabetes, B12 deficiency, amyloidosis, chronic kidney disease Idiopathic Neoplasm - lung Ca (paraneoplastic), chemotherapy Drugs - INH, alcohol, Amiodarine, nitrofurantoin |
|
|
Pulmonary embolism on ECG |
S wave in lead I Q wave in lead III Inverted T wave in lead III |
|
|
Mechanism of unfractionated heparin |
Potentiate antithrombin III |
|
|
Issues with unfractionated heparin |
No antidote Needs PTT monitoring >5 days, risk heparin-induced thrombocytopaenia |
|
|
Mechanism of LMWH |
Affects factor Xa |
|
|
LMWH antidote |
Protamine sulphate |
|
|
What is a side effect of warfarin? |
Skim sloughing due to inhibition of protein C (prothrombotic) |
|
|
What should you consider when on warfarin and INR is high? |
Drug drug interactions Liver dysfunction Overdose Genetic predisposition - then need novel or LMWH |
|
|
Important cause of clostridium difficile |
Ciprofloxacin PPIs Especially together Use vancomycin because metronidazole needs GIT absorption |
|
|
Treatment for Hereditary angio edema |
FFPs |
|
|
HAS-BLED SCORE |
For risk of bleeding in patients taking anticoagulation for AF Hypertension - >160 Abnormal renal function - dialysis, transplant, creatinine >200 Abnormal liver function - cirrhosis or bilirubin >2X normal or AST/ALT>3X normal Stroke Bleeding - major bleeding or predisposition Labile INR - unstable/high Elderly - >65 Drugs - alcohol or drugs, Antiplatelets, NSAIDs |
|
|
Management of haemoptysis |
Get Hb IV line CXR - lie bad lung down (prevent aspiration) Oxygen 2 pinks and 1 yellow Give morphine (4mg) and dormixum (4mg) to suppress the cough |
|
|
Causes of hypoglycaemia in non-diabetic |
Exogenous insulin (measure C-peptide), glimepiride Pancreatitis Liver failure Addison Infection Neoplasm (insulin-secreting) |
|
|
Kussmauls sign |
JVP does not go down during inspiration |
|
|
Wallenberg's syndrome (lateral medullary) |
Crossed signs Ipsilateral cerebellar Ipsilateral Horners Ipsilateral palate and vocal coed weakness Ipsilateral facial sensory loss Contralateral arm and leg sensory loss No UMN weakness |

