![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
158 Cards in this Set
- Front
- Back
|
what kind of virus is influenza?
|
RNA virus (negative, single strand **SEGMENTED**)
helical nucleocapsid has an envelope Virions are pleomorphic |
|
|
what is different about influenza from other viruses?
|
the genome is segmented... 8 segments
each segment has its own RNA |
|
|
Influenza Type A
|
- causes epidemic/pandemic flu in humans
- mutates, and reassorts during passage through humans and animals (birds, pigs, horses, marine mammals). - Also causes seasonal non-epidemic flu by mutational drift, like type B. |
|
|
Influenza Type B
|
- causes non-epidemic seasonal flu.
- Mutates only (antigenic drift). Infects only humans. |
|
|
Influenza Type C
|
- does not cause serious disease in humans.
- Mutates only, and infects only humans. |
|
|
Virus Nomenclature
|
- Influenza type
- Species isolated form (unless human) - Place of Isolation - Strain designation - Year isolation - H#N# subtypes Example: A/Hong Kong/1/68(H3N2) |
|
|
Hemagglutinin
|
- Binds to sialic acid on cells for entry
- Mediates binding and entry into cells - Hemagglutinates red blood cells - diagnosis - Elicits protective antibodies that neutralize the virus - H1, H2, etc. are the different forms of HA that represent antigenic shift - Minor mutation result in antigenic drift that makes new strains each season |
|
|
Neuraminidase
|
- Cleaves sialic acid, which allows virus to be released from cells
- Target of antiviral drugs zanamivir (Relenza) and oseltamiver (Tamiflu) - N1, N2 represent distinct forms with different antigenicities - Antibodies against N do not neutralize virus, but do reduce virus release --> allows virus to be released from the cell AND prevents them from clumping to one another |
|
|
Flu viruses infect _____________ cells in lower respiratory tract.
|
columnar epithelial
Tracheal mucosal epithelium loses ciliary cells until recovery. This makes you vulnerable to secondary bacterial infections. |
|
|
pathogenesis of influenza
|
- Virus kills the cells it infects.
- Disrupts ciliary action, making patient susceptible to secondary bacterial infections. - Bronchitis and pneumonia can result from influenza directly but usually are the result of secondary infection. - Interferon response induced by dsRNA intermediate. - Virus has mechanisms to counter IFN effects on cells these are partially effective. |
|
|
recovery from the flu
|
- Virus replication is fast, acute, so immune response is dominated by non-specific immunity – interferon.
- Interferon has side effects – fever, myalgia, fatigue, malaise These are many of the symptoms of flu. - Cell mediated immune responses kick in around day 4-5 and are important for recovery, also for producing symptoms due to cytokine effects. - Ab response later - protects from reinfection, but only to same virus. vaccines rely on antibody response. |
|
|
Cytokine Storm
|
- Also referred to as systemic inflammatory response syndrome (SIRS).
- SIRS may explain the devastating nature of the 1918 strain of influenza. - The immune system overreacts toward the pathogen. - Cytokines signal macrophages to travel to the site of infection, causing damage to the body and organ failure. - H5N1 Avian Influenza virus also causes SIRS and is at least 50% lethal in humans. |
|
|
Antigenic Drift
|
A cell infected with 1 virus can only produce viruses identical to the infecting virus, or viruses with point mutations *
|
|
|
Antigenic Shift
|
Reassortment occurs when a cell is infected with >1 different viruses
|
|
|
Laboratory diagnosis of Influenza virus infection
|
- Usually done by noting symptoms, time of year, exposures, etc. rather than a diagnostic test.
- Quick lab tests are available and detect viral antigens, but they are error prone, both false (+) and false (-) results - Viral culture tests can also be performed but take longer |
|
|
Vaccines
|
- Most effective way to prevent influenza (but still get sick... because its ********)
- Flu vaccination time in the U.S. --> October and November - Vaccine grown in eggs - Inactivated trivalent vaccine contains purified HA and NA - Live, attenuated vaccine, LAIV (Licensed in 2003) - LAIV (FluMist®) is approved for use in healthy people 2-49 years of age who are not pregnant. - Given as a nasal spray. |
|
|
Trivalent Vaccine Composition
|
Vaccine is a cocktail of 3 virus strains
2 strains of Influenza A 1 Influenza B strain Recommendations made based on antigenic analyses of recently isolated influenza viruses, epidemiologic data and post-vaccination serologic studies in humans |
|
|
What viruses can cause a common cold?
|
Rhinoviruses - members of the Picornavirus family - the most common cause
Adenoviruses Enteroviruses (also are Picornaviruses) Coronaviruses Parainfluenza viruses **MOSTLY SMALL, NAKED VIRUSES |
|
|
difference between susceptibility to cold and flu
|
Rhinoviruses grow best at a cool 33°C, while influenza virus grows best at warmer temperatures deep in lung.
|
|
|
Cold vs. Flu
|

|
|
|
The common cold causes a release of:
|
histamine - symptoms
IFN - symptoms Mucous - symptoms |
|
|
Rhinovirus blocks ____production:
|
Rhinovirus blocks IFN production:
less IFN symptoms than flu - contrast the mechanisms - Rhinovirus infections are largely controlled by IFN production - Neutralizing antibodies are made weakly, so protection against reinfection is weak. |
|
|
high risk group for the common cold
|
EVERYONE
|
|
|
Enteric viruses
|
Unlike the respiratory tract, which is warm and moist and neutral pH, the digestive tract is more hostile.
|
|
|
Picornaviruses
|
Enteroviruses - spread via fecal-oral route but replicate mainly in lymph nodes
Poliovirus - spreads to neurons in spine and kills them HAV - covered in Hepatitis virus section (Rhinovirus is a picornavirus but it is is not an enteric virus - it’s a respiratory virus) |
|
|
what would normally happen when double stranded RNA is introduced into a cell?
|
treated as foreign and would induce a strong interferon response
|
|
|
how does the rotavirus avoid typical response of the cell to ds-RNA ?
|
genome is protected by 3 capsid layers... so never exposes it to the cell to induce a response
The first capsid layer is removed by intestinal enzymes. Transcription happens in virions and ssRNA is squirted out to cytoplasm. During viral assembly, ssRNA is packaged then turned into dsRNA. This is all designed to hide the dsRNA from the innate immune system to reduce the induction of TNF. |
|
|
why do antibodies come up late in infection in the rotavirus infections?
|
Infected cells die, inducing innate immunity anyway.
Antibodies come up late in infection, and virus is gone by the time they are in full gear. Antibodies mainly provide (incomplete) protection from reinfection. |
|
|
effects of rotavirus
|
causes gastroenteritis (intestinal inflammation, diarrhea), fever, vomitting, mostly in children
Infect intestinal columnar epithelial cells. Stool can contain up to a billion virions per mL - even during asymptomatic infection Virus remains infectious in water. |
|
|
symptoms of hepatitis
|
- inflammation of the liver
- jaundice (yellowing in the skin, eyes caused by bilirubin buildup in the blood) - fatigue - abdominal pain - loss of appetite - nausea & vomiting - darkening of the urine |
|
|
jaundice
|
yellowing in skin, eyes!
caused by buildup of bilirubin in the blood --> a byproduct of hemoglobin metabolism due to liver not liver properly metabolizing and excreting it |
|
|
most cases of viral hepatitis
|
A, B, C > 90% of viral hepatitis
|
|
|
Hepatitis A virus
|
HAV - infectious hepatitis
HBV - serum hepatitis HCV - formerly non-A and non-B hepatitis virus HSV - hepatitis D virus (delta particle) |
|
|
Hep B
|
HAV - infectious hepatitis
HBV - serum hepatitis HCV - formerly non-A and non-B hepatitis virus HSV - hepatitis D virus (delta particle) |
|
|
Hep C
|
HAV - infectious hepatitis
HBV - serum hepatitis HCV - formerly non-A and non-B hepatitis virus HSV - hepatitis D virus (delta particle) |
|
|
Hep D
|
HAV - infectious hepatitis
HBV - serum hepatitis HCV - formerly non-A and non-B hepatitis virus HSV - hepatitis D virus (delta particle) |
|
|
how is hep A different from the others?
|
its the one NAKED VIRUS
|
|
|
which hepatitis is a naked virus?
|
type A
|
|
|
what is special about Hep D
|
requires Hep B to replicate
|
|
|
what types are viruses are the hep viruses
|
HBV is a DNA virus
HAV is a ssRNA virus HCV is a ssRNA virus |
|
|
Hep A
|
- naked picornavirus (+ssRNA genome)
- spread by not washing hands - short incubation period (15-30 days) - will ONLY cause acute hepatitis --> no carrier state (like in hep B) Virus is not lysing the cell leaves the cell through exocytosis (budding off the cell) Therefore, the virus is not pathogenic Damage/pathogenesis is caused via immune response in the body, regulated by T-cell response Virus gets out of the body via the stool |
|
|
HAV Prevention and treatment
|
- hygiene (hand-washing)
- vaccine is 100% effective *Immune serum can also be given as prevention post exposure. |
|
|
Hep B
|
- aka "serum hepatitis" / "long incubation hepatitis"
- ENDEMIC in many developing countries (spread via mothers) - usually from sex, shady tattoo places, dentists (in the old days) - Infection is usually Acute, and your body deals with it and eliminates it - you can also become chronic and the disease becomes persistent hepatitis. - you’ll be a lifelong carrier, shedding the virus throughout life (i.e. during sex) ** 45-80 day incubation period! - chronic infection is similar to Hep A... but with JOINT PAIN Chronic infection can lead to cirrhosis of the liver --> liver cancer - Hepatocellular carcinoma |
|
|
Hepatocellular carcinoma
|
80% caused by Hep B... rest by Hep C
--> Chronic infections/inflammations can lead to cellular DNA damage (hyperproliferation due to cytokine exposure or need to replace dead cells) **alcohol is a risk factor |
|
|
chronic hepatitis
|
> 6 months of liver inflammation... detected by alanine aminotransferase ALT in blood
HBV/HCV releases many virions per day through the liver. -test can be done against the hepatitis antigen in the blood. -chronic infection is characterized by appearance of escape mutants. -alcohol worsens the liver damage |
|
|
how are acute vs chronic hepatitis determined
|
by the original immune response you make
- strong immune response leads to acute hepatitis that is rid of eventually - weakened immune response may lead to a chronic infection and a lifelong carrier (may also have cirrhosis/liver cancer) |
|
|
dane particle
|
infectious Hep B virion
- little ball attached to the immune decoy that contains different capsid layers with the virion inside of it - Outside coat protein may self assemble even without a virion inside --> may form an immune decoy - your body may only form so much antibody, and a lot of it binds only to the immune decoy, leaving the infectious virion intact. |
|
|
how is HBV different from other DNA viruses?
|
not fully double stranded or single stranded DNA
--> finishes its polymerization into double stranded DNA when already in your cell mRNA goes into the cytoplasm, but the mRNA will make both proteins and becomes RT to make RNA - the RNA made by the RT and protein will assemble into a new virion - RT step allows the virus to be vulnerable against some types of meds. |
|
|
vaccine for hep B
|
Vaccine = clone gene for outside coat protein and make yeast/bacteria synthesize it (doesn’t contain the virion but induces antibody response)
- vaccine doesn’t cure you but it would be able to limit the viral load because you get a good immune response (you’re ready) - Vaccine protects against re-exposure but doesn’t prevent sterilizing immunity only prevents the virus from reaching the liver, but it may still replicate |
|
|
Test for active Hep B infection is usually for the
|
HBsAg
|
|
|
HBV replication
|

|
|
|
Recombivax
|
Recombivax vaccine is a subunit vaccine (for Hep B) using recombinant DNA technology to make HBsAg particles.
3 injections and a titer test for antibodies to surface antigen.! |
|
|
Hep B treatment
|
- There are no antivirals for acute infection
- may be that the virus is not using the RT during this step. - RT inhibitors are used for chronic infections (lamivudine) Test for HepB can include the surface antigen (HBsAg). - can be positive in blood even when virus is not actively replicating - antibodies indicate past exposure HBc = hepatitis B virus core antigen (diagnoses acute infection) HBeAG = present only during viremia, when contagious |
|
|
Hepatitis D
|
“delta particle”
- Doesn’t replicate by itself, it piggybacks off Hepatitis-B. - not commonly seen in the industrialized world +ssRNA - relies on enzymes of Hep-B to replicate and the combination of the two makes the disease much worse |
|
|
Hepatitis C
|
NO VACCINE AGAINST C
Flavivirus: +ssRNA virus, enveloped! Mutates very rapidly (RNA virus) --> 6 major serotypes - 80% remain asymptomatic - Most spread is through blood contact rather than through sex or food. - Acute infection with resolution - 15%! - Chronic persistent infection with disease progression - cirrhosis and liver cancer later in life - 70%! - Rapid disease progression - cirrhosis - 15% **damage is predominantly through the immune response by the body (virus is not cytopathic --> lyse the cell & kill it) |
|
|
HCV vs HIV
|
Now more people are killed by HCV than HIV.
|
|
|
HCV Prevention and Treatment
|
**No vaccine for HCV (high mutation rate makes it hard to make one)
Ribavirin + Pegylated Interferon-α Side effects are severe --> cure rate 50% Sofosbuvir (may be used alone or in combination of tx #1) - Inhibits viral RNA polymerase (a chain terminator) - less severe in its side effects than the interferon inhibitor. |
|
|
arboviruses
|
Flavivirus family --> +ssRNA viruses
From Arthropods - Arthropod Borne Virus - mostly from mosquitos sucking blood from viremic people or animals - Virus replicates usually in mosquito salivary gland, then is available to be transmitted to new host |
|
|
Sylvatic (Jungle) Cycle
|
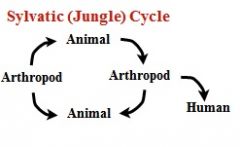
it can stay in the jungle where the cycle can continue, and doesn’t really need a human host
|
|
|
Urban Cycle
|
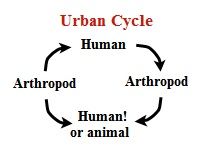
the human is actually part of the chain/cycle
|
|
|
effects of arboviruses
|
- encephalitis
- febrile diseases - hemorrhagic fevers |
|
|
West Nile Virus
|
- arbovirus
- incubation period is 2-14 days - Fever, headaches, stiffness are some of the symptoms - follows bird migratory symptoms he said to look at other symptoms out there. --> fever, rash, encephalitis |
|
|
Dengue fever
|
- not as prevalent in the U.S (mostly in the tropics)
- 4 serotypes... used to be localized, but now b/c of airplanes, spread and enhance the infection against other serotypes (antibody dependent enhancement) - Fever, headache, myalgia, bone ache, (breakbone fever) ***Humans are the only vertebrate reservoir besides monkeys, which play no role in spread |
|
|
ADE
|
In dengue fever...
reinfection with a second serotype results in antibodies from the first infection making the second infection worse - ADE: Antibody Dependent Enhancement of infectivity. |
|
|
prion
|
**Prions are NOT viruses,** they are single proteins found in the nervous system on the surface of neurons in the brain.
Prions contact and induce a normal cellular protein to change shape and to become a prion protein. --> prions are infectious proteins |
|
|
Transmissible Spongiform Encephalopathy (TSE)
|
Spongiform encephalopathy describes the appearance of the vacuolated neurons, as well as their loss of function and the lack of an immune response or inflammation
Vacuolation of the neurons, the formation of amyloid-containing plaques and fibrils, a proliferation and hypertrophy of astrocytes, and the vacuolation of neurons and adjacent glial cells are observed (brain turns spongy/mushy) |
|
|
Bovine spongiform encephalopathy (BSE)
|
Mad Cow Disease
|
|
|
Creutzfeldt-Jakob disease
|
a form of brain damage that leads to a rapid decrease of mental function and movement
Creutzfeldt-Jakob disease in humans can be inherited or infectious - Infection can come from transplants. - Inherited from a mutant protein. |
|
|
Kuru
|
cannibalism - eating human brains - Papua New Guinea
Vacuolization of the gray matter of the brain - progressive disease. Long term - 20 or more years until symptoms. Neurological impairment: anxiety, memory loss, mood changes etc. Movement problems: muscle twitching, spasms. Loss of speech, coma, death. |
|
|
Diagnosis of brain diseases from prions
|
Patients referred due to behavioral changes.
Diagnosis is by protein detection from biopsies or by brain sectioning on autopsy. Prions induce no immune response, so there is no diagnosis by detection of antibodies. ***There is NO treatment. |
|
|
FFI
|
Fatal familial insomnia (prion disease)
|
|
|
GSS
|
Gerstmann-Straussler-Schienker disease (prion disease)
|
|
|
how do you kill a prion?
|
they are pretty much indestructible....
(resistant to UV.. radiation.. ethanol... routine autoclave etc.) you need to treat with 1N NaOH, then autoclave for 4 hours at 132° C |
|
|
Passive immunization
|
Transfer of maternal IgG antibody to the fetus in utero or IgA to the child’s gut from breast milk.
Injection of antibody against the pathogen or toxin. |
|
|
Active immunization
|
Vaccination with an antigen that elicits an immune response prior exposure to pathogen or related pathogen.
|
|
|
What a vaccine does, or can do
|
A vaccine makes the body think it is infected and elicits a memory immune response that is ready to go when a person is exposed to that pathogen.
-Block infection - sterilizing immunity -Block spread in the body or establishment of -chronic infection -Lesson symptoms of infection -Shorten the time of infection -Block the action of toxins (bacteria) -Reduce or eliminate the risk of virus-caused cancers (HBV, HPV) -Reduce opportunity of spread to other individuals lowering the incidence in a population. -Herd immunity. |
|
|
inactivated vaccines
|
took viruses and inactivated it in formaldehyde. It ended up with particles. The virus could not replicate. This is still a popular way of making vaccines. Sometimes there is a purification process after this.
There are limitations to using something passive and dead. There’s not enough of it. The body see’s it and clears it almost immediately Salk Polio vaccine, HAV, influenza. Formalin (formaldehyde) is the most common inactivating agent. |
|
|
attenuated vaccines
|
the virus can lose certain genes, and but it is still able to persist. It replicates in the host, and generates an immune response, but it cannot cause disease.
Sabin Polio Vaccine, Measles, Mumps, Rubella (MMR) VZV, Yellow Fever, Influenza nasal spray (FluMist). |
|
|
subunit vaccines
|
HBV vaccine - make individual proteins from virus.
|
|
|
how many doses do you need for an immune response, regarding vaccines
|
Initial dose doesn’t generate much of a response. The second dose has some slight memory. By the time you get to the third dose you have a bigger response.
|
|
|
Attenuated vs. Inactivated Vaccines
|

|
|
|
Herd immunity
|
Vaccines are usually not 100% effective - some people will not develop a protective immune
response and not all people will receive a vaccine. If enough people are successfully vaccinated, the chain of transmission can be broken and the incidence of infection will drop. the viral reproductive ratio is reduced to <1 (i.e. smallpox no longer exists besides in research labs) |
|
|
Variola virus
|
causes smallpox
- Smallpox has killed more people than any other disease. - Immunization against it was pretty simple. - Jenner discovered that milk maids around cows would get a mild form of cowpox, but they wouldn’t get smallpox. They had immunity. |
|
|
Vaccinia virus
|
causes cowpox, a milder disease that can affect humans and induce cross immunity to smallpox
|
|
|
polio
|
+ssRNA Picorna-virus (Icos capsid & NO envelope)
- Up to 95% of polio infections are asymptomatic but are contagious. - has a primary replication, but this isn’t what causes the disease. - causes a viremia and spreads to the nervous system --> cause destruction of motor neurons, causing temporary or permanent paralysis - Recovery can be incomplete and take up to 2 years. - transmitted fecal-orally. |
|
|
Post-Polio Syndrome (PPS)
|
8-70 years after recovery from paralysis, fatigue, weakness pain in areas involved at the time of acute poliomyelitis. Etiology is not clear.
|
|
|
Inactivated Polio Vaccine (IPV)
|
Formalin used to inactivate virus Requires 3 doses
(from Salk) |
|
|
Live attenuated Oral Polio Vaccine (OPV)
|
1958 Albert Sabin
- strong immunity against all 3 forms of virus - replicates well in gut but not in nervous system - became the vaccine of choice during the control of polio - can revert to disease causing form in rare cases (1/750,000) |
|
|
Adjuvants
|
Adjuvants are agents such as aluminum salts or oil emulsions (e.g. squalene) added to non-live vaccine formulations to boost the immune response
- If you inject the vaccine only, it will get cleared quickly by the immune response. - Adjuvants hold cells and cause irritation. - They are not ALWAYS used – the flu vaccine does not use them. |
|
|
how do adjuvants enhance the immune response?
|
- Hold the antigen in place, allowing a greater length of time for a response and aiding in presentation of antigens to macrophages.
- Stimulate localized inflammatory/innate immune response which recruits T and B cells to the site, thus enhancing the adaptive response. Adjuvants can sometimes allow less antigen to be used in each dose of vaccine, making a limited supply of flu vaccine, for example, be used in more people. (Adjuvants in flu vaccine are used in Europe but not the US.) |
|
|
An HIV vaccine?
|
- Potential or perceived dangers of an attenuated HIV vaccine
- Extreme variability of the virus - high mutation rate - Lack of knowledge about “correlates of protection” - we just don’t know what protective immunity will “look like”. - Lack of good animal models of HIV infection and disease - Political/social issues in testing vaccines in humans - Failure of recent vaccine trials |
|
|
do Koch's postulates apply to caries?
|
NO !!!!
do NOT apply to endogenous bacteria !!! |
|
|
what dictates how the bioflm responds?
|
its the CONDITIONS that dictstes how the biofilm responds
--> the biofilm "adapts" and recruits what it needs to survive |
|
|
in ECC, what part of the triad (diet, bacteria, host) has changed the most?
|
DIET
thus has the most influence in terms of caries/disease |
|
|
the human diet affects caries at two levels:
|
1) Tooth development:
- can be affected by malnutrition and enamel hypoplasia (during perinatal development) - 80% or more in caries is found in 20% of the children, which we DO NOT SEE. (we see the good 80% that has $) - The percent of people living at or below poverty is increasing daily --> associated with increased caries! Pits and grooves formed due to enamel hypoplasia are colonization sites for bacteria early on. (bad b/c poor people eat a lot of sugar) 2) Biofilm metabolism: - Sucrose has a critical role in critical mass formation and lactic acid production |
|
|
T/F
NCD exceeds infectious diseases and cancer as cause of death |
TRUE !
|
|
|
What environmental change in modern humans lead to dental caries?
|
DIET
- refined sugar - texture consistency increased lifespan |
|
|
Which type of polysaccharide can be most quickly catabolized to form energy?
|
glycogen (has a lot of chains)
|
|
|
*** Sucrose is a (monomer / dimer /trimer)
|
dimer --> alpha 1,2 glycosidic bond
|
|
|
*** bond of sucrose
|
dimer --> alpha 1,2 glycosidic bond
|
|
|
Polymers of sugar are held together by _____bonds
|
glycosidic
|
|
|
What was the major source of sweetening food prior to sugar?
|
Honey
|
|
|
What is "sweetness" ?
|
major determinant distinguishing poisonous vs. non-poisonous food
(humans have the most receptors for sweet than any other mammal) |
|
|
Composition of honey is:
|
Composition of honey is mainly fructose and glucose natural preservative (no bacteria grow due to low pH, fructose, glucose)
(only ~1% sucrose) |
|
|
** in order to be pathogenic... a bacteria must:
|
- adhere to specific receptors
- form critical mass ** - invade or elaborate noxious substances |
|
|
Glucosyltransferase (GTF)
|
- extracellular enzyme unique in nature
- most important enzyme in formation of caries “Glucosyl” --> Cleaves the alpha 1,2 bond of sucrose “Transferase” --> transferring the glucose from sucrose to the polymer to make a capsule called mutan & glucan - Mutans streptococci have 3 copies from gene duplication (GTF-b,c,d) - gene duplication occurred over millions of years, and strep mutans is one of about 5 bacteria that can utilize sucrose. - GTF works outside of the bacterial cell and requires no ATP ! Polymer is originally thought to make sticky plaque, but it is actually not crucial to adherence. - Knock out experiments for these genes showed that the bacteria could stick, but they couldn’t form critical mass |
|
|
what is the most important enzyme in formation of caries
|
Glucosyltransferase (GTF)
|
|
|
What is special about glucosyltransferase?
|
GTF works outside of the bacterial cell and requires no ATP !
|
|
|
Why do caries form?
|
Caries is result of the UNIQUE ability of oral streptococci (e.g. strep mutans) to enzymatically cleave the alpha-1,2 glycosidic bond of sucrose.
This enables the organism to perform metabolic work EXTRACELLULARLY, yielding a polymer of glucose and a monosaccharide, fructose. Catabolism to lactic acid via PTS import |
|
|
Caries is result of the _____ ability of oral streptococci (e.g. strep mutans) to enzymatically cleave the_____ bond of sucrose.
This enables the organism to perform metabolic work _____ , yielding a polymer of ___and a monosaccharide, _____. |
Caries is result of the UNIQUE ability of oral streptococci (e.g. strep mutans) to enzymatically cleave the alpha-1,2 glycosidic bond of sucrose.
This enables the organism to perform metabolic work EXTRACELLULARLY, yielding a polymer of glucose and a monosaccharide, fructose. |
|
|
Where can you find glucosyltransferase?
|
ONLY found in mammals with teeth !!
|
|
|
What is the major factor in expression of virulence?
|
SUCROSE !!!
|
|
|
If you were just eating high glucose/fructose and no sucrose, would you be caries free?
|
There is actually sucrose in everything, even plants, so you cannot get away from it.
Pivotal role of sucrose is the alpha 1,2 bond that PROVIDES ENERGY to form capsules extracellularly |
|
|
early infection of HIV
|
- often associated with a mononucleosis-like or flu-like syndrome.
- Many transmissions are not apparent to the infected person. **A fall in CD4 T cell counts always precedes disease. |
|
|
what precedes disease in HIV?
|
A fall in CD4 T cell counts always precedes disease.
|
|
|
HIV-1 vs.HIV-2
|
HIV-1 is what is responsible for the world wide epidemic events
HIV-2 from monkeys --> less pathogenic and less transmissible disease |
|
|
what are the proportion of HIV/AIDS cases amongs adults & adolescents
|
males --> male-to-male sexual contact
females --> high-risk heterosexual contact |
|
|
HIV infection, replication
|
- HIV is present in semen and vaginal secretions.
- Transmission from men to women is twice as efficient as from women to men. - Anal sex and needle sharing are more efficient. *The likelihood of transmission is greatly reduced by the reduction in viral load that results from antiviral treatment. |
|
|
Virology - schematic of HIV
|
- has a Capsid (as all viruses do) - in this case a CONE shaped one --> icosahedron
another capsid is called the matrix - Contains spikes (envelope glycoproteins that usually exist in TRIMERS***) - The virus contains reverse transcriptase - Needs to convert the RNA genome into DNA immediately after entering the cell |
|
|
** spikes are envelope glycoproteins that usually exist in...
|
TRIMERS
|
|
|
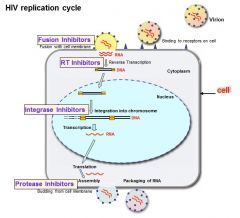
HIV replication cycle
|
|
|
|
protease inhibitors
|
Protease inhibitors are a class of antiviral drugs that are widely used to treat HIV/AIDS and hepatitis caused by hepatitis C virus.
Protease inhibitors prevent viral replication by selectively binding to viral proteases (e.g. HIV-1 protease) and blocking proteolytic cleavage of protein precursors that are necessary for the production of infectious viral particles. |
|
|
Integrase Inhibitors
|
- Integrase inhibitors (also known as integrase strand transfer inhibitors) are a class of antiretroviral drug designed to block the action of integrase, a viral enzyme that inserts the viral genome into the DNA of the host cell.
- Since integration is a vital step in retroviral replication, blocking it can halt further spread of the virus. - Integrase inhibitors were initially developed for the treatment of HIV infection, but they could be applied to other retroviruses. |
|
|
Fusion Inhibitors
|
Entry inhibitors, also known as fusion inhibitors, are a class of antiretroviral drugs, used in combination therapy for the treatment of HIV infection.
--> can inhibit entry of virus with drugs |
|
|
integrase, protease & reverse transcriptase are all coded by ____
|
pol gene
|
|
|
Regulatory genes
|
(everything other than Gag, Pol, and Env)
- controlling the timing of the gene expression neutralizes the intracellular defense systems |
|
|
Overlapping Genes
|
genes stacked on top of one another:
- overlapping sequences that encode for proteins - can start with one nucleotide and get a specific sequence or start on the third and gt something different - stacks genes on top of each other on the same piece of DNA |
|
|
Pol proteins
|
- reverse transcriptase (RT)
- integrase - protease |
|
|
Reverse transcriptase (RT)
|
- RNA-dependent DNA polymerase
- Uses the RNA genome as a template to generate a DNA copy. - RT is carried in the virion. - No proofreading - introduces a lot of mutations* |
|
|
Integrase
|
- integrates the DNA genome into chromosomal DNA. - Carried in the virion.
|
|
|
Provirus
|
an integrated retroviral DNA genome.
|
|
|
Protease
|
- During virus budding protease cleaves the immature Gag polyprotein into subunits.
- Necessary for virus maturation* |
|
|
Many viral proteins are generated first as _____ which are then cleaved by cellular or viral proteases during maturation.
|
polyproteins
|
|
|
Protease inhibitor drug
|
- the virus can still be expelled but it will not have its normal infective properties.
***If virus cannot cleave the GAG proteins, the virions are NON-INFECTIOUS |
|
|
HIV envelope protein binds to:
|
Primary receptor: CD4 - initial adhesion of virus to cell
Co-receptors: CCR5 or CXCR4 - triggers the fusion between virus and cell |
|
|
CXCR4
|
HIV Co-receptor on CD4 T cell
|
|
|
CCR5
|
HIV co-receptor on macrophages
|
|
|
HIV Infection
|
Activated CD4+ T cells - these cells make most of the virus
HIV replicates in activated CD4+ T cells (metabolically active) Resting CD4+ T cells - these are few but are often latently infected and cannot currently be eliminated. If a patient stops HAART, virus from these cells will begin replicating. Macrophages - can be persistently infected for long periods and apparently don’t die from infection, though their function is impaired. |
|
|
If a patient stops HAART, virus from what cells will begin replicating.
|
resting CD4+ T-cells
|
|
|
Activated CD4+ T cells
|
- these cells make most of the virus
-HIV replicates in activated CD4+ T cells (metabolically active) |
|
|
Resting CD4+ T cells
|
- these are few but are often latently infected
and cannot currently be eliminated. - If a patient stops HAART, virus from these cells will begin replicating. |
|
|
HIV infecting Macrophages
|
- can be persistently infected for long periods and apparently don’t die from infection, though their function is impaired.
|
|
|
Viral load trend in HIV
|
Since HIV infects T cells right at the site of transmission, and these cell migrate to lymph nodes and spread virus quickly, there is no classical primary and secondary viremia.
Viral load increases exponentially early in infection. |
|
|
increase in viral load of HIV
|
Exponential increase in virus
- this happens first 1 ~ 2 week - Acute Phase of infection - viral titers can be as high as 10 million viral particles per cubic mm of blood After ~2 weeks, adaptive immunity starts to kick in 1. Cytotoxic T cells can kill the virus 2. Because HIV are using up a lot of the CD4 T cells (their primary site for replication) → reasons why the viral load decreases at this point initially |
|
|
set point of HIV
|
SET POINT:
- viral load decrease; hence you feel OK at this point - No more acute syndromes; they feel healthy, hence the reason why it spread worldwide - Antibodies take a long time to develop - Regardless of feeling okay, CD4 T cells are continuously declining due to infection - takes about 10 years before you develop AIDs and other opportunistic infection. - what kills you is not the infection of AIDs but the opportunistic infection |
|
|
HAART
|
- multiple drug combination; decreased in epidemics
- If you stop the drugs, the viral load goes back up again - Antibody Production: lags behind the infection sometimes you miss the diagnosis |
|
|
Diagnosis of HIV infection
|
1) Primary screen
- if this comes back bad then you do a confirmatory test - sensitive test - b/c you dont want to miss anyone only flaw is that you may get a false positive Hence you do a confirmatory test if diagnosed as positive in the primary screen 2) confirmatory test - if you get positive you come back for a confirmatory test (this wont give a false positive). |
|
|
detecting HIV
|
These tests depend on detecting antibodies
- Western blot is how we confirm the disease - ELISA just tells us we have antibodies that react with something - problem is - when first infected, it takes a few weeks to produce antibodies - so results can be -misinterpreted - There are home tests that use saliva (some antibody can be found in saliva) = OraQuick |
|
|
What is the best way to test for HIV?
|
Viral RNA (RT-PCR) most sensitive way to test is detect nucleic acid itself
- used primarily to screen blood supply - also to measure viral load and to detect recent infection - this is superior way to test |
|
|
Characteristics of Immunodeficiency
|
The immune system mounts a strong response to HIV but fails to:
- prevent continued viral replication - ongoing development of immunodeficiency: Progressive loss of CD4+ T cells Progressive accumulation of functional defects in all aspects of immunity - CD4 T cells - CD8 T cells - macrophages - chronic inflammatory response markers - improper cytokine levels |
|
|
The immune system mounts a strong response to HIV but fails to:
|
- prevent continued viral replication
- ongoing development of immunodeficiency: |
|
|
Oral AIDS defining illnesses
|
- Oral/esophageal candidiasis (thrush)
- Oral hairy leukoplakia (OHL) - Kaposi's sarcoma (KS) |
|
|
Oral Lesions Associated with HIV Infection
|

|
|
|
HIV Antiviral Therapy
|
HAART - Highly Active Antiretroviral Therapy
A combination of antiviral drugs targeting two or more stages in the viral replication cycle. Reverse transcriptase inhibitor(s) + protease inhibitors(s) Recently added - integrase inhibitors, fusion inhibitors The introduction of HAART in the mid 1990’s allowed HIV+ people to survive for a normal life span in many cases. |
|
|
HIV-1 variability
|
- Reverse transcriptase has no proofreading activity
- Error rate of cellular DNA polymerases is ~10-8-1011 errors per nucleotide added to the newly formed viral DNA Error rate of RT is ~3x10-5 - This means that antibodies and T cells stop recognizing the virus and new antibodies and T cells must be created constantly. There is more HIV-1 genetic variability in a single person after 3 years than there is in all of the flu viruses in the world. HIV also develops antiviral drug resistance. |
|
|
HIV latency
|
HIV-1 replicates best in activated T cells.
When HIV is integrated in a resting T cell, viral transcription often fails, and no viral proteins are made. Resting T cells last for many years with latent HIV in them. CTL cannot recognize the infection in the cell and cannot kill the latently infected cell - just as for herpesviruses. **Antiviral drugs cannot eliminate latently infected cells |
|
|
Where does HIV replicate best?
|
HIV-1 replicates best in activated T cells.
When HIV is integrated in a resting T cell, viral transcription often fails, and no viral proteins are made. Resting T cells last for many years with latent HIV in them. CTL cannot recognize the infection in the cell and cannot kill the latently infected cell - just as for herpesviruses. **Antiviral drugs cannot eliminate latently infected cells |
|
|
T/F: Antiviral drugs cannot eliminate latently infected cells
|
TRUE
|

