![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
45 Cards in this Set
- Front
- Back
|
How are fungi classified?
|
>Fungi are Eukaryotes:
- sharing some characteristics with plants (and animals) - possess their own kingdom >Broadly divided into: YEASTS: - unicellular - budding organisms - e.g. Candida Albicans / Cryptococcus Neoformans MOULDS: - Organisms with branching hyphae - e.g. Aspergillus fumigatus / Tricophyton Rubrum DIMORPHIC FUNGI: - Some species capable of displaying both morphologies in response to environmental triggers - e.g. Histoplasma capsulatum / penicillium fungi |
|
|
Describe the growth characteristics of fungi.
|
>Slow growing in the lab (days to weeks)
>Able to assimilate many different substrates, act as scavengers in the environment - important in recycling biomaterial - invasive species need to be able to grow at 37 degrees C but many grow at environmental temperatures |
|
|
What is the burden of fungal infection?
|
>Superficial and mucosal infections are very common
- 10% of population will suffer dermatophyte infection (ringworm - skin/scalp/nails) - 75% women episode of vulvovaginal candidiasis during lifetime >Endemic or pathogenic fung causing invasive disease in immunocompetent hosts are restricted to certain parts of the world - UK cases are caused from exposure elsewhere |
|
|
What are the big five causes of fungal infection?
|
- Candida (esp. Albicans)
- Aspergillus (esp. Fumigatus) - Pneumocystis Jirovecii - Cryptococcus Neoformans - Zygomycete species (esp. Rhizopus arrhizus) |
|
|
Describe the characteristics of yeasts.
|
>Unicellular organisms
>Reproduce via budding >Generally round or oval - form pseudomycelium under certain conditions >Medically important are candida and cryptococcus |
|
|
Describe the characteristics of Candida.
|
>Principal pathogen is C. Albicans
- Tropicalis, Parapsilosis, Glabrata and Krusei also crop up occasionally >Small numbers may be found in mouth, GI and genital tract without causing infection - Larger numbers during or following broad spectrum antibiotic therapy - Risk of superficial/systemic candidiasis >Opportunistic infection - occurs in immunosuppressed patients, broad spectrum antibiotic patients or extremes in age - more common in diabetics, pregnant patients, steroid patients (e.g. asthmatics) >Site of infection: - Cutaneous candidiasis occurs particularly in moist skin - Candidemia (blood infection) seen in TPN patients / drug abusers - Recurrent oropharyngeal candidiasis infrequently encountered in normal healthy adults (should raise possibility of underlying disease / immunosuppression) - Often commensal in origin, but cross infection occurs in healthcare setting >Diagnosed via visualisation of yeast cells - Can be grown on most agar 48-72h - Saburaud's medium used to inhibit bacterial growth - Chromogenic media available to differentiate species - Rapid test - germ tube test (hyphae produced in human serum after incubation for 2-3 hours in human serum) TREATMENT: >Superficial infection: topical antifungals, or oral systemic therapy may be required for highly immunosuppressed patients (and nail infections - prolonged treatment required) - Imidazoles (clotrimazole), polyenes (nystatin, amphotericin B) >Systemic: - Imidazoles (fluconazole, itraconazole, voriconazole) - Polyenes can be used as oral suspensions for treatment of oropharyngeal candidiasis - IV drugs include amphotericin B, flucytosine, caspofungin, imidazoles |
|
|
Describe the characteristics of Cryptococcus neoformans.
|
>Encapsulated yeast
>Found in dried pigeon droppings or contaminated soil - inhaled into lungs >Opportunistic infection - occurs in immunocompromised patients, particularly those with HIV >Patients present with meningitis (acute or chronic), +/- pulmonary signs - Can occur in skin, eyes and musculoskeletal system (via haematogenous spread) >Diagnosed via CSF / blood stain (india ink) - Cultures take up to 10 days - Latex agglutination can be used >High mortality >Treated with high dose systemic anti fungal drugs >Combination of amphotericin B or fluconazole + flucytosine for 4-6 weeks - Recurrent infection common in HIV+, maintenance therapy of oral fluconazole may be given |
|
|
What is Malassezia furfur?
|
>Lipophilic commensal yeast
>Cause of common pityriasis versicolor - disfiguring skin condition with development of numerous brown scaly patches - hypo pigmentation of skin - Treat with topical anti fungal or oral itraconazole >May cause central venous catheter associated fungemia (in patients receiving fat emulsions) |
|
|
What is Trichosporum beigelii?
|
>Causes mild infection of hair in tropical countries (white piedra)
>Rare opportunistic infection in immunosuppressive disease e.g. leukaemia, causing disseminated infection |
|
|
Describe the characteristics of Aspergillus.
|
>Abundant in environment
>Airborne spores common, infections follow inhalation of Aspergillus >Several species can cause infection: - fumigatus - niger - flavus >Risk factors = immunosuppression (e.g. bone marrow transplant recipients) >Outbreaks occur during building demolition or construction occurs in vicinity of high risk units, releasing aspergillus spores >Infections: ALLERGIC ASPERGILLOSIS: - Uncommon condition caused by hypersensitivity to inhalation of aspergillus spots - Asthma-like symptoms, mucus plug formation, Farmer's lung ASPERGILLOMA: - Fungus ball occurring in patients with lung cavities (result of TB) - Patients may be asymptomatic or have cough / malaise INVASIVE PULMONARY ASPERGILLOSIS - Rapidly progressive and life threatening - Highly immunosuppressed patients - Persistent fever, shortness of breath and pleuritic chest pain - Cause widespread necrosis and hemoptysis - Haematogenous spread >Diagnosed via Aspergillus precipitins in serum (Ab test) - Difficult in immunosuppressed as immune response not mounted - Treatment sometimes given on empiric basis - Radiologic investigation may be used (e.g. CT) >Definitive diagnosis ONLY by HISTOLOGICAL DETECTION OR CULTURE >Treatment: - Allergic aspergillosis: steroids - Aspergillomas: surgical excision / installation of antifungals - Invasive Aspergillosis: high dose systemic antifungal therapy NB. Prophylaxis may be used for at risk patients e.g. HEPA filtered positive pressure rooms, itraconazole. |
|
|
Describe the characteristics of mucorales.
|
>Group of moulds causing a variety of infections called mucormycosis (or zygomycosis)
- Rhizopus - Rhizomucor - Absidia >Infection caused by spore inhalation or inoculation >Risk factors: - Diabetes - Immunosuppression - Burns >Common infection 'rhinocerebral mucormycosis' - starts paranasal sinuses - spreads to eye, palate and brain >Diagnosed by clinical, radiological and histological features (showing browad nonseptate hyphae within tissue) >Fungus can be grown occasionally from clinical specimen >Treatment by resection of necrotic tissue / high dose antifungal therapy - High mortality |
|
|
Describe the characteristics of dermatophytes.
|
>Filamentous fungi commonly causing superficial infection of skin, nails and hair:
- tinea / ringworm (skin/hair) - onychomycosis (nails) >Clinical diagnosis by microscopy and fungal culture >Treatment with topical anti fungal preparations - systemically for nail and hair |
|
|
What are dimorphic fungi? Which diseases are dimorphic fungi associated with?
|
>Exhibit mycelial growth at 22C but form yeasts at 35-37C
SPOROTRICHOSIS: >Infection of subcut. tissue with Sporothrix Shenckii - Arms hands after inoculation injury >Histoplasma capsulatum (causes histoplasmosis) - Mild self-limiting chest infection - Chronic pulmonary infection (resembling TB) can occur in immunosuppressed) >Reservoir - bird or bat droppings COCCIDIOIDES IMMITIS: >Soil fungus found in SW USA, Central and South America - Inhalation of airborne spores can cause asymptomatic pulmonary infection - Occasionally chronic pulmonary or disseminated disease occur |
|
|
What is pneumocystis jirovecii?
|
>Found worldwide, natural reservoir unknown.
>Humans exposed via airborne route - Infection normally only occurs in patients with depressed cell mediated immunity (e.g. HIV infection) >Principally causes PCP >AIDS defining illness in HIV+ patients >Other patients include bone marrow and solid organ transplant recipients Lab diagnosis is by microscopic exam of sputum or broncho-alveolar lavage fluid (using immunofluorescence) >Treatment principally with high dose trimethoprim sulfamethoxazole |
|
|
Describe the characteristics of moulds.
|
>Or filamentous fungi
>Group of saprophytic (feeds on dead matter) eukaryotic organisms >Form mycelia in vegetative state >Many moulds found in the environment, few capable of causing human disease >Important filamentous fungi causing human infection: - Aspergillus - Mucorales - Dermatophytes |
|
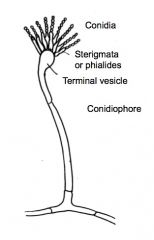
Identify this fungus.
|
>Aspergillus fumigatus
|
|
|
Identify this fungus.
|
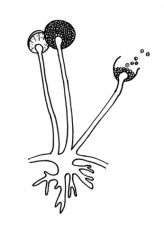
Rhizopus
|
|
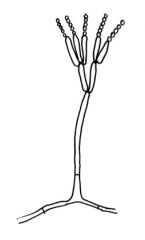
Identify this fungus.
|
Penicillium
|
|
|
What are the three forms of asexual spore?
|
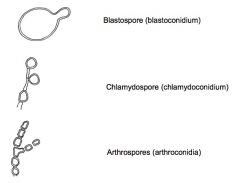
|
|
|
Describe the basic nomenclature of fungi.
|

|
|
|
Describe the structure of the fungal cell wall.
|
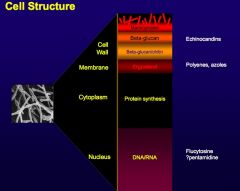
>Cell membrane contains ergosterol as the main sterol (c.f. cholesterol in mammalian cell membrane)
>Cell wall consists of several polysaccharides (glucans, manna's), proteins and chitin >Some fungi have melanin in the cell wall >Some fungi have a polysaccharide capsule e.g. Cryptococcus neoformans |
|
|
What is unusual about candida opthalmitis?
|
It lights up in the retina.
|
|
|
Define parasitism.
|
The activity of an organism that spends any portion of its life in direct contact with a host species at the expense of the host.
>Protozoa: - exist in all body compartments - intra and extracellular - cause a spectrum of disease (e.g. malaria, presents with symptoms such as diarrhoea and blastocystis) >Helminths: - multicellular - highly organised - complex lifecycles |
|
|
Describe the burden of parasitic disease.
|
>Parasites cause chronic invasive illnesses
- often overlooked - affect people's daily lives - prelude to worse disease >Parasites are associated more with DALYs (disability adjusted life years) - significantly impact society as people's contribution is affected >Due to parasite coevolution with man; not in the parasite's interest to kill the host >Malaria an exception - causes a significant number of deaths annually in developing world |
|
|
How do parasites tend to be transmitted?
|
>Environmental / behavioural:
- Associated with resistant cyst or ova (survives in the environment) - e.g. Giardia, Toxoplasma, Tapeworms, geohelminths; Trichomonas vaginalis directness of contact precludes need for cyst formation >Consumption of resistant stages with food - e.g. tissue cyst of toxoplasma >Direct invasion - e.g. schistosomes and hookworms invade host via the skin >Via insect vectors PROTOZOA - E.g. Malaria (Anopheles mosquito; interestingly can be infected with fungus as a means of controlling spread)) - Leishmania (Sandflies) - Trypanosomes (African = Tsetse fly, American = Triatomid bugs) HELMINTHS - FILIARIASIS - Blood sucking flies Onchocerca - Simulium blackflies Loa Loa - Chysops Wucheria bancrofti - Culex, Anopheles and Aedes Brugia malayi - Mansonia |
|
|
What are the typical mechanisms of parasite pathogenesis?
|
>Disruption of normal physiological function:
- e.g. Giardia deconjugates bile salts causing malabsorption and consequent steatorrhea >Invasion of host tissues: - Disruption of metabolism: trypanosome induced cardiac failure - Disruption of host immune responses e.g. Toxoplasma and Leishmania invade macrophages - Physical disruption e.g. granuloma formation leading to necrosis >Physical presence - Plasomodium aggregation in cerebral malaria, Ascaris blockage of gut (foot long worm, between 10 and 100 will physically obstruct the gut) >Induction of immune responses: - Leishmania lesions associated with protective immune responses - Toxoplasma encephalitis associated with cyst reactivation - Schistosome granuloma formation |
|
|
Give five examples of protozoa and their common hosts/route of transmission.
|
1. Malaria (Anopheles mosquito, bite)
2. Trichomonas vaginalis (Sexually transmitted) 3. Trypanosomiasis (Tsetse fly = Africa, Triatomine bug = USA, bite) 4. Leishmaniasis (Sandflies, bite) 5. Toxoplasmosis (Domestic cat, oral) |
|
|
What are the 4 main species of malaria?
|
Plasmodium...
- ...falciparum (most deaths, subsaharan Africa, S.E. Asia, S/C America) - ...vivax - ...ovale - ...malaria |
|
|
What is the epidemiology of malaria?
|
- Tropical disease
- 40% of world's population, mostly those living in the poorest countries, are at risk of malaria. - 2.5 billion are at risk - >500 million become severely ill with malaria each year - >1 million die from malaria - Africa: - 20% childhood deaths - African child has on average between 1.6 and 5.4 episodes of malaria fever each year - Every 30 seconds a child dies from malaria |
|
|
Give an overview of Toxoplasmosis.
|
>Toxoplasma gondii
>Obligate intracellular parasite (apicomplex) >Sexual cycle only occurs in cats but all vertebrates are susceptible >Non-feline hosts 2 critical phases of infection - Acute flu like disease - Establishment of chronic latent cysts >UK seropositivity 30-40% (60% in France due to rare lamb etc.) >Reactivation of cysts associated with immunosuppression; HIV or transplantation - AIDS defining illness >Risk of congenital transmission during pregnancy - spontaneous abortion / adolescent eye disease |
|
|
Give an overview of Trichomonas.
|
>3 species:
- T. hominis (caecum / large intestine - T. Tenax (mouth) - T. Vaginalis (vagina, urethra, seminal vesicles and prostate) >T. vaginalis results in inflammation and discharge and affects ~180 million women |
|
|
Give an overview of Trypanosomiasis.
|
African vs. South and central American
>Trypanosoma cruzi - S. American - Intracellular; macrophages, muscle and nerve cells - Chagas disease (common in Southern and Central America) - Cardiac failure (hypertrophy) - Loss of nervous control of gut >Trypanosoma brucei - 2 sub species - T.b. Gambiense - T.b. Rhodesiense SYMPTOMS: >Fever, malaise, anorexia; invasion of CNS results in sleeping sickness phase of disease >Both sub-species demonstrate variable surface coats associated with avoidance of host immune response - Variable surface glycoproteins >Treatment = antibiotics which are toxic to the host |
|
|
Give an overview of Leishmaniasis.
|
>Multiple species
>Cutaneous diseases, deeper tissue may be implicated >Old World vs. New World >L. donovanii (OW) - Most severe form Kala azar >Simple cutaneous lesion localises at the site of the bite resulting in a granulomatous response >Epidermis fragile and prone to further physical damage, ulceration and secondary infection NB. Many Africans self inoculate with Leishmania and may be unsuccessful. |
|
|
Describe the pathogenesis of Leishmaniasis.
|
>Insect takes a blood meal and injects protozoa
>Protozoa invades macrophages >Immune response leads to granulomatous reaction and fragile skin >Patients prone to secondary bacterial infections |
|
|
What classes of worm are there?
|
>2 groups:
- Platyhelminthes or 'flatworms' - Cestodes; tapeworms - Digeneans; flukes - Nematodes or 'roundworms' |
|
|
Give an overview of Cestodes.
|
>Complex parasites, invade tissues, immune responses to larval stages
>Pathogenesis can be classified by lifecycle stage >Larval cestodiasis - Larvae in organs results in disease - Spirometra spp. Invasion of deep tissues - Taenia solium cysticercosis, invasion of range of tissue but predilection for brain (may cause epilepsy) - Echinococcus granulosus, hydatid disease (cysts cannot be penetrated by drugs, full of larvae), liver and lung infections >Humans not obligate hosts, heavy infections are found in communities with close contact to reservoir species |
|
|
What are Digeneans?
|
>Flutelike worms
- Flattened oral sucker, ventral sucker >Alternate asexual and sexual cycles between molluscan and vertebrate hosts >6000spp. ~12 significant in man >Human infective stage is the cercariae which emerges from the snail >Swimmers itch |
|
|
What is Schistosomiasis?
|
>Occurs in the rural tropics:
- S. Mansoni (intestinal) - S. Haematobium (urinary) - S. Japonicum (intestinal) - S. Intercalatum (intestinal) >Located in the lumen of blood vessels >Female permanently in ventral groove of male >Adaptations to evasion of host immunity >Pathology associated with granulomatous lesions |
|
|
What are Nematodes?
|
>Free living and parasitic
>Egg-L1-L4 adult >Resistant cuticle >Multi organ systems >Broad classification - Intestinal - Filarial - others |
|
|
What is Filariasis and a potential pathology in humans?
|
>Long lived roundworm
>Requires larval passage through insect vector >4 major species - Lymphatic disease (Wucheria bancrofti, Brugia malayi) - Blindness (Onchocerca volvulus, Loa loa) LYMPHATIC FILARIASIS: >Adults: afferent lymphatics >Juveniles: blood dwelling, sheathed micro filariae >Pathology associated with adults: - Inflammation and immune responses to worms - Lymphatic inflammation, pain, fever - Elephantiasis (chronic lymphodaema, fibrous infiltration, thickening of the skin) |
|
|
What are two examples of intestinal nematodes?
|
>Ascaris lumbricoides
>Hookworms - Ancyclostoma duodenale - Necator americanus |
|
|
What is onchoceriasis?
|
>Causes river blindness / onchodermatitis
- Result due to immune response to microfilariae - Unsheathed microfilariae found in skin leading to nodular formation - Skin changes; increased pigmentation, loss of elasticity, hanging groin, pouches under eye - High vector density with 30% blindness >Immune response to treatment = Mazotti reaction |
|
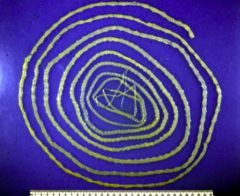
Identify this microbe and describe its characteristics.
|
>Taenia Saginata
- beef tapeworm - found in lumen of small intestine - 5-20m long - 60M cases world-wide - competes for nutrients and space! |
|

Identify this microbe and its characteristics.
|
>Taenia solium scolex
- pork tapeworm - found in small intestine - disease associated with nutrient competition and physical blockage |
|

Identify this disease and its cause.
|
Elephantiasis; filariasis (nematode / round worm)
|

