![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
How can viruses indirectly cause cancer?
|
- Chronic infection (e.g., Hepatitis B and C) cause cirrhosis, inflammation, tissue damage, high levels of cell division
- Cycle vastly increases probability that hepatocytes develop mutations and chromosomal aberrations that derail their "growth control" |
|
|
How can viruses directly cause cancer?
|
- E.g., Papillomavirus
- Upon infection, some DNA viruses stimulate cells to enter S phase of cell cycle and ready themselves for DNA synthesis - Virus needs this for replication - If virus does not complete lifecycle and kill infected cell then the same viral proteins can continue to direct cell to override normal controls on cell growth - Inappropriate division |
|
|
What kind of cancer are Hepatitis B and C associated with? What kind of viruses are they?
|
- Hepatocellular Carcinoma
- Hep B = hepadnavirus - Hep C = flavivirus |
|
|
What kind of cancer are herpesvirus associated with? What viruses specifically?
|
- Lymphoma; nasopharyngeal carcinoma (EBV)
- Kaposi's sarcoma KSHV (HHV8) |
|
|
What kind of cancer is lentivirus associated with? What virus specifically?
|
- Adult T cell leukemia
- HTLV1 |
|
|
What kind of cancer are papillomavirus associated with? What viruses specifically?
|
- Cervical cancer
- Head and neck cancer - HPV |
|
|
What kind of cancer is Merkel cell polyoma virus (MCPyV) associated with?
|
Merkel Cell Carcinoma - aggressive skin cancer (in elderly and immunosuppressed patients)
|
|
|
How was it discovered that viruses were associated with cancer?
|
Observation that a particular cancer is more common in immunosuppressed individuals
|
|
|
Human Papillomavirus (HPV) is a member of what viral family?
|

Papovavirus
|
|
|
What do Papillomaviruses infect?
|
- Cutaneous and mucosal epithelia
- Hands, feet (warts) - Anogenital tract |
|
|
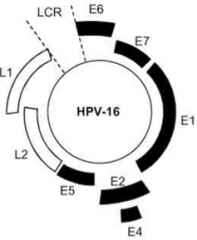
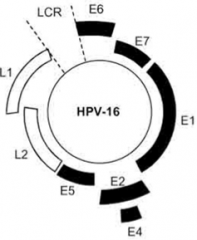
What is the genome of Papillomaviruses?
|

Small, circular, dsDNA
|
|
|
How many subtypes of Papillomaviruses are there? Notable group of subtypes?
|
~100
1/3 infect genital tract - sexually transmitted |
|
|
What genes do the Papillomaviruses encode? Functions?
|
- Early (E) and Late (L) genes:
- E1 and E2 - mediate replication and transcription of viral DNA - E4 - disrupts cytokeratins to facilitate virus exit - E5 - stimulates constitutive growth factor receptor signaling - E6 and E7 - neutralize major "brakes" that regulate cell cycle (p53 and Rb), uncoupling cell division from regulatory controls - L1 and L2 - capsid proteins |
|
|
Which Papillomavirus genes mediate replication and transcription of viral DNA?
|
E1 and E2
|
|
|
Which Papillomavirus gene disrupts cytokeratins to facilitate virus exit?
|
E4
|
|
|
Which Papillomavirus gene stimulates constitutive growth factor receptor signaling?
|
E5
|
|
|
Which Papillomavirus genes neutralize major "brakes" that regulate cell cycle (p53 and Rb), uncoupling cell division from regulatory controls?
|
E6 and E7
|
|
|
Which Papillomavirus genes form capsid proteins?
|
L1 and L2
|
|
|
Which Papillomavirus genes intersect with key elements of cellular growth control, and are associated with oncogenesis?
|
E5, E6, and E7
- E5 - stimulates constitutive growth factor receptor signaling - E6 and E7 - neutralize major "brakes" that regulate cell cycle (p53 and Rb), uncoupling cell division from regulatory controls |
|
|
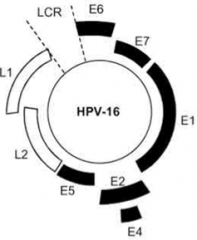
What is the course of a Papillomavirus infection?
|
Papillomavirus -->
inoculation of epithelium (hand, foot, throat, or cervix) --> local multiplication --> wart --> resolution (latency) or cell transformation |
|
|
How does Papillomavirus inoculate the epithelium?
|
Enters through a microabrasion / break in the skin
|
|
|
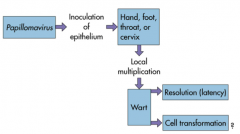
What is the life cycle of Papillomavirus tied to?
|
Differentiation state of the keratinocytes
|
|
|
How does the gene expression / lifecycle of Papillomavirus relate to the keratinocytes?
|
- Virus enters through break in skin to level of Dermis
- Begins early gene expression (E1, E2, E6, E7) in Stratum Basale and Spinosum - Late gene expression and viral genome amplification in Stratum Spinosum and Granulosum - Virion assembly and release in Stratum Granulosum and Corneum |
|
|
What does Human Papillomavirus (HPV) stimulate? Where? How does this differ from normal?
|
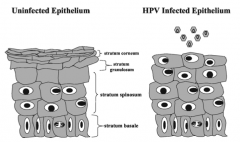
- Stimulation of cell cycle
- Causes cells in statrum spinosum to replicate - Normally only stratum basale cells replicate |
|
|
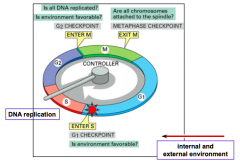
What are the stages of the cell cycle?
|
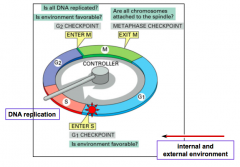
- G1
- S (DNA replication) - G2 - M |
|
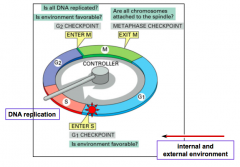
What controls the movement through the stages of the cell cycle?
|
- Cyclin dependent kinases (CDKs)
- Move cell cycle ahead by phosphorylating key substrates |
|
|
What regulates the cyclin dependent kinases (CDKs)?
|
- Temporally regulated synthesis
- Proteasome-mediated degradation of cyclin subunits - Stimulatory and inhibitory phosphorylation events - Stoichiometric inhibitors |
|
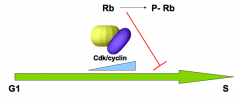
What is the "brake" that blocks progression into S phase? How is it regulated?
|
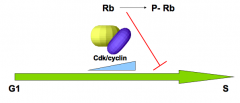
- Rb protein (Retinoblastoma)
- When sufficient Cdk/cyclin has accumulated in G1, Rb becomes phosphorylated and inactivated, cell can move into S phase |
|
|
What protein from Papillomavirus affects the Rb protein? How?
|
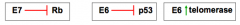
E7 protein binds to Rb and prevents it from blocking the progression to S phase (removes a key regulator of cell cycle progression)
|
|
|
When there is inappropriate entry into the cell cycle, what should happen?
|
Activation of the p53 protein - "guardian of the genome"
|
|
|
What is the role of p53?
|
- Activated by inappropriate entry into the cell cycle
- "Guardian of the genome" - Induces production of Cdk/cyclin inhibitors to stop cell cycle - Major inducer of apoptosis - Stops and weeds out cells that are dividing inappropriately |
|
|
What protein from Papillomavirus affects the p53 protein? How?
|
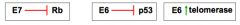
E6 protein recruits a ubiquitin ligase that targets p53 for degradation, thereby preventing it from blocking the progression to S phase or inducing apoptosis; E6 removes a key regulator of cell "accuracy"
|
|
|
What protein from Papillomavirus affects the telomeres? How?
|
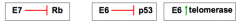
E6 protein induces the expression of telomerase, which enables cells to maintain their chromosomal telomeres and avoid senescence; E6 therefore induces a key component of cellular immortality
|
|
|
What data supports the hypothesis that HPV causes cervical cancer?
|
- Sexually active populations have a higher risk of cervical cancer
- Sexually inactive populations have an extremely low risk of cervical cancer - Greater than 99% of all cervical cancer specimens show evidence of infection with "high risk" strains of HPV (16, 18, 6, and 11) - Low risk strains are associated with warts - Correlation between "high risk" strains and activity of E6 and E7 proteins --> immortalize keratinocytes |
|
|
What kind of proteins are p53 and Rb?
|
"Tumor suppressor genes" - their loss or inactivation causes a predisposition to cancer formation
|
|
|
What percentage of human cancers have a mutated p53?
|
>50%
|
|
|
What happens to the viral DNA from Papillomavirus in the earlier stages of acute and persistent infection?
|
Maintained as an episome (genetic element that can replicate independently of the host and also in association with a chromosome with which it becomes integrated)
|
|
|
What happens to the viral DNA from Papillomavirus during the development of carcionma?
|
- Associated with the integration of the DNA into the host chromosome; E6 and E7 always retained in cancer cells
- Integration disrupts expression of E2 gene, which is a transcriptional repressor and allows increased levels of E6 and E7 expression - Replication of integrated DNA triggers DNA amplifications and chromosomal abnormalities |
|
|
What is a key step towards oncogenesis of HPV infection?
|

Genome integration
|
|
|
What is the cytological progression of HPV-induced lesions?
|
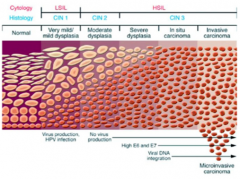
- Normal <-->
- Infection <--> - LSIL (Low grade Squamous Intraepithelial Lesion) <--> - HSIL (High grade Squamous Intraepithelial Lesion) --> - Cervical Cancer (doesn't always progress) |
|
|
What is the histological progression of HPV-induced lesions?
|
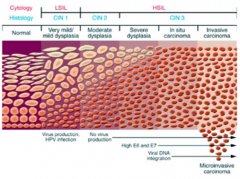
CIN-1 --> CIN-2 --> CIN-3
(CIN = Cervical Intraepithelial Neoplasia) |
|
|
What kind of lesion occurs during a productive infection?
|
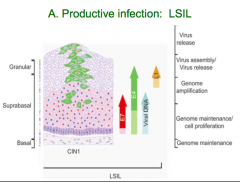
LSIL - Low grade squamous intraepithelial lesion
|
|
|
What kind of lesion occurs during cellular gene deregulation?
|
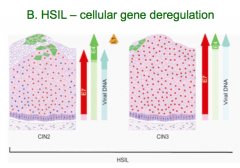
HSIL - High grade squamous intraepithelial lesion
|
|
|
What kind of lesion occurs with DNA integration and breaks in basal membrane?
|
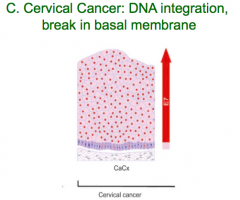
Cervical Cancer
|
|
|
What immune, environmental, genetic, and life-style choices impact the outcome of HPV infection?
|
- Host immune response involved in initial infection of HPV
- Smoking, Oral contraceptive use, viral-load, and coinfections determine conversion from Low grade to High grade squamous intraepithelial lesion - Viral integration and methylation determines conversion from HSIL to cervical cancer |
|
|
What are some markers of the progression from a normal cervix --> HPV infection --> LGIL --> HGIL --> cervical cancer?
|
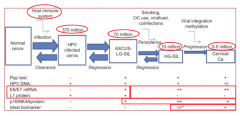
- Pap test: (-) for HPV infection; (+) for LSIL, HSIL, and CC
- E6/E7 mRNA: (-) for HPV infection; (+) for LSIL, HSIL, and CC - L1 protein: (+) for HPV infection and LSIL; (-) for HSIL and CC |
|
|
What diagnostic tests are used for CIN1, CIN2, and cervical cancer?
|
- Pap Smear
- Hybrid Capture Assay for HPV DNA |
|
|
What are you looking for on a pap smear?
|
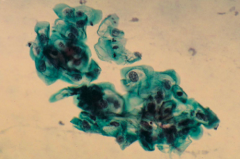
- Cytological evidence of displasia or neoplasia; detection of koilocytotic cells (vacuolated cytoplasm) which are rounded and appear in clumps
- Odd looking cells (easy to miss and easy to get false positive) |
|
|
What is done if there is an abnormal pap smear?
|
Hybrid Capture Assay - for detection, strain analysis, and quantification of HPV DNA
|
|
|
What are the steps of the Hybrid Capture Assay for detection, strain analysis, and quantification of HPV DNA
|
1. Release nucleic acids - by combination w/ base solution (releases target DNA)
2. Hybridize RNA probe w/ target DNA - creates RNA:DNA hybrids 3. Capture hybrids - onto solid phase coated w/ universal capture antibodies specific for RNA:DNA hybrids 4. Label for detection - conjugated to alkaline phosphatase; signal can be amplified >3000-fold 5. Detect, read, and interpret results - substrate produces light that is measured on luminometer in Relative Light Units (RLUs) |
|
|
What are the issues with making an effective vaccine that would prevent genital infection with high-risk strains of HPV?
|
- Need for mucosal infection due to route of infection
- Need to recognize multiple high risk strains - Administration of a vaccine that included "oncogenes" not possible - Societal issues - is this to prevent cancer or STD? |
|
|
What protein from HPV is utilized in vaccines? How does it work?
|
- Capsid protein L1 induces productive humoral immunity
- Recombinant L1 can be produced in culture (insect cells or yeast) - L1 self-assembles into "VLPs - virus like particles" that resemble virions and induce appropriate immunological response |
|
|
What is the effect of the HPV vaccine that contains purified "VLPs - virus like proteins"?
|
- Induces protective, humoral immunity
- Antibodies present at mucosal surface prevent incoming HPV from establishing infection |
|
|
When was HPV discovered? When was HPV proposed as a necessary cause of cervical cancer? When was the vaccine licensed?
|
- Discovered in 1982
- HPV --> cervical cancer in 1999 - Vaccine (Gardasil) licensed in 1008 |
|
|
What strains of HPV cause cervical cancer?
|
Types 6, 11, 16, and 18
|

